| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://jocmr.elmerjournals.com |
Original Article
Volume 17, Number 3, March 2025, pages 145-152
Effect of Ascorbic Acid on the Incidence of Postoperative Delirium Among Elderly Patients Undergoing Cardiovascular Surgery: A Pilot Study
Yusuke Iizukaa, Kentaro Fukanoa, d, Sayaka Okia, Ikumi Sawadaa, Keika Miyazawaa, Shohei Onoa, Koichi Yoshinagab, Masamitsu Sanuib, Atsushi Yamaguchic
aDepartment of Anesthesiology and Critical Care Medicine, Saitama Medical Center, Jichi Medical University, Saitama City, Saitama 330-8503, Japan
bDepartment of Anesthesiology and Critical Care Medicine, Jichi Medical University, Shimotsuke City, Tochigi, Japan
cDepartment of Cardiovascular Surgery, Saitama Medical Center, Jichi Medical University, Saitama City, Saitama, Japan
dCorresponding Author: Kentaro Fukano, Department of Anesthesiology and Critical Care Medicine, Saitama Medical Center, Jichi Medical University, Omiya-ku, Saitama City, Saitama 330-8503, Japan
Manuscript submitted December 21, 2024, accepted February 24, 2025, published online March 11, 2025
Short title: Ascorbic Acid and Postoperative Delirium
doi: https://doi.org/10.14740/jocmr6169
| Abstract | ▴Top |
Background: Ascorbic acid is a strong antioxidant that prevents postoperative delirium by inhibiting reactive oxygen species production. This pilot study was designed to investigate the prevalence of postoperative delirium among older patients undergoing cardiovascular surgery, who received perioperative ascorbic acid administration, to estimate an appropriate sample size for further randomized controlled trials.
Methods: This single-arm prospective interventional study enrolled patients aged > 70 years scheduled to undergo elective cardiovascular surgery using cardiopulmonary bypass. Ascorbic acid (500 mg) was administered intravenously every 6 h for a total of eight times following the induction of general anesthesia. The incidence of postoperative delirium was evaluated until discharge using the Confusion Assessment Method for the Intensive Care Unit.
Results: Data from 48 patients were analyzed. Of the 48 patients, 16 developed postoperative delirium (33.3%). Patients in the delirium group had more severe heart failure (New York Heart Association Classification), higher European System for Cardiac Operative Risk Evaluation scores, lower intraoperative Bispectral Index, longer duration of cardiopulmonary bypass and surgery, incidence of postoperative cerebral infarction, longer intubation time, and length of intensive care unit stay.
Conclusions: The incidence of postoperative delirium among older patients undergoing cardiovascular surgery who received ascorbic acid perioperatively (2 g/day for 2 days) was 33%. This incidence was comparable to that observed in a previous observational study, suggesting that ascorbic acid administration may not be effective in preventing the incidence of postoperative delirium.
Keywords: Postoperative delirium; Cardiac surgery; Ascorbic acid
| Introduction | ▴Top |
The incidence of postoperative delirium (POD), a major cause of concern in the intensive care unit (ICU), affects short- and long-term prognoses [1]. A high prevalence of POD has been observed in patients who have undergone cardiac surgery. The reported incidences of POD after cardiovascular surgery vary from 4% to 55% [2]. POD is especially concerning among older patients undergoing cardiovascular surgery because of the increase in the number of older patients undergoing surgery. However, medications for the prevention of POD remain unknown [3, 4]. The incidence of POD among patients undergoing cardiac surgery may be attributed to several factors, such as preoperative cognitive function, aging, diabetes, European System for Cardiac Operative Risk Evaluation II (EuroSCORE II) score, New York Heart Association Classification (NYHA) functional class, intraoperative hypoperfusion, cumulative fluid balance, time of intubation, and length of stay in the ICU [2, 5-8]. Reactive oxygen species (ROS) generation during cardiopulmonary bypass (CPB) plays a substantial role in inducing POD in patients undergoing CPB cardiac surgery [9, 10].
CPB can induce a systemic inflammatory response via foreign surface contact and is a potential source of cerebral microemboli (thrombi, fat, or gas bubbles) [10-12]. These factors contribute to the incidence of ischemia/reperfusion injury, which is characterized by excessive ROS levels that can cause endothelial dysfunction, cellular injury, and multiple organ failure. The brain tissue is highly susceptible to oxidative damage due to the high content of polyunsaturated fatty acids and high oxygen demand. The high prevalence of POD among patients undergoing cardiac surgery with CPB may indicate greater brain damage due to the ROS generated by CPB than in patients without CPB. Minimizing the effects of ROS may be a strategy for preventing and treating POD.
Ascorbic acid, a vital water-soluble vitamin, acts as an electron donor by directly scavenging ROS. Furthermore, it prevents the generation of new ROS by inhibiting the nicotinamide adenine dinucleotide phosphate (NADPH) oxidase pathway and assists in the recycling of other antioxidants [13]. The postoperative ascorbic acid levels decrease because of the production of ROS after cardiac surgery with CPB, indicating a potential link between low plasma ascorbic acid levels and multiple organ damage [14-16]. Moreover, the plasma ascorbic acid levels of older patients scheduled for cardiac surgery were expected to be lower than normal levels (9 - 12 µg/mL) because plasma ascorbic acid levels have been reported to decrease with age, heart failure, and frailty [17-19]. Thus, ascorbic acid supplementation in older patients may reduce organ damage after cardiac surgery. Numerous studies have been conducted on the administration of ascorbic acid and the prevention of organ damage in cardiovascular surgery, particularly in the prevention of postoperative atrial fibrillation [20]. However, no previous studies have investigated whether ascorbic acid has a preventive effect on the incidence of delirium, a phenotype of brain damage. Ascorbic acid is the most important antioxidant in the brain, and its levels in the brain cells (350 - 1,700 µg/mL) are much higher than those in the plasma (9 - 12 µg/mL), owing to its active transport via the sodium-dependent vitamin C transporter-2 (SVCT2) [21].
Our previous study investigated the relationship between preoperative and postoperative blood ascorbic acid levels and the incidence of POD and revealed that 32% of the enrolled patients (31/98) developed POD [14]. The preoperative plasma ascorbic acid levels recorded immediately after the induction of general anesthesia were 5.6 (4.6 - 7.8) and 5.2 (3.6 - 7.2) µg/mL in the non-POD and POD groups, respectively. The postoperative plasma ascorbic acid levels were 2.8 (2.3 - 3.5) and 2.3 (1.6 - 3.3) µg/mL in the non-POD and POD groups, respectively. While the plasma ascorbic acid level decreased by more than 50% from the preoperative value in both groups, a significant association was detected between postoperative plasma ascorbic acid levels and the incidence of POD. Thus, the findings of this study suggest that the administration of ascorbic acid during cardiac surgery to compensate for the consumption of ascorbic acid may prevent the incidence of POD.
This study hypothesized that ascorbic acid administration would reduce the incidence of POD in older patients undergoing cardiovascular surgery. However, this is the first study in which ascorbic acid was administered to prevent delirium, and the Ethics Committee recommended that the incidence of POD following the administration of ascorbic acid should be examined without controls. Therefore, this study aimed to determine the prevalence of POD among older patients undergoing cardiovascular surgery, who received 2 g/day ascorbic acid for 2 days, to estimate an appropriate sample size for further randomized controlled trials, by comparing the incidence of POD in other studies without ascorbic acid administration. If the incidence of POD in this study was < 32% of that reported in a previous study conducted using the same inclusion criteria [14], the administration of ascorbic acid could be considered to have a preventive effect on the incidence of POD.
| Materials and Methods | ▴Top |
This single-center interventional study was approved by the Ethics Committee of the author’s institution on February 16, 2023. This study investigated the incidence of POD in older patients who underwent cardiovascular surgery with CPB. In accordance with the advice of the Ethics Committee, this was a single-arm study with no comparison, as no previous study has investigated whether the administration of ascorbic acid prevents the incidence of POD to estimate an adequate sample size. The inclusion criteria were as follows: 1) age > 70 years; 2) scheduled to undergo elective cardiovascular surgery using CPB. The exclusion criteria were as follows: 1) patients with cognitive disorders who could not understand the details of the present study; 2) patients requiring urgent surgery.
Perioperative management
An arterial catheter was placed in the radial artery and 5 mL of blood was drawn from the arterial catheter before or immediately after the induction of general anesthesia to determine preoperative plasma ascorbic acid levels. Ascorbic acid (500 mg) mixed with saline (50 mL) was administered intravenously over 10 min after drawing the preoperative sample. In addition, the solution was administered intravenously every 6 h for a total of eight times (2 g/day for 2 days) during the perioperative period.
Anesthetic management and hypothermic CPB were administered as follows. Midazolam/propofol/remimazolam, fentanyl, and rocuronium were administered intravenously to induce general anesthesia. Subsequently, 1-1.5% of sevoflurane and remifentanil were administered to maintain anesthesia, except during CPB when 1.5 - 4 mg/kg of propofol and 0.1 - 0.4 µg/kg/min of remifentanil were administered to maintain anesthesia. Valvular surgery was performed under the condition of mild hypothermia (bottom temperature set as 30 °C), whereas aortic surgery requiring circulatory arrest with CPB was performed under the condition of deep hypothermia (bottom temperature set as 25 °C). By the end of the surgery, 10 - 20 µg/kg of fentanyl was administered. All patients were transferred to the ICU postoperatively and extubated after hemodynamic stabilization. The hemodynamic target was to maintain a mean arterial pressure (MAP) of > 60 mm Hg, except during CPB when 50 - 80 mm Hg of MAP was the hemodynamic target. Hemofiltration was not routinely performed during CPB.
The postoperative plasma ascorbic acid levels were measured from plasma samples drawn 24 h after drawing the first preoperative sample and just before the fifth administration of ascorbic acid (usually in the morning on postoperative day 1). Plasma ascorbic acid levels were measured only on weekdays. The levels were not measured on weekends and holidays due to the unavailability of laboratory technicians.
The patients were monitored for POD incidence by an ICU nurse until discharge from the ICU using the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). The ICU nurses worked two shifts, day and night, with at least one CAM-ICU evaluation per shift. Some patients at risk for POD may be assessed more than once during a shift. Therefore, the CAM-ICU score was routinely assessed twice or more per day in all patients. Patients with at least one positive CAM-ICU result were considered to have delirium. The duration of delirium was defined as the period between positive and negative ICU CAM results. The duration of delirium was summed for each episode in cases in which multiple episodes of delirium were reported. Patient backgrounds and intraoperative and ICU events were reviewed from the charts. Intraoperative MAP and Bispectral Index (BIS), as parameters of anesthetic depth, were obtained from the anesthetic records every minute, except during CPB. We excluded information on BIS and MAP during CPB because the degree of hypothermia would interfere with the influence of hypotension and depth of anesthesia on POD.
Statistical analysis
This study aimed to estimate the incidence of POD following ascorbic acid administration. Because this was a pilot study with no comparisons, an adequate sample size could not be estimated. Data were collected from 50 older patients scheduled to undergo cardiac surgery with CPB. The normality of continuous variables was assessed using the Shapiro-Wilk test. Variables with normal distribution are expressed as mean ± standard deviation (SD), whereas the variables with non-normal distribution are expressed as medians (interquartile range (IQR)). As a secondary analysis, to represent the characteristics of patients with POD, we compared the groups with and without POD. Continuous variables were compared using the two-sample t-test and the Mann-Whitney U test, as appropriate. Categorical variables are expressed as numbers and compared using Fisher’s exact test or the Chi-square test, where appropriate. Statistical significance was set at P < 0.05. All statistical analyses were performed using EZR version 3.6.3. (Saitama Medical Center, Jichi Medical University, Saitama, Japan), a graphical user interface for R (version 3.6.3) (R Foundation for Statistical Computing, Vienna, Austria) [22]. Data were visualized using GraphPad Prism (version. 10.1.1, GraphPad Software LLC, Boston, MA, USA).
Ethics approval and consent to participate
This single-center interventional study was approved by the Jichi Medical University Central Clinical Research Ethics Committee on February 16, 2023. This study was conducted in accordance with the Declaration of Helsinki and was registered in the Japan Registry of Clinical Trial (jRCT) on March 9, 2023 (Registration No.: jRCTs031220690). Written informed consent was obtained from all the patients.
| Results | ▴Top |
Among 57 eligible patients who received explanations regarding the study objectives between April 2023 and December 2023, consent was obtained from 51 patients. One patient scheduled to undergo resection of a left atrial myxoma experienced a mild cerebral stroke due to the myxoma after providing consent; consequently, her willingness to consent to participate in the study was uncertain. Therefore, this patient was excluded from the study. Thus, 50 patients were enrolled in the study. Among the 50 patients scheduled to receive ascorbic acid, one patient did not receive ascorbic acid during the postoperative period. In addition, one patient developed fatal arrhythmia due to postoperative coronary graft occlusion and died. Thus, these patients were excluded from the analysis, and data from 48 patients were analyzed (Fig. 1).
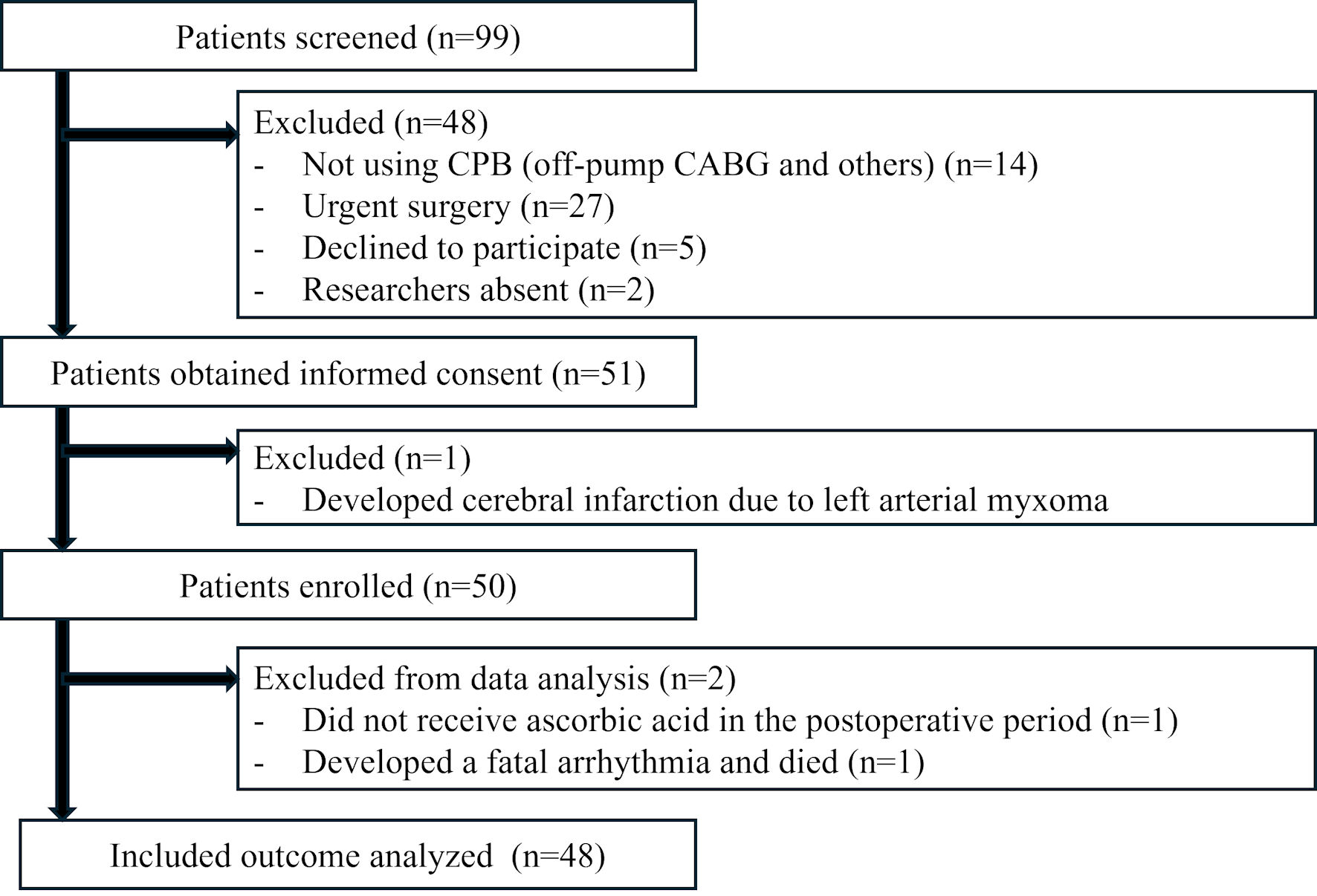 Click for large image | Figure 1. Flow chart depicting patient enrolment. CPB: cardiopulmonary bypass; CABG: coronary artery bypass graft. |
The characteristics of the enrolled patients are shown in Table 1. Sixteen patients developed POD (33.3%), whereas 32 patients did not. The mean duration of delirium in the POD group was 19.9 (11.3 - 59.5) h. The number of patients with NYHA functional class III/IV, higher EuroSCORE II, lower intraoperative BIS, longer duration of CPB and surgery, incidence of postoperative cerebral infarction, longer intubation time, and length of ICU stay were higher in the POD group. Significant differences were observed between the non-POD and POD groups in terms of the preoperative plasma ascorbic acid levels (6.08 ± 2.33 vs. 4.25 ± 1.26 µg/mL, P = 0.005); however, no significant differences were observed between the groups in terms of the postoperative plasma ascorbic acid levels (17.3 ± 5.6 vs. 22.1 ± 10.7 µg/mL, P = 0.09). The postoperative plasma ascorbic acid levels were measured in only 34 patients as these values could not be measured on weekends and holidays. Figure 2 shows a box plot of the preoperative and postoperative plasma ascorbic acid levels for each group. Figure 3 shows the distribution of EuroSCORE II and the incidence of POD. No adverse events attributable to ascorbic acid administration were observed in any patient.
 Click to view | Table 1. Patient Characteristics |
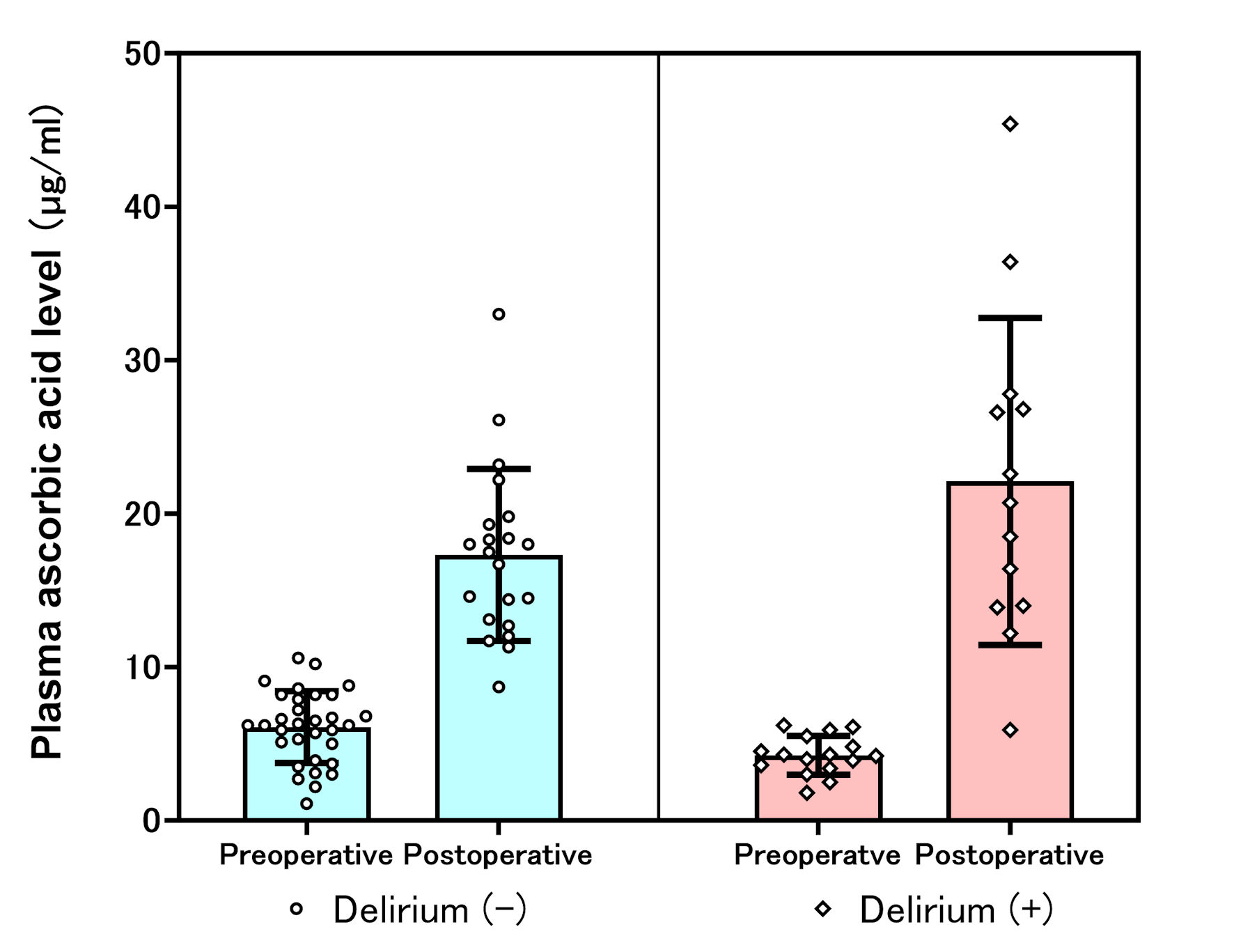 Click for large image | Figure 2. Plasma ascorbic acid levels in the non-delirium and delirium groups. |
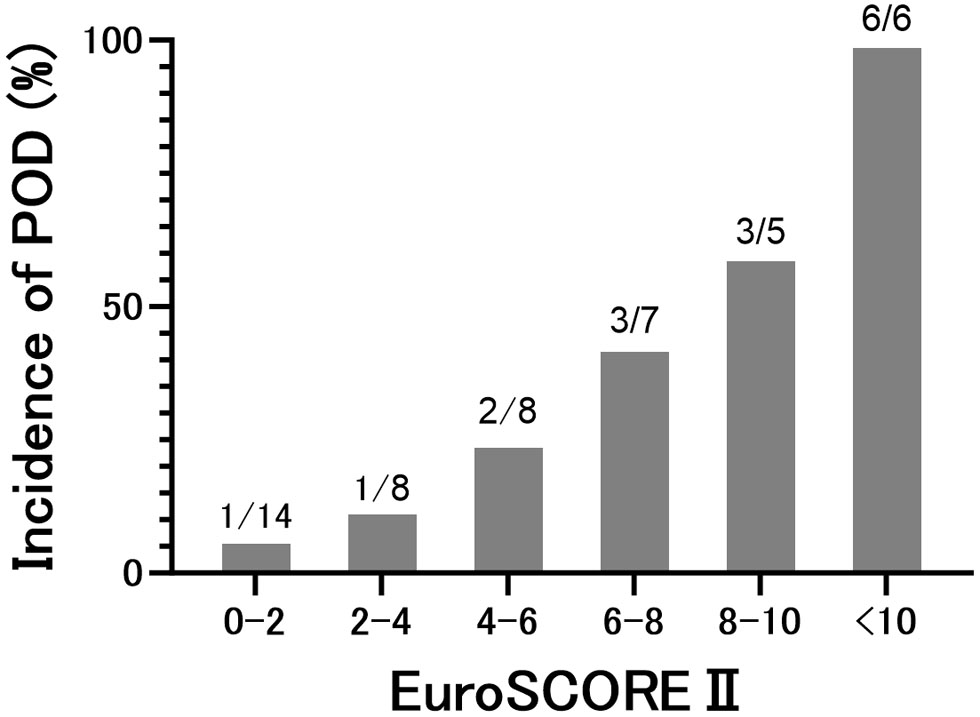 Click for large image | Figure 3. Distribution of EuroSCORE II and the incidence of postoperative delirium (POD). EuroSCORE II: European System for Cardiac Operative Risk Evaluation II. |
| Discussion | ▴Top |
The current study revealed that 33% of older patients undergoing cardiovascular surgery with CPB who received ascorbic acid at a dose of 2 g/day for 2 days experienced POD. To the best of our knowledge, this is the first study to examine the effects of ascorbic acid administration on the incidence of POD in this patient group. These findings may help estimate an appropriate sample size for future pilot randomized clinical trials.
Several studies have reported the effects of ascorbic acid in patients undergoing cardiac surgery. However, most of these studies have focused on its role in preventing postoperative atrial fibrillation, with many studies and meta-analyses indicating that the administration of ascorbic acid can reduce this condition [20, 23]. Other studies have noted benefits such as shorter mechanical ventilation duration, reduced ICU stay duration, and decreased overall hospital stay duration [20]. However, its protective effects against cerebral ischemic events, postoperative cognitive dysfunction, and delirium remain unclear. A significant decline in ascorbic acid levels in the brain has been observed during cerebral ischemia in animal models [24], indicating a strong association between ascorbic acid levels in the brain and the incidence of postoperative neurological complications such as delirium. Moreover, the administration of ascorbic acid effectively reduced the size of cerebral infarctions in animal models [25, 26]. Thus, the administration of ascorbic acid may protect the brain tissue and prevent the incidence of POD after cardiac surgery with CPB.
Contrary to our expectations, the incidence of POD (33% in this study) was almost identical to that observed in our previous observational study (31 of 98 patients developed POD; incidence of POD was 32%) [14]. This study lacked a control group for comparison, rendering it insufficient to conclusively determine the protective effect of ascorbic acid against delirium; however, the results suggest that the effect of ascorbic acid on preventing POD is minimal compared to that observed in our previous observational study. There are several possible explanations for these findings. The following factors that may influence the results may aid future research.
Severity of patient condition
The patient conditions in this study were more severe than those observed in our previous study. The patients in the POD group in this study exhibited higher EuroSCORE II scores, longer intubation times, and longer ICU stays. These differences in disease severity may have influenced our results. EuroSCORE II, which integrates patient, cardiac, and operation-related factors, predicts mortality after cardiac surgery [27]. High EuroSCORE II scores have been suggested as risk factors for POD development [6]. In the present study, patients with higher EuroSCORE II scores had a higher incidence of POD (Fig. 3). In the highest EuroSCORE II group (> 10%), the effect of 2 days of ascorbic acid supplementation was limited or disappeared because the intubation time and ICU stay were much longer than 2 days. A limited number of patients with mild-to-moderate severity (such as EuroSCORE II < 10%) could be appropriate to determine the effect of ascorbic acid more clearly. The incidence of POD in patients with EuroSCORE II < 10% was 23.8% in the present study and 29.2% in our previous study. This suggests that the sample size would need 2,170 patients in a future larger study, which investigates the effect of ascorbic acid on the prevention of POD in patients over 70 years of age scheduled for cardiac surgery with CPB and a mild-to-moderate risk of mortality (EuroSCORE II < 10%).
Dose of ascorbic acid
The dose of ascorbic acid administered may have influenced the outcome. A dose of 2 g/day was administered for 2 days in the current study. This dose appears to be minimal, as 2 - 4 g/day of ascorbic acid has been administered for 1 - 5 days in several studies investigating the effects of ascorbic acid administration in patients undergoing cardiac surgery [6]. The dose of ascorbic acid was set to 2 g/day, which is the maximum dose permitted in Japan. The duration of ascorbic acid administration in the ICU was set to 2 days in the current study, as a few patients may be discharged from the ICU on postoperative day 2. A small dose and short duration of ascorbic acid administration may be less likely to influence the incidence of POD than a larger dose and longer duration of ascorbic acid. Theoretically, the first dose administered before the start of CPB may be the most important for replenishing consumption during surgery. A larger initial dose of ascorbic acid may be required to maintain a high level of ascorbic acid at the beginning of CPB.
Type of ascorbic acid
The form of ascorbic acid used in this study may have affected its efficacy. Ascorbic acid can enter the cerebrospinal fluid directly through the choroid plexus via SVCT2 and can enter neurons via the same transporter. This process is slow, saturable, and controlled. Dehydroascorbate (DHA) is transported directly and quickly into the brain via glucose transporter (GLUT) 1 on the endothelial cells of the blood-brain barrier and via GLUT1 or GLUT3 in neurons [12, 23]. In neurons, DHA is converted into ascorbic acid by glutathione and other intracellular thiols. Intravenous administration of DHA, but not ascorbic acid, generates supraphysiological concentrations of ascorbic acid in the brain due to the more efficient uptake of DHA. The results might have varied if DHA had been used instead of ascorbic acid. However, ascorbic acid, the more stable form, was used in this study because the use of DHA is not permitted in Japan. Preoperative supplementation with ascorbic acid may be another option to achieve a high concentration of ascorbic acid in the brain more quickly at the beginning of CPB. In this study, no patients developed POD when their preoperative levels of ascorbic acid were above 6.3 µg/mL. Although this level seemed to be much lower than the normal range (9 - 12 µg/mL), it may imply that increasing preoperative ascorbic acid levels to within the normal range might be useful. Moreover, the use of DHA to maintain adequate plasma and brain levels of ascorbic acid swiftly needs to be assessed in future studies.
Limitations
The primary limitation of this study is its design, which lacked a control group. Ideally, a control arm without ascorbic acid administration would be necessary. However, due to the absence of prior studies investigating the use of ascorbic acid for delirium prevention in patients undergoing cardiovascular surgery, the Ethics Committee initially assessed the incidence of delirium without a control group. The committee decided that the study was not at a stage where ascorbic acid should be studied in two groups, given its unknown effect on delirium, and its potential aggravating effect. Consequently, this study was not suitable for evaluating the preventive effects of ascorbic acid on delirium. The second limitation of this study is its small sample size, heterogeneous population, and single-center design. Particularly, the variety of patients who underwent aortic surgery with CPB under deep hypothermia might have affected the results, because these patients might have had a higher incidence of POD than those who underwent usual cardiac surgery. Three patients (all counted in the composite surgery group) were in the non-POD group, and six (two in the composite surgery and four in the aortic surgery group) were in the POD group. This heterogeneous population may limit the generalizability and reproducibility of our findings to other institutions. Third, we had three patients with mild postoperative cerebral infarction discovered from delayed emergence only in the POD group. Cerebral infarction may affect the incidence of POD because cerebral infarction is a risk factor for POD. However, these patients were not excluded from the analysis. Since the patients did not undergo routine postoperative brain magnetic resonance imaging (MRI) or computed tomography (CT), we could not rule out the occurrence of mild cerebral infarction in other patients. Hence, the effect of mild cerebral infarction on POD in this study was unclear. Fourth, dexmedetomidine was administered to six patients in the non-POD group during their ICU stay. Since dexmedetomidine has been suggested to reduce POD [4], its use may have influenced the results. Fifth, the incidence of delirium was determined using the CAM-ICU, which may not capture the effects of postoperative cognitive dysfunction, such as subclinical delirium (e.g., hallucinations), which can occur even in patients who are CAM-ICU-negative. Subsyndromal delirium, which is characterized by mild cognitive dysfunction, does not meet the formal criteria for delirium, and its symptoms vary substantially [28]. Administration of ascorbic acid may reduce overall cognitive dysfunction; however, data on subsyndromal delirium were not collected in the current study.
Conclusions
The incidence of POD among older patients who underwent cardiovascular surgery and received perioperative ascorbic acid (2 g/day for 2 days) was 33%. This incidence was comparable to that observed in our previous observational study. Thus, the ascorbic acid regimen may not be effective in preventing delirium. Further studies are warranted to investigate the effects of ascorbic acid on POD prevention in homogeneous populations.
Acknowledgments
None to declare.
Financial Disclosure
This study was supported by MEXT KAKENHI (grant number: JP20275452).
Conflict of Interest
The authors declare that they have no known competing financial interests or personal relationships that could have influenced the work reported in this study.
Informed Consent
Written informed consent was obtained from all the patients.
Author Contributions
YI, MS, and AY contributed to the study conception and design. YI, KF, S. Oki, IS, KM, S. Ono, and KY were involved in data investigation, and YI, KF, and KY analyzed and interpreted the data. YI was the major contributor to the writing of the manuscript. All authors critically revised, read, and approved the final manuscript.
Data Availability
The data presented in this study are available upon request from the corresponding authors.
Abbreviations
CAM-ICU: Confusion Assessment Method for the Intensive Care Unit; CPB: cardiopulmonary bypass; DHA: dehydroascorbate; GLUT: glucose transporter; ICU: intensive care unit; jRCT: Japan Registry of Clinical Trial; NADPH: nicotinamide adenine dinucleotide phosphate; POD: postoperative delirium; ROS: reactive oxygen species; SVCT2: sodium-dependent vitamin C transporter-2
| References | ▴Top |
- Marcantonio ER. Delirium in hospitalized older adults. N Engl J Med. 2017;377(15):1456-1466.
doi pubmed - Chen H, Mo L, Hu H, Ou Y, Luo J. Risk factors of postoperative delirium after cardiac surgery: a meta-analysis. J Cardiothorac Surg. 2021;16(1):113.
doi pubmed - Hayhurst CJ, Pandharipande PP, Hughes CG. Intensive care unit delirium: a review of diagnosis, prevention, and treatment. Anesthesiology. 2016;125(6):1229-1241.
doi pubmed - Pieri M, De Simone A, Rose S, De Domenico P, Lembo R, Denaro G, Landoni G, et al. Trials focusing on prevention and treatment of delirium after cardiac surgery: a systematic review of randomized evidence. J Cardiothorac Vasc Anesth. 2020;34(6):1641-1654.
doi pubmed - Gosselt AN, Slooter AJ, Boere PR, Zaal IJ. Risk factors for delirium after on-pump cardiac surgery: a systematic review. Crit Care. 2015;19(1):346.
doi pubmed - Greaves D, Psaltis PJ, Davis DHJ, Ross TJ, Ghezzi ES, Lampit A, Smith AE, et al. Risk factors for delirium and cognitive decline following coronary artery bypass grafting surgery: a systematic review and meta-analysis. J Am Heart Assoc. 2020;9(22):e017275.
doi pubmed - Mohr NL, Krannich A, Jung H, Hulde N, von Dossow V. Intraoperative blood pressure management and its effects on postoperative delirium after cardiac surgery: a single-center retrospective cohort study. J Cardiothorac Vasc Anesth. 2024;38(5):1127-1134.
doi pubmed - Mailhot T, Cossette S, Lambert J, Beaubien-Souligny W, Cournoyer A, O'Meara E, Maheu-Cadotte MA, et al. Delirium after cardiac surgery and cumulative fluid balance: a case-control cohort study. J Cardiothorac Vasc Anesth. 2019;33(1):93-101.
doi pubmed - Faisal H, Farhat S, Grewal NK, Masud FN. ICU delirium in cardiac patients. Methodist Debakey Cardiovasc J. 2023;19(4):74-84.
doi pubmed - Hill A, Wendt S, Benstoem C, Neubauer C, Meybohm P, Langlois P, Adhikari NK, et al. Vitamin C to improve organ dysfunction in cardiac surgery patients-review and pragmatic approach. Nutrients. 2018;10(8):974.
doi pubmed - van Harten AE, Scheeren TW, Absalom AR. A review of postoperative cognitive dysfunction and neuroinflammation associated with cardiac surgery and anaesthesia. Anaesthesia. 2012;67(3):280-293.
doi pubmed - Spoelstra-de Man AME, Elbers PWG, Oudemans-van Straaten HM. Making sense of early high-dose intravenous vitamin C in ischemia/reperfusion injury. Crit Care. 2018;22(1):70.
doi pubmed - Moskowitz A, Andersen LW, Huang DT, Berg KM, Grossestreuer AV, Marik PE, Sherwin RL, et al. Ascorbic acid, corticosteroids, and thiamine in sepsis: a review of the biologic rationale and the present state of clinical evaluation. Crit Care. 2018;22(1):283.
doi pubmed - Iizuka Y, Yoshinaga K, Takahashi K, Oki S, Chiba Y, Sanui M, Kimura N, et al. Association between plasma ascorbic acid levels and postoperative delirium in older patients undergoing cardiovascular surgery: a prospective observational study. J Cardiovasc Dev Dis. 2023;10(7):293.
doi pubmed - Lassnigg A, Punz A, Barker R, Keznickl P, Manhart N, Roth E, Hiesmayr M. Influence of intravenous vitamin E supplementation in cardiac surgery on oxidative stress: a double-blinded, randomized, controlled study. Br J Anaesth. 2003;90(2):148-154.
doi pubmed - Rodemeister S, Duquesne M, Adolph M, Nohr D, Biesalski HK, Unertl K. Massive and long-lasting decrease in vitamin C plasma levels as a consequence of extracorporeal circulation. Nutrition. 2014;30(6):673-678.
doi pubmed - Travica N, Ried K, Hudson I, Sali A, Scholey A, Pipingas A. The contribution of plasma and brain vitamin C on age and gender-related cognitive differences: a mini-review of the literature. Front Integr Neurosci. 2020;14:47.
doi pubmed - Wannamethee SG, Bruckdorfer KR, Shaper AG, Papacosta O, Lennon L, Whincup PH. Plasma vitamin C, but not vitamin E, is associated with reduced risk of heart failure in older men. Circ Heart Fail. 2013;6(4):647-654.
doi pubmed - Sharma Y, Popescu A, Horwood C, Hakendorf P, Thompson C. Prevalence of hypovitaminosis c and its relationship with frailty in older hospitalised patients: a cross-sectional study. Nutrients. 2021;13(6):2117.
doi pubmed - Hill A, Clasen KC, Wendt S, Majoros AG, Stoppe C, Adhikari NKJ, Heyland DK, et al. Effects of vitamin C on organ function in cardiac surgery patients: a systematic review and meta-analysis. Nutrients. 2019;11(9):2103.
doi pubmed - Lykkesfeldt J, Tveden-Nyborg P. The pharmacokinetics of vitamin C. Nutrients. 2019;11(10):2412.
doi pubmed - Kanda Y. Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transplant. 2013;48(3):452-458.
doi pubmed - Shi R, Li ZH, Chen D, Wu QC, Zhou XL, Tie HT. Sole and combined vitamin C supplementation can prevent postoperative atrial fibrillation after cardiac surgery: A systematic review and meta-analysis of randomized controlled trials. Clin Cardiol. 2018;41(6):871-878.
doi pubmed - Flamm ES, Demopoulos HB, Seligman ML, Poser RG, Ransohoff J. Free radicals in cerebral ischemia. Stroke. 1978;9(5):445-447.
doi pubmed - Henry PT, Chandy MJ. Effect of ascorbic acid on infarct size in experimental focal cerebral ischaemia and reperfusion in a primate model. Acta Neurochir (Wien). 1998;140(9):977-980.
doi pubmed - Ranjan A, Theodore D, Haran RP, Chandy MJ. Ascorbic acid and focal cerebral ischaemia in a primate model. Acta Neurochir (Wien). 1993;123(1-2):87-91.
doi pubmed - Sullivan PG, Wallach JD, Ioannidis JP. Meta-analysis comparing established risk prediction models (EuroSCORE II, STS Score, and ACEF Score) for perioperative mortality during cardiac surgery. Am J Cardiol. 2016;118(10):1574-1582.
doi pubmed - Breu A, Stransky M, Metterlein T, Werner T, Trabold B. Subsyndromal delirium after cardiac surgery. Scand Cardiovasc J. 2015;49(4):207-212.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.