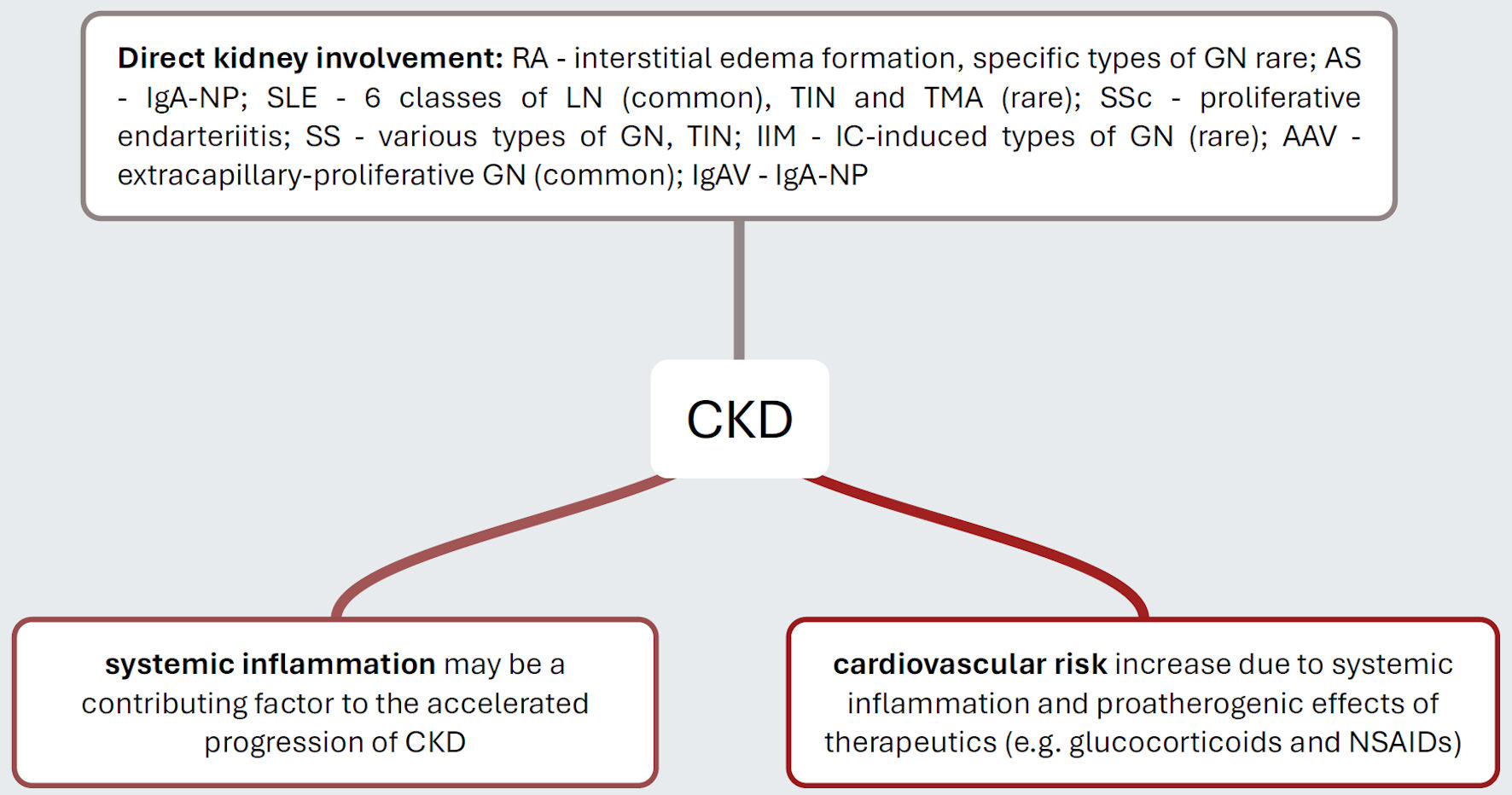
Figure 1. Pathogenetic mechanisms that explain the increased risk of CKD in distinct inflammatory rheumatic diseases. Rheumatic autoimmunopathies manifest themselves with varying frequency directly on the kidneys, with SLE and AAV being disproportionately common. It is now considered certain that individuals with rheumatic autoimmunopathies suffer from a significantly increased cardiovascular risk, which ultimately increases the risk of hypertensive atherosclerotic nephropathy. Presumably, the inflammatory activity of the diseases themselves is also a progression-promoting factor. CKD: chronic kidney disease; RA: rheumatoid arthritis; GN: glomerulonephritis; IgA-NP: IgA nephropathy; SLE: systemic lupus erythematosus; LN: lupus nephritis; TIN: tubulo-interstitial nephritis; TMA: thrombotic microangiopathy; SSc: systemic sclerosis; SS: Sjogren’s syndrome; IIM: idiopathic inflammatory myopathy; IC: immunocomplex; AAV: ANCA-associated vasculitis; IgAV: IgA vasculitis; NSAIDs: nonsteroidal anti-inflammatory drugs.