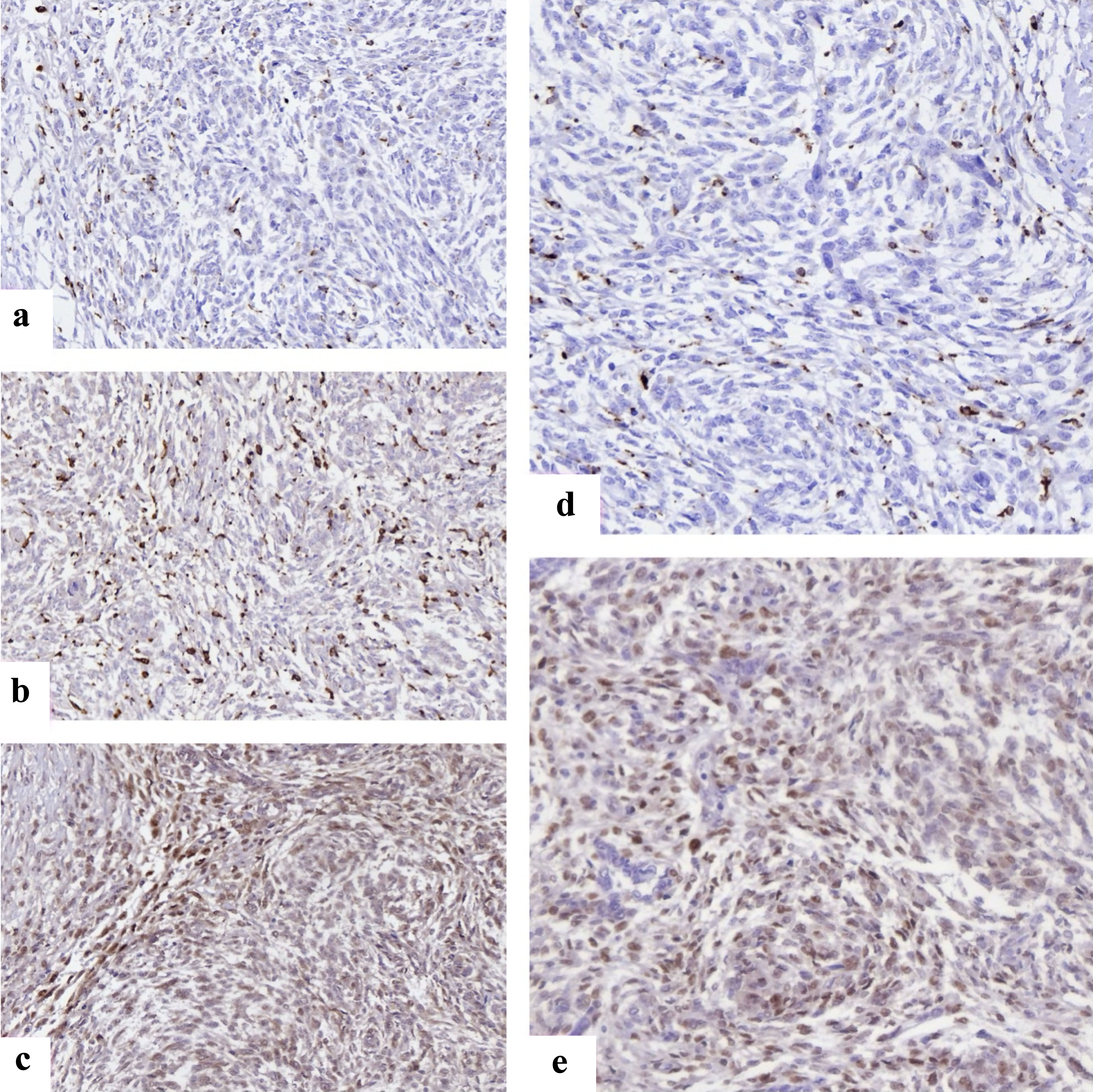
Figure 1. Representative immunohistochemical staining of immune and cell cycle markers in endometrial stromal sarcomas. (a) FOXP3+ regulatory T cells with distinct nuclear staining scattered within tumor stroma, reflecting immune evasion. (b) CD68 positivity showing widespread macrophage infiltration across tumor areas. (c) CD163 highlights M2-polarized macrophages, enriched at invasive margins, supporting an immunosuppressive microenvironment. (d) Cyclin D1 nuclear overexpression in HG-ESS, consistent with deregulated cell cycle progression. (e) CDK4 nuclear and cytoplasmic expression in HG-ESS tumor cells. CDK4: cyclin-dependent kinase 4; FOXP3: forkhead box P3; HG-ESS: high-grade endometrial stromal sarcoma.