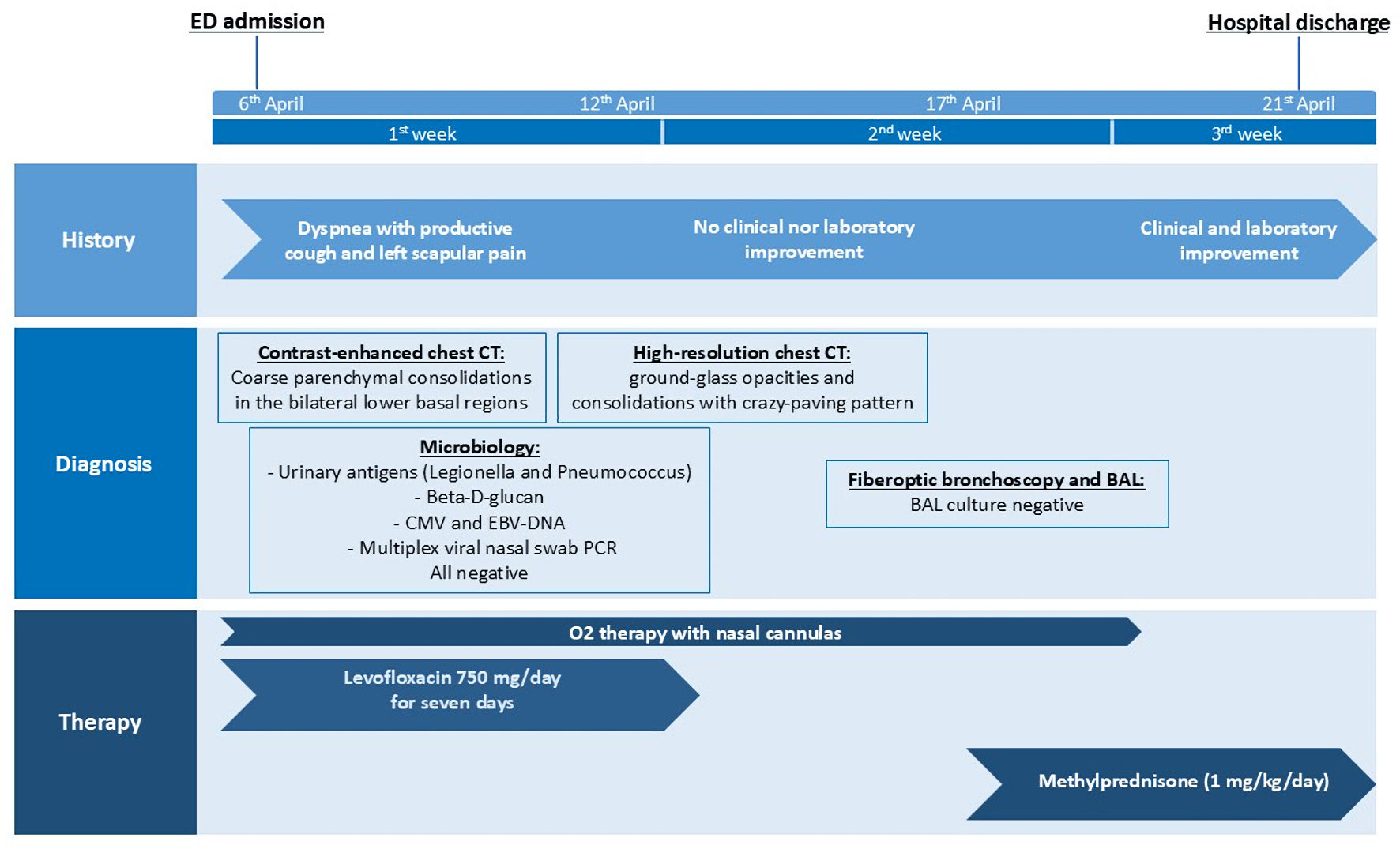
Figure 1. Timeline of the clinical case. CT: computed tomography; BAL: bronchoalveolar lavage; CMV: cytomegalovirus; EBV: Ebstein-Barr virus; ED: emergency department; PCR: polymerase chain reaction.
| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://jocmr.elmerjournals.com |
Case Report
Volume 17, Number 10, October 2025, pages 595-600
A Challenging Case of Immune-Related Organizing Pneumonitis Following Programmed Cell Death 1 Inhibitor Therapy in Non-Small Cell Lung Cancer
Figures

Table
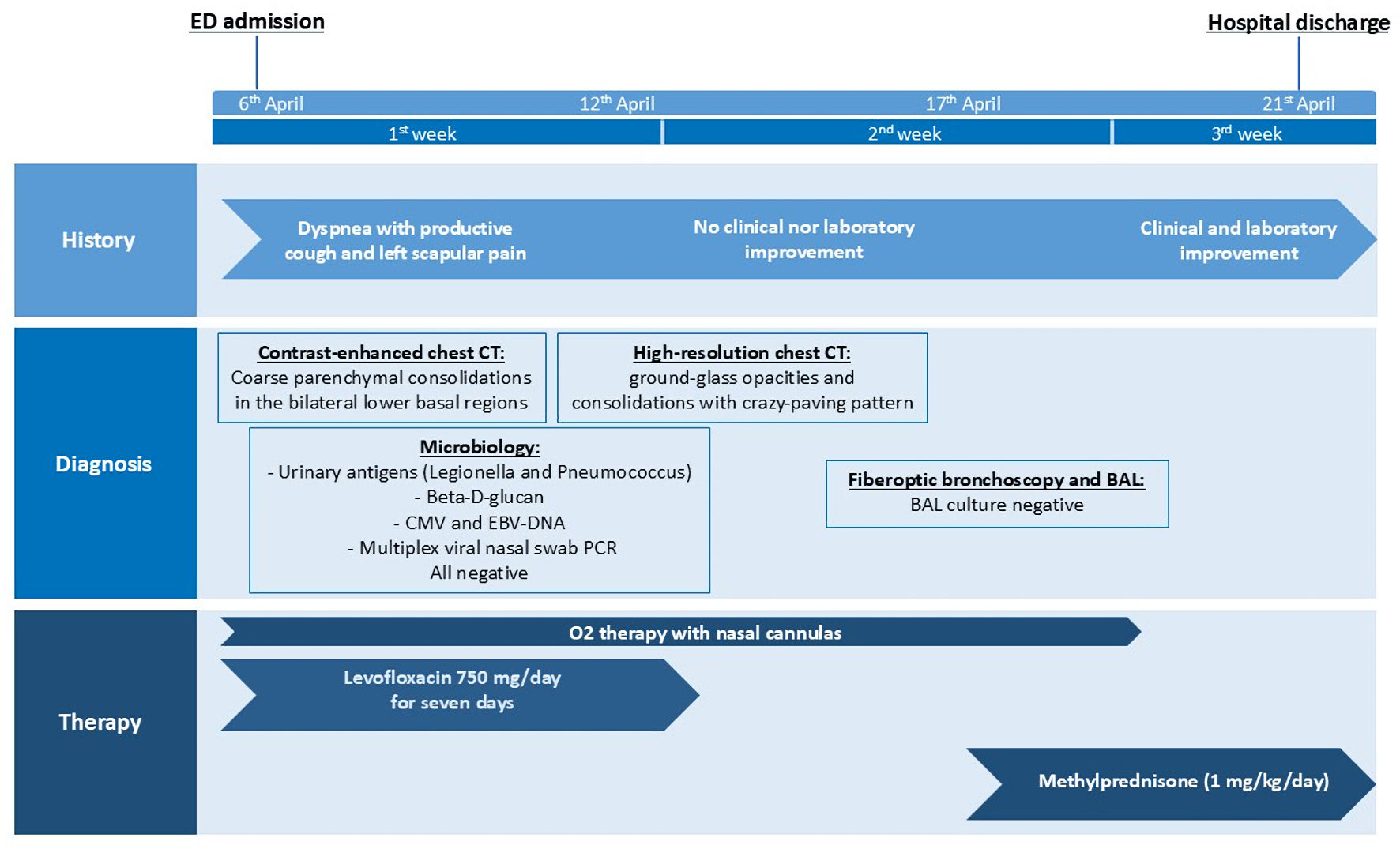
| Grading | Management |
|---|---|
| BAL: bronchoalveolar lavage; CT: computed tomography; DLCO: diffusing capacity of lung for carbon monoxide; ICI: immune checkpoint inhibitor; IV: intravenous; IVIG: intravenous immunoglobulin. | |
| G1: asymptomatic; confined to one lobe of the lung or 25% of lung parenchyma; clinical or diagnostic observations only | Hold ICI or proceed with close monitoring. Monitor patients weekly with history and physical examination, pulse oximetry; chest imaging (X-ray or CT) if uncertain diagnosis and/or to follow progress. Repeat chest imaging in 3 - 4 weeks or sooner if patient becomes symptomatic. In patients with baseline spirometry or DLCO, repeated testing may be considered in 3 - 4 weeks. May resume ICI with radiographic evidence of improvement or resolution if held. If there is no improvement, treat it as G2. |
| G2: symptomatic; involves more than one lobe of the lung or 25-50% of lung parenchyma; medical intervention indicated; limiting daily activities | Hold ICI until clinical improvement to G1. Prednisone 1 - 2 mg/kg/day and taper over 4 - 6 weeks. Consider bronchoscopy with BAL ± transbronchial biopsy. Consider empiric antibiotics if infection remains in the differential diagnosis after workup. Monitor at least once per week with history and physical examination, pulse oximetry, consider radiologic imaging; if there is no clinical improvement after 48 - 72 h of prednisone, treat it as grade 3. Pulmonary and infectious disease consults if necessary. |
| G3: severe symptoms; hospitalization required; involves all lung lobes or 50% of lung parenchyma; limiting self-care daily activities; oxygen indicated | Permanently discontinue ICI. Empiric antibiotics may be considered. Methylprednisolone IV 1 - 2 mg/kg/day. If there is no improvement after 48 h, may add immunosuppressive agent. Options include infliximab or mycophenolate mofetil IV or IVIG or cyclophosphamide. Taper corticosteroids over 4 - 6 weeks. Pulmonary and infectious disease consults if necessary. G4: life-threatening respiratory compromise; urgent intervention indicated (intubation) May consider bronchoscopy with BAL ± transbronchial biopsy if patient can tolerate. |