| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://jocmr.elmerjournals.com |
Original Article
Volume 16, Number 7-8, August 2024, pages 345-354
Effect of Comorbidities on the Incidence of Surgical Site Infection in Patients Undergoing Emergency Surgery: A Systematic Review and Meta-Analysis
Asriwati Amiraha, d, Juliandi Harahapb, Herick Alvenus Willimc, Razia Begum Suroyoa, Alhoi Hendry Hendersonc
aFaculty of Public Health, Institut Kesehatan Helvetia, Medan, Indonesia
bFaculty of Medicine, Universitas Sumatera Utara, Medan, Indonesia
cDr. Agoesdjam Public Hospital, Ketapang Regency, West Kalimantan, Indonesia
dCorresponding Author: Asriwati Amirah, Faculty of Public Health, Institut Kesehatan Helvetia, Medan, Indonesia
Manuscript submitted June 2, 2024, accepted July 20, 2024, published online August 12, 2024
Short title: Comorbidities and Surgical Site Infection
doi: https://doi.org/10.14740/jocmr5222
| Abstract | ▴Top |
Background: Surgical site infection (SSI) is a significant concern in patients undergoing emergency surgery, particularly in those with underlying comorbidities. This meta-analysis aimed to evaluate the effect of comorbidities, including diabetes mellitus, hypertension, obesity, pulmonary disease, cardiac disease, liver disease, and renal disease, on the incidence of SSI in patients undergoing emergency surgery.
Methods: We performed a systematic literature search across electronic databases including PubMed, ScienceDirect, Cochrane Library, ProQuest, and Google Scholar to identify studies examining the effect of comorbidities on the incidence of SSI in patients undergoing emergency surgery. To determine the effect size, pooled odds ratios (ORs) were calculated. Statistical analysis was performed using Review Manager 5.3 software.
Results: Thirteen studies involving 8,952 patients undergoing emergency surgery were included in this meta-analysis. The pooled analysis showed that the following comorbidities significantly increased the risk of SSI following emergency surgery: diabetes mellitus (OR = 2.22; 95% confidence interval (CI) = 1.52 - 3.25; P < 0.0001), obesity (OR = 1.43; 95% CI = 1.19 - 1.72; P = 0.0001), and liver disease (OR = 1.66; 95% CI = 1.37 - 2.00; P < 0.00001). However, hypertension, pulmonary disease, cardiac disease, and renal disease showed no significant association with SSI.
Conclusions: In patients undergoing emergency surgery, the presence of comorbidities including diabetes mellitus, obesity, and liver disease increases the incidence of developing SSI.
Keywords: Comorbidity; Surgical site infection; Emergency; Surgery
| Introduction | ▴Top |
Surgery is one of the essential components of public health services. One important aspect to consider for patients undergoing surgery is the risk of developing surgical site infection (SSI). SSI is an infection that occurs at the incision site or around the incision site within 30 days post-surgery or within 90 days post-implantation of a prosthetic device [1]. Despite improvements in surgical techniques and infection prevention strategies, SSI continues to occur at a concerning rate. SSIs are among the most frequent infections in hospital settings (nosocomial/hospital-acquired infections). SSIs represent 20% to 39% of all nosocomial infections [2].
According to recent studies, the incidence of SSIs is estimated to be between 2% and 11% of all surgical procedures [3]. SSI rates are reported to be higher in developing countries than in developed ones. For instance, a study in Ethiopia with 251 patients who underwent surgery at a tertiary hospital found an SSI incidence of 21.1% [4]. Conversely, a large study in Germany, which included 221,113 patients from 79 hospitals, reported an SSI incidence of 4.9% [5]. In Indonesia, SSI incidence ranges from 5.3% to 13.9% [6]. SSIs can develop shortly after surgery or several days to weeks later, but they most commonly occur between the fifth and 10th day post-surgery [7].
Patients undergoing emergency surgery have been reported to have a higher incidence of SSIs compared to those undergoing elective surgery. A study in 2019 reported that the incidence of SSI in developing countries for elective surgeries was 7.5%, whereas for emergency surgeries it was 19.2% [8]. Patients undergoing emergency surgery have higher morbidity and mortality rates. In this context, predicting and preventing SSI in this vulnerable patient group is crucial [9]. Identifying risk factors and implementing preventive measures for SSI are essential to improve patient clinical outcomes, reduce hospitalization duration, and decrease hospital cost burdens [10].
Comorbidities are a significant factor in determining the risk of SSIs in patients undergoing emergency surgery. Patients with comorbidities such as diabetes mellitus, hypertension, obesity, pulmonary diseases, cardiac diseases, liver diseases, and renal diseases theoretically have a higher risk of experiencing postoperative complications, including SSIs. Although many studies have reported the effects of comorbidities on the incidence of SSIs after emergency surgery, the variability in these research findings remains a challenge in consistently identifying comorbidities that have a significant relationship. Identifying and managing comorbidities before, during, and after surgery is crucial for reducing the risk of SSIs and improving patient clinical outcomes [11, 12].
So far, to the best of our knowledge, there have been no previous systematic reviews and meta-analyses in the literature examining the effect of comorbidities on the incidence of SSI in patients undergoing emergency surgery. Recognizing the need for robust evidence and aiming to address this research gap, we conducted this systematic review and meta-analysis to comprehensively identify and evaluate the latest evidence regarding the effect of comorbidities on the incidence of SSI in patients undergoing emergency surgery.
| Materials and Methods | ▴Top |
Study registration
The study protocol for this research was registered in the International Prospective Register of Systematic Reviews (PROSPERO) under registration number CRD42024548893.
Search strategy
This meta-analysis was conducted based on the guidelines from Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [13]. We systematically searched several online databases, including PubMed, ScienceDirect, Cochrane Library, ProQuest, and Google Scholar, for relevant studies published from 2010 to March 2024. The keywords used were a combination of: (“comorbidity” OR “comorbidities”) AND (“surgical site infection” OR “surgical wound infection”) AND “emergency” AND (“surgery” OR “operation”). There were no geographical or country restrictions in the search for studies.
Inclusion and exclusion criteria
The inclusion criteria for the eligible studies were: 1) studies that were cross-sectional, cohort, case-control, or retrospective in design; 2) studies involving patients who underwent any type of emergency surgery; 3) studies that evaluated the number of patients with and without comorbidities; 4) studies providing sufficient data to calculate the number of events necessary for determining odds ratios (ORs) along with the corresponding 95% confidence intervals (CIs); and 5) studies available in full-text format. The exclusion criteria were: 1) review articles, case reports, letters, editorials, and conference abstracts; 2) animal studies; 3) studies lacking sufficient data to estimate effect size; and 4) duplicate or overlapping studies.
Data extraction
Three authors (AA, JH, and HAW) independently conducted data extraction from the relevant studies. Any disagreements regarding data extraction were resolved through discussions with the remaining authors (RBS and AHH). We gathered various details from the selected articles, including the first author’s name, publication date, study location, study design, demographic characteristics, sample size (in either the SSI or non-SSI group), comorbidities, and the necessary data for calculating OR with 95% CI. The comorbidities included diabetes mellitus, hypertension, obesity, pulmonary diseases, cardiac diseases, liver diseases, and renal diseases.
Quality assessment
Three authors (AA, JH, and HAW) independently evaluated the quality of the included studies. Any disagreements were resolved through discussions with the remaining authors (RBS and AHH). The Newcastle-Ottawa Scale (NOS) was utilized to assess study quality, scoring from zero to nine stars across three criteria: patient selection (zero to four stars), comparability of study groups (zero to two stars), and outcome (zero to three stars). Studies scoring ≥ 7 were considered high quality with low risk of bias, those scoring 5 - 6 were considered moderate quality with moderate risk of bias, and those scoring ≤ 4 were considered low quality with high risk of bias [14].
Statistical analysis
Statistical analyses were performed using Review Manager 5.3 software (The Nordic Cochrane Centre, Copenhagen). The meta-analysis calculated OR with 95% CI for dichotomous variables. Heterogeneity was assessed using the Cochran’s Q Chi-square test and the I2 statistic. Significant heterogeneity was considered when the P value was below 0.05 and I2 was greater than 50%. In instances without heterogeneity, a fixed-effects model was employed. However, in the presence of heterogeneity, a random-effects model was utilized. Statistical significance was determined by any test statistics with a P value less than 0.05.
The Institutional Review Board approval was not required since this study is a systematic review and meta-analysis. This study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
| Results | ▴Top |
Literature search
A systematic literature search was performed on electronic databases, initially yielding 1,079 potential articles. After eliminating duplicates, 864 articles remained for screening based on their titles and abstracts. Of these, 157 articles were chosen for full-text review, and 144 were excluded due to insufficient data or because they involved elective surgery. Ultimately, 13 studies were included in this meta-analysis [15-27]. The flowchart of the literature search process is depicted in Figure 1.
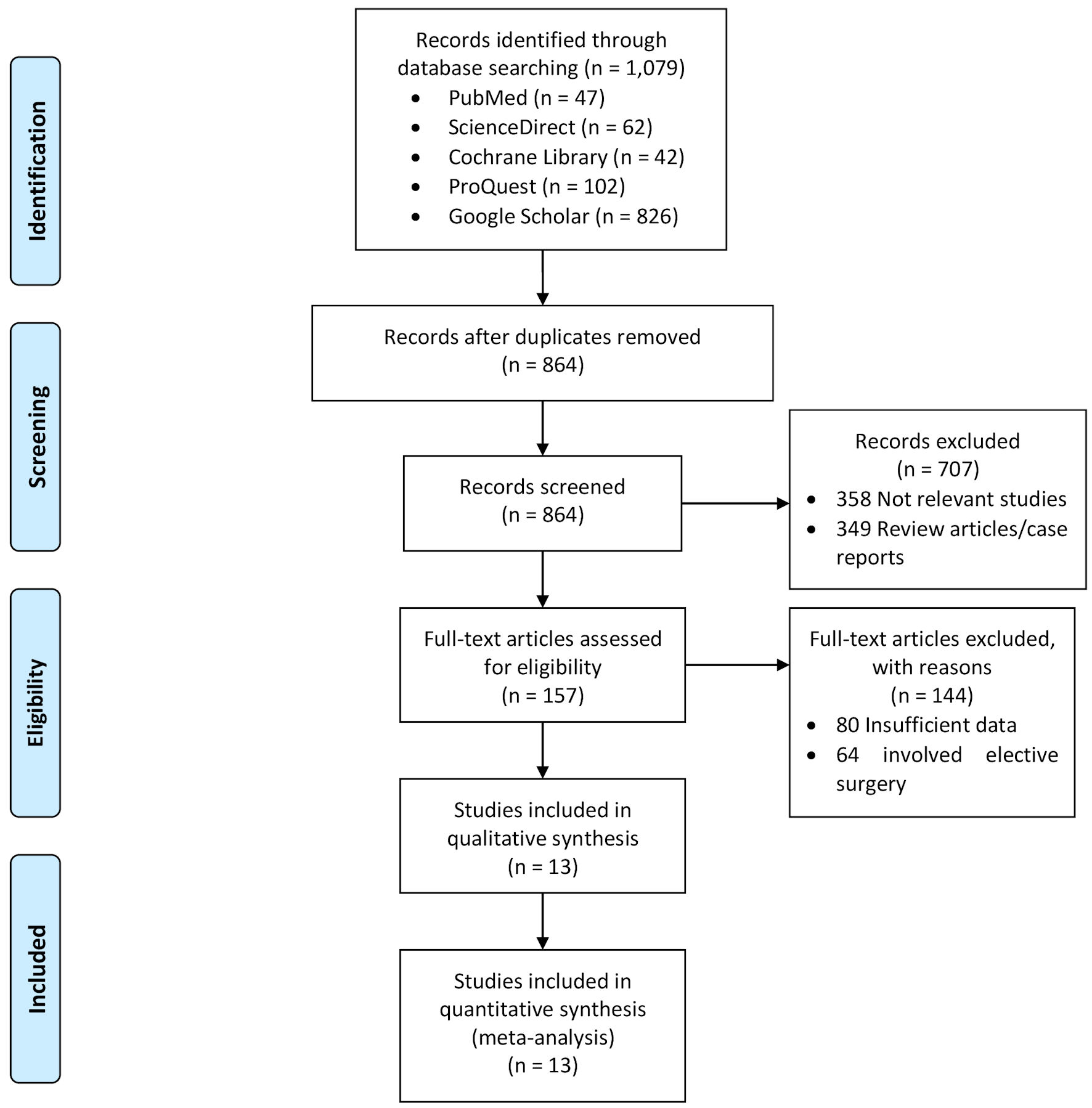 Click for large image | Figure 1. Literature search flow chart. |
Study characteristics and quality assessment
This meta-analysis included 13 studies involving a total of 8,952 patients [15-27]. Among these, six were retrospective cohort studies and seven were prospective cohort studies, conducted between 2014 and 2023. Geographically, three studies were conducted in China, two in the USA, two in India, and one each in Egypt, Bangladesh, Massachusetts, Greece, Japan, and Nepal. The participants’ mean age ranged from 33 to 68 years. The quality of the included studies was assessed using the NOS, with all quality scores ranging from 7 to 9, indicating generally high-quality studies with a low risk of bias. Table 1 [15-27] details the characteristics of the included studies, while Table 2 [15-27] presents the quality assessments.
 Click to view | Table 1. Characteristics of the Included Studies in the Meta-Analysis |
 Click to view | Table 2. Quality Assessment of the Included Studies by Newcastle-Ottawa Scale |
Pooled results
The pooled results from the included studies are presented in Table 3.
 Click to view | Table 3. Meta-Analysis of the Effect of Comorbidities on SSI in Patients Undergoing Emergency Surgery |
Diabetes mellitus
Eleven studies reported data on the comorbidity of diabetes mellitus. The incidence of SSI in the diabetes mellitus group was 18.5% (270 out of 1,459 patients), while in the non-diabetes mellitus group it was 11.9% (859 out of 7,275 patients). There was significant heterogeneity with an I2 of 67%. Analysis using a random-effects model (Fig. 2) showed that diabetes mellitus is significantly associated with SSI in patients undergoing emergency surgery (OR = 2.22; 95% CI = 1.52 - 3.25; P < 0.0001). This means that patients with diabetes mellitus have a 2.22 times higher risk of developing SSI compared to non-diabetic patients.
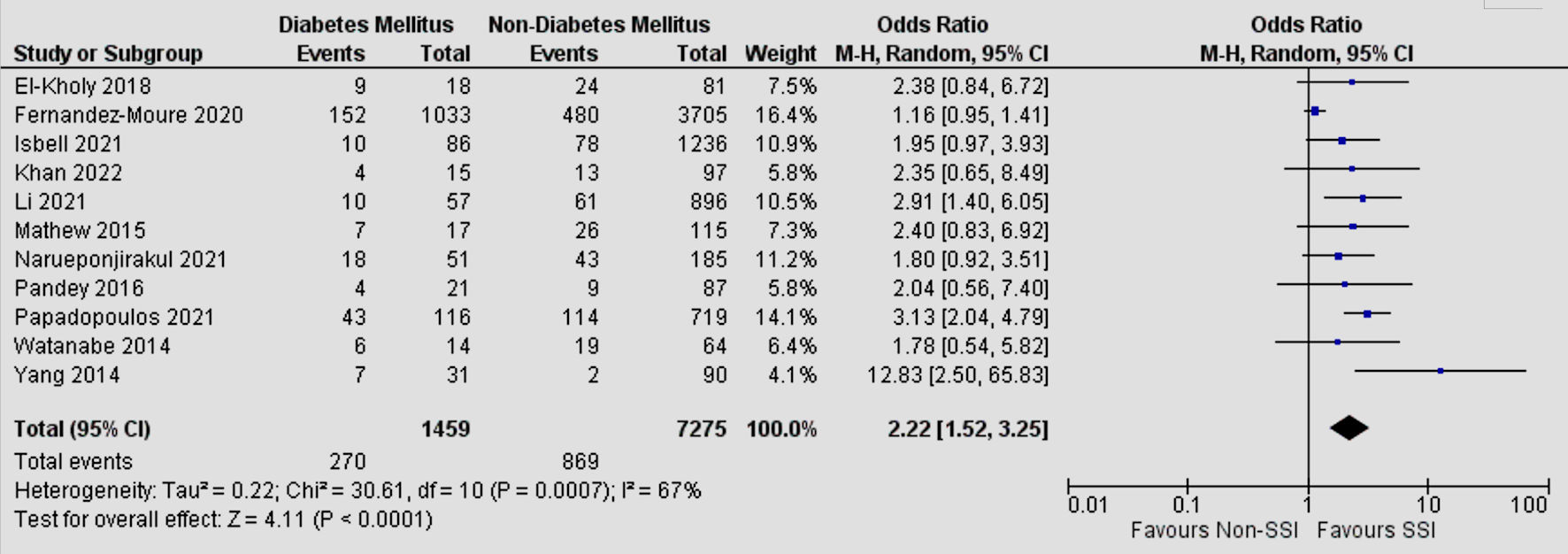 Click for large image | Figure 2. Forest plot of meta-analysis on the effect of diabetes mellitus on SSI. CI: confidence interval; SSI: surgical site infection. |
Hypertension
Four studies reported data on the comorbidity of hypertension. The incidence of SSI in the hypertension group was 14.0% (385 out of 2,747 patients), while in the non-hypertension group it was 12.0% (396 out of 3,292 patients). There was significant heterogeneity with an I2 of 62%. Analysis using a random-effects model (Fig. 3) showed that hypertension is not significantly associated with SSI in patients undergoing emergency surgery (OR = 0.95; 95% CI = 0.62 - 1.47; P = 0.82).
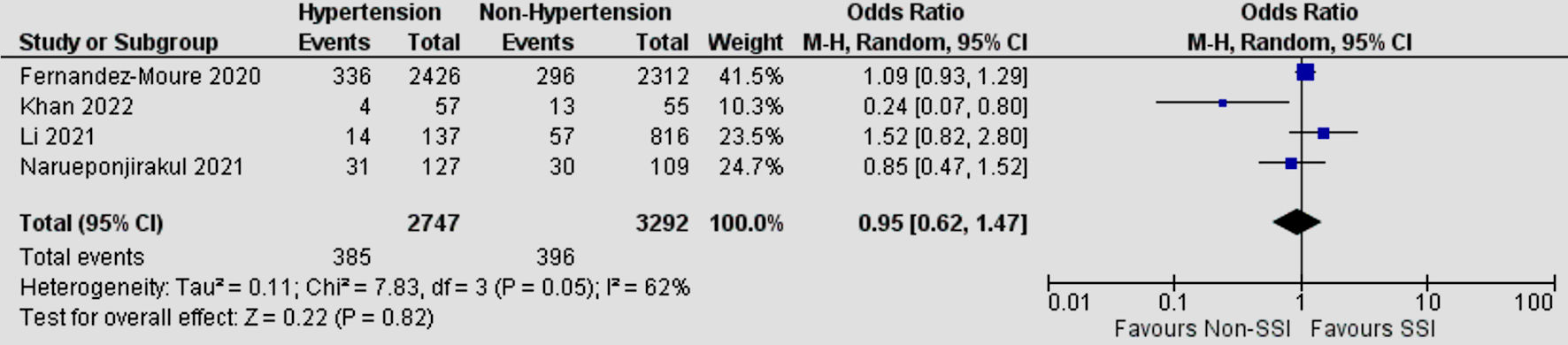 Click for large image | Figure 3. Forest plot of meta-analysis on the effect of hypertension on SSI. CI: confidence interval; SSI: surgical site infection. |
Obesity
Five studies reported data on the comorbidity of obesity. The incidence of SSI in the obesity group was 19.6% (208 out of 1,063 patients), while in the non-obesity group it was 13.5% (567 out of 4,204 patients). There was no significant heterogeneity with an I2 of 47%. Analysis using a fixed-effects model (Fig. 4) showed that obesity is significantly associated with SSI in patients undergoing emergency surgery (OR = 1.43; 95% CI = 1.19 - 1.72; P = 0.0001). This means that obese patients have a 1.43 times higher risk of developing SSI compared to non-obese patients.
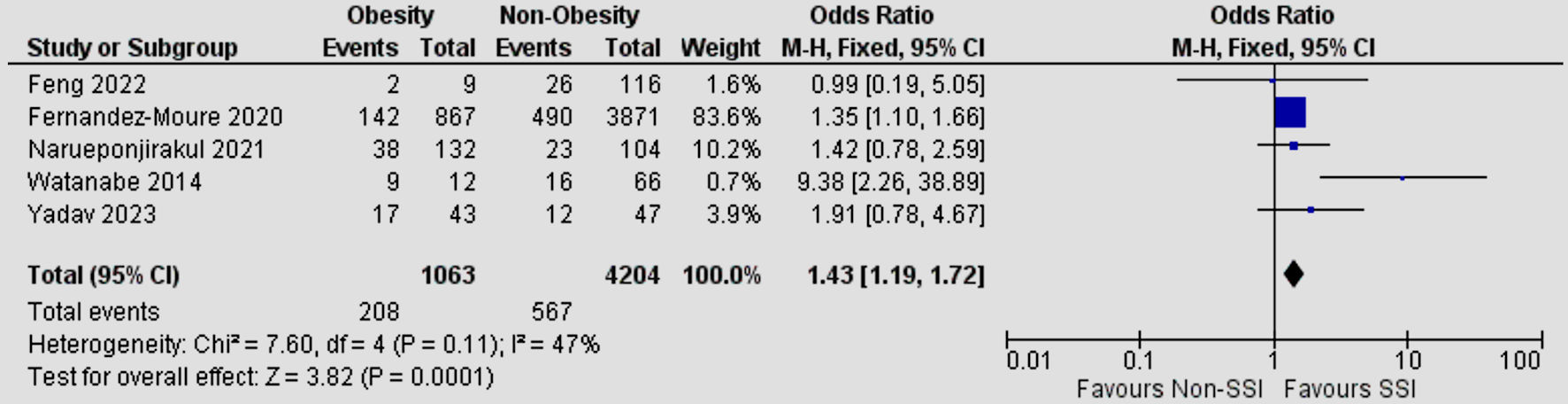 Click for large image | Figure 4. Forest plot of meta-analysis on the effect of obesity on SSI. CI: confidence interval; SSI: surgical site infection. |
Pulmonary disease
Four studies reported data on the comorbidity of pulmonary diseases. The incidence of SSI in the pulmonary disease group was 15.7% (229 out of 1,456 patients), while in the non-pulmonary disease group it was 13.0% (692 out of 5,306 patients). There was significant heterogeneity with an I2 of 64%. Analysis using a random-effects model (Fig. 5) showed that pulmonary diseases are not significantly associated with SSI in patients undergoing emergency surgery (OR = 1.39; 95% CI = 0.83 - 2.32; P = 0.21).
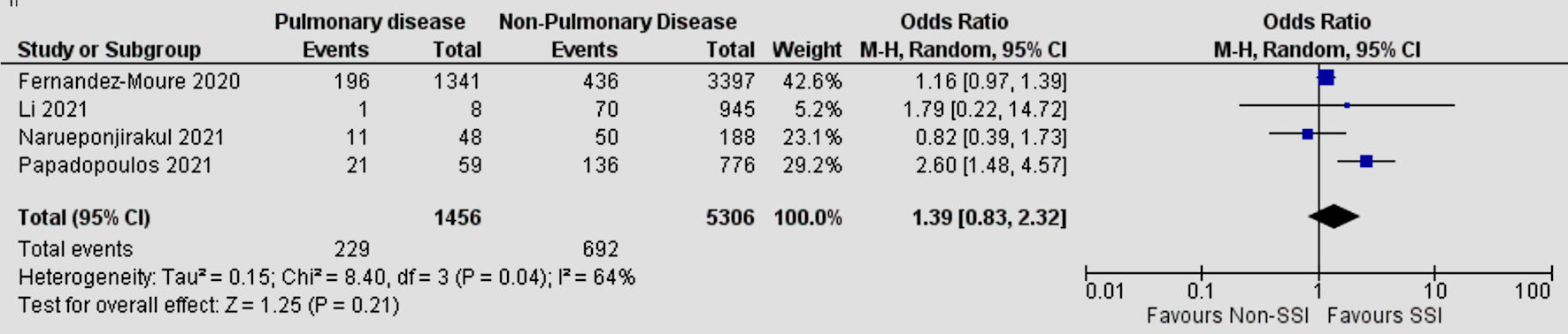 Click for large image | Figure 5. Forest plot of meta-analysis on the effect of pulmonary disease on SSI. CI: confidence interval; SSI: surgical site infection. |
Cardiac disease
Four studies reported data on the comorbidity of cardiac diseases. The incidence of SSI in the cardiac disease group was 16.8% (211 out of 1,254 patients), while in the non-cardiac disease group it was 12.9% (710 out of 5,508 patients). There was significant heterogeneity with an I2 of 61%. Analysis using a random-effects model (Fig. 6) showed that cardiac diseases are not significantly associated with SSI in patients undergoing emergency surgery (OR = 1.35; 95% CI = 0.90 - 2.01; P = 0.14).
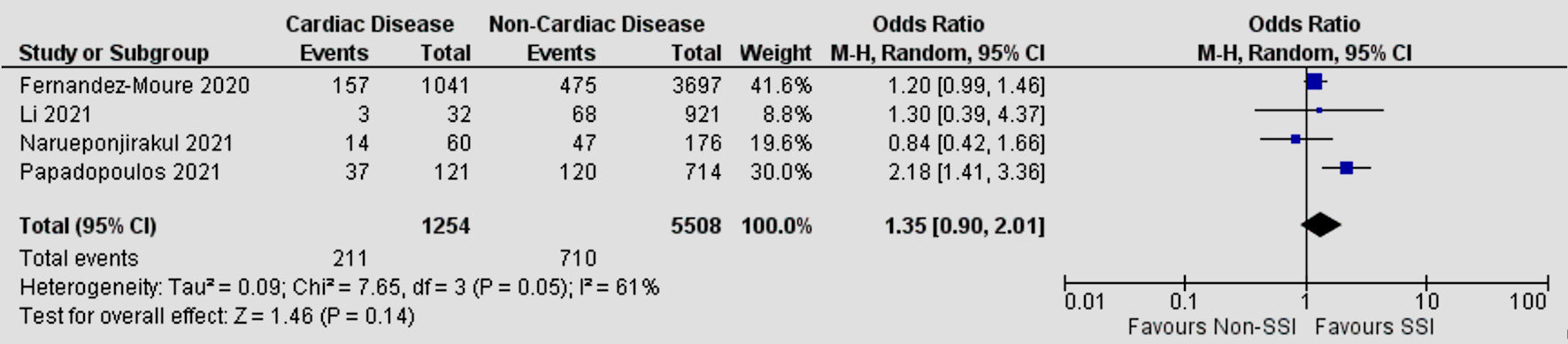 Click for large image | Figure 6. Forest plot of meta-analysis on the effect of cardiac disease on SSI. CI: confidence interval; SSI: surgical site infection. |
Liver disease
Three studies reported data on the comorbidity of liver diseases. The incidence of SSI in the liver disease group was 18.5% (173 out of 933 patients), while in the non-liver disease group it was 11.8% (591 out of 4,994 patients). There was no significant heterogeneity with an I2 of 0%. Analysis using a fixed-effects model (Fig. 7) showed that liver diseases are significantly associated with SSI in patients undergoing emergency surgery (OR = 1.66; 95% CI = 1.37 - 2.00; P < 0.00001). This means that patients with liver disease comorbidity have a 1.66 times higher risk of SSI compared to non-liver disease patients.
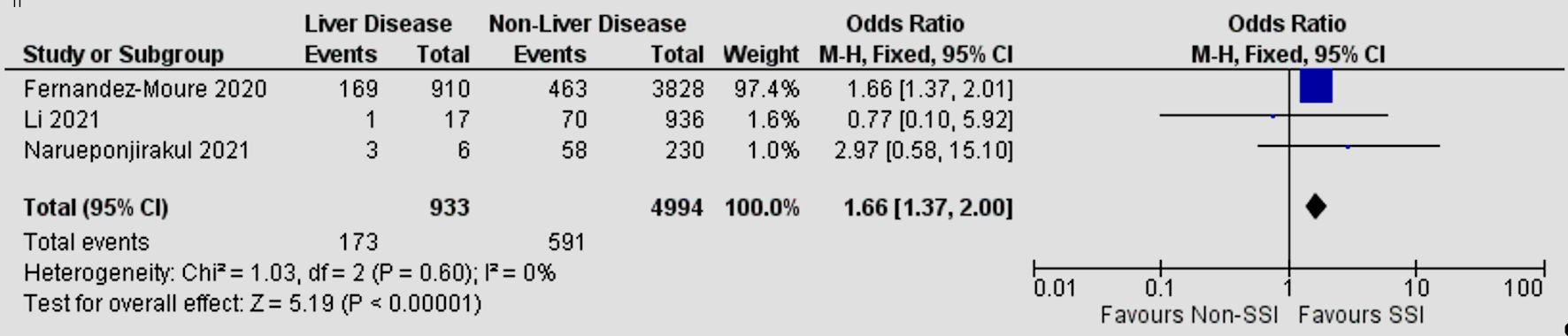 Click for large image | Figure 7. Forest plot of meta-analysis on the effect of liver disease on SSI. CI: confidence interval; SSI: surgical site infection. |
Renal disease
Four studies reported data on the comorbidity of renal disease. The incidence of SSI in the renal disease group was 14.1% (131 out of 929 patients), while in the non-renal disease group it was 13.3% (762 out of 5,729 patients). There was no significant heterogeneity with an I2 of 0%. Analysis using a fixed-effects model (Fig. 8) showed that renal disease is not significantly associated with SSI in patients undergoing emergency surgery (OR = 1.04; 95% CI = 0.85 - 1.28; P = 0.67).
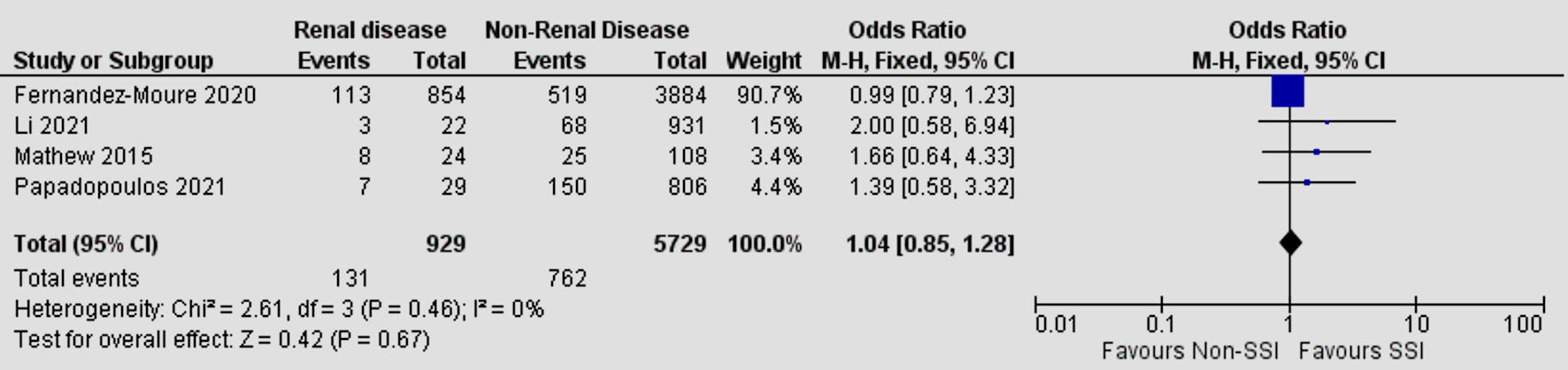 Click for large image | Figure 8. Forest plot of meta-analysis on the effect of renal disease on SSI. SSI: surgical site infection. |
| Discussion | ▴Top |
This systematic review and meta-analysis comprised 13 studies, encompassing a total of 8,952 patients undergoing emergency surgery. Our findings indicate that the presence of comorbidities such as diabetes mellitus, obesity, and liver disease heightens the risk of SSI subsequent to emergency surgery. However, hypertension, pulmonary disease, cardiac disease, and renal disease are not significantly associated with SSI. As far as we are aware, this study represents the first meta-analysis investigating the impact of comorbidities on SSI incidence among the distinct cohort of patients undergoing emergency surgery.
SSIs are often more common in emergency surgeries due to a confluence of factors. Contaminated or dirty wounds, frequently encountered in emergency cases resulting from traumatic injuries or acute conditions, create an optimal environment for bacterial colonization and subsequent infection [28]. Emergency surgeries often entail prolonged operative times as surgeons navigate intricate conditions or unforeseen complications, thereby heightening the likelihood of microbial contamination and subsequent SSIs. Moreover, emergency patients typically present with a higher burden of comorbidities, which can compromise immune function and wound healing, thereby further exacerbating the risk of SSIs [29]. Furthermore, the high American Society of Anesthesiologists (ASA) scores frequently observed in emergency settings reflect the overall health status and physiological reserve of patients, serving as predictors of surgical outcomes and complication rates, including SSIs [30].
Our meta-analysis revealed that diabetes mellitus carries nearly double the risk of developing SSI following emergency surgery. A meta-analysis study by Xu et al on patients undergoing colorectal surgery also reported that comorbid diabetes mellitus is significantly associated with an increased risk of SSI [31]. Diabetes mellitus can compromise the integrity of the immune system, making patients more susceptible to infections. Uncontrolled blood sugar levels in diabetes can impair the normal function of immune cells, including phagocytes, which are crucial in clearing pathogenic microorganisms from surgical wounds. Additionally, diabetes mellitus is often accompanied by vascular disorders that result in poor blood circulation. This can impede the supply of blood to the surgical site, reducing the body’s ability to effectively deliver immune substances and antibiotics to the wound area. This disrupted wound healing process creates an environment more conducive to bacterial growth and infection. High blood glucose levels can also create an environment supportive of bacterial growth [32].
We observed a significant 1.46-fold increase in SSI risk associated with obesity in patients undergoing emergency surgery, underscoring the need to address this risk factor in perioperative care. This finding is consistent with previous research by Liu et al, which also highlighted the elevated incidence of SSI among obese individuals compared to those with a normal body mass index [33]. Obesity is considered a comorbidity due to its association with various health conditions and its impact on physiological functions. It not only increases the risk of cardiovascular disease and diabetes mellitus but also heightens vulnerability to infections and slows wound healing, making it crucial in emergency surgery contexts. Obesity may compromise oxygen circulation to wounds due to adipose tissue impeding blood flow. This impaired oxygenation can hinder tissue healing processes and create an environment conducive to bacterial colonization and infection. Inadequate collagen synthesis in obese individuals may prolong the recovery process and increase susceptibility to infections [34]. Reduced antibiotic effectiveness in adipose tissues can further exacerbate SSI risk by promoting bacterial proliferation despite antimicrobial treatment. Moreover, obesity-related immune system dysregulation, characterized by chronic low-grade inflammation, may compromise the body’s ability to mount an effective defense against pathogens, increasing susceptibility to SSIs. Technical challenges during surgery in obese patients, such as difficulty accessing surgical sites and prolonged operative times, may also heighten the risk of contamination and subsequent SSIs [35].
Lastly, we found that liver disease significantly increases the risk of SSI by 1.66-fold. The liver plays a crucial role in the body’s metabolism and detoxification, and impaired liver function can result in a decreased ability of the body to fight off infections. Additionally, patients with chronic liver disease such as cirrhosis and hepatitis often experience decreased production of proteins, including those essential for wound healing processes and immune defense. This condition can slow down the healing process and increase vulnerability to infections in the surgical area. Moreover, liver dysfunction can also affect the function of the immune system, raising the risk of postoperative infection complications [36, 37].
While our meta-analysis findings indicated that comorbidities such as hypertension, pulmonary disease, cardiac disease, and renal disease were not significantly associated with SSI, it is crucial to interpret these results within a broader context. The lack of significant association does not necessarily imply that these factors do not impact infection risk. These results may be influenced by the relatively limited number of included studies. Additionally, the complex interplay of patient characteristics and clinical factors could contribute to the diversity in the reviewed study results. Therefore, further research considering other potential factors that may affect the relationship between comorbidities and SSI risk in patients undergoing emergency surgery is warranted.
The results of this meta-analysis have several important clinical implications. Firstly, the finding that comorbidities such as diabetes mellitus, obesity, and liver disease significantly increase the risk of SSI underscores the need for heightened vigilance in identifying and managing patients with these conditions before, during, and after emergency surgery. Secondly, implementing infection prevention measures, such as tight glycemic control in diabetic patients, stricter monitoring of surgical wound conditions in obese patients, and optimal supportive management in patients with liver diseases, can help reduce the risk of SSI. Thirdly, the use of antimicrobial agents in patients requiring emergency surgery, regardless of comorbidities, becomes critically important. Prophylactic administration of appropriate antibiotics can help mitigate the heightened risk of SSI. Therefore, tailored antimicrobial strategies should be integrated into perioperative care protocols to improve surgical outcomes. Fourthly, although our results indicate that other factors such as hypertension, pulmonary disease, cardiac disease, and kidney disease are not significantly associated with SSI, further research is needed to understand their potential roles more deeply. Therefore, integrating our findings into clinical practice can help improve perioperative management and outcomes for patients undergoing emergency surgery.
Study limitations
Our meta-analysis has several limitations. First, the studies included were sourced from only nine countries, which may limit the representativeness of the findings on a global scale. Second, the number of included studies is relatively small, with only 13 studies. Research examining the impact of comorbidities on the incidence of SSI in specific populations undergoing emergency surgery remains limited. Third, many of the included studies were retrospective cohort studies, which can introduce biases related to data collection and patient selection. Future research should focus on larger, well-designed studies to confirm these findings and provide more precise estimates of the effect of comorbidities on the incidence of SSI in emergency surgery patients.
Conclusions
In summary, this systematic review and meta-analysis found that among patients undergoing emergency surgery, the presence of comorbidities such as diabetes mellitus, obesity, and liver disease increases the incidence of developing SSI. Healthcare providers should heighten vigilance in identifying and managing patients with these risk factors. These high-risk patients require more careful monitoring and management before, during, and after surgery.
Acknowledgments
We would like to thank Institut Kesehatan Helvetia for the support of this research.
Financial Disclosure
The authors received no financial support for the research or publication of this manuscript.
Conflict of Interest
The authors declare that there is no conflict of interest in the publication of this manuscript.
Informed Consent
Not applicable.
Author Contributions
AA, JH, and HAW contributed to developing the study’s concept and design, conducting the systematic literature search, analyzing the data, performing statistical analysis, and drafting the manuscript. RBS and AHH supervised the study and provided critical intellectual input during manuscript revision. All authors have approved the final version of the manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Borchardt RA, Tzizik D. Update on surgical site infections: the new CDC guidelines. JAAPA. 2018;31(4):52-54.
doi pubmed - Sattar F, Sattar Z, Zaman M, Akbar S. Frequency of post-operative surgical site infections in a tertiary care hospital in Abbottabad, Pakistan. Cureus. 2019;11(3):e4243.
doi pubmed pmc - Kolasinski W. Surgical site infections - review of current knowledge, methods of prevention. Pol Przegl Chir. 2018;91(4):41-47.
doi pubmed - Misha G, Chelkeba L, Melaku T. Bacterial profile and antimicrobial susceptibility patterns of isolates among patients diagnosed with surgical site infection at a tertiary teaching hospital in Ethiopia: a prospective cohort study. Ann Clin Microbiol Antimicrob. 2021;20(1):33.
doi pubmed pmc - Eckmann C, Kramer A, Assadian O, Flessa S, Huebner C, Michnacs K, Muehlendyck C, et al. Clinical and economic burden of surgical site infections in inpatient care in Germany: A retrospective, cross-sectional analysis from 79 hospitals. PLoS One. 2022;17(12):e0275970.
doi pubmed pmc - Syaiful RA, Mazni Y, Prasetyo ML, Lalisang TJM. Surgical site infection after digestive surgery in a single tertiary hospital in indonesia: six years of data. Med J Indones. 2020;29(3):310-315.
- Barie PS, Eachempati SR. Surgical site infections. Surg Clin North Am. 2005;85(6):1115-1135.
doi pubmed - Ansari S, Hassan M, Barry HD, Bhatti TA, Hussain SZM, Jabeen S, Fareed S. Risk factors associated with surgical site infections: a retrospective report from a developing country. Cureus. 2019;11(6):e4801.
doi pubmed pmc - Wong K, Holloway S. An observational study of the surgical site infection rate in a general surgery department at a general hospital in Malaysia. Wounds Int. 2019;10(3):13-21.
- Piednoir E, Robert-Yap J, Baillet P, Lermite E, Christou N. The socioeconomic impact of surgical site infections. Front Public Health. 2021;9:712461.
doi pubmed pmc - Korol E, Johnston K, Waser N, Sifakis F, Jafri HS, Lo M, Kyaw MH. A systematic review of risk factors associated with surgical site infections among surgical patients. PLoS One. 2013;8(12):e83743.
doi pubmed pmc - Alfonso-Sanchez JL, Martinez IM, Martin-Moreno JM, Gonzalez RS, Botia F. Analyzing the risk factors influencing surgical site infections: the site of environmental factors. Can J Surg. 2017;60(3):155-161.
doi pubmed pmc - Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
doi pubmed pmc - Wells GA, Shea B, O’Connel, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses [Internet]. 2011 [cited May 15, 2024]. Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
- El-Kholy AA, Elanany MG, Sherif MM, Gad MA. High prevalence of VIM, KPC, and NDM expression among surgical site infection pathogens in patients having emergency surgery. Surg Infect (Larchmt). 2018;19(6):629-633.
doi pubmed - Fernandez-Moure JS, Wes A, Kaplan LJ, Fischer JP. Actionable risk model for the development of surgical site infection after emergency surgery. Surg Infect (Larchmt). 2021;22(2):168-173.
doi pubmed - Isbell KD, Hatton GE, Wei S, Green C, Truong VTT, Woloski J, Pedroza C, et al. Risk stratification for superficial surgical site infection after emergency trauma laparotomy. Surg Infect (Larchmt). 2021;22(7):697-704.
doi pubmed pmc - Khan SI, Khan S, Hossain MM, Talukder IH, Ali M. Incidence and etiology of abdominal surgical site infections among emergency postoperative patients in a tertiary medical college hospital, Faridpur, Bangladesh. IP J Surg Allied Sci. 2022;4(2):49-55.
- Li Z, Li H, Lv P, Peng X, Wu C, Ren J, Wang P. Prospective multicenter study on the incidence of surgical site infection after emergency abdominal surgery in China. Sci Rep. 2021;11(1):7794.
doi pubmed pmc - Mathew JD, Kalaivani R, Ganesh Babu CP. A prospective study on various factors influencing post-operative wound infection in emergency surgeries. J Patient Saf Infect Control. 2015;3(3):121-125.
- Narueponjirakul N, Breen KA, El Hechi MW, Kongkaewpaisan N, Velmahos G, King D, Fagenholz P, et al. Abdominal wall thickness predicts surgical site infection in emergency colon operations. J Surg Res. 2021;267:37-47.
doi pubmed - Pandey HC. An observational study of incidence and pattern of surgical site infections in emergency surgeries. J Med Sci Clin Res. 2016;04(11):13686-13691.
- Papadopoulos A, Machairas N, Tsourouflis G, Chouliaras C, Manioti E, Broutas D, Kykalos S, et al. Risk factors for surgical site infections in patients undergoing emergency surgery: a single-centre experience. In Vivo. 2021;35(6):3569-3574.
doi pubmed pmc - Watanabe M, Suzuki H, Nomura S, Maejima K, Chihara N, Komine O, Mizutani S, et al. Risk factors for surgical site infection in emergency colorectal surgery: a retrospective analysis. Surg Infect (Larchmt). 2014;15(3):256-261.
doi pubmed - Yang L, Wang H, Liang X, Chen T, Chen W, Song Y, Wang J. Bacteria in hernia sac: an important risk fact for surgical site infection after incarcerated hernia repair. Hernia. 2015;19(2):279-283.
doi pubmed - Feng S, Xie X, An W, Gao B. Risk factors and outcome analysis of surgical site infections in Chinese elderly patients with intestinal obstruction after emergency surgery. SN Compr Clin Med. 2022;4(1):222.
- Yadav AP, Rauniyar CS, Joshi M, Singh A, Shrestha B. Factor responsible for surgical site infection following emergency non-traumatic abdominal surgery. Med Phoenix. 2023;8(1):7-10.
- De Simone B, Sartelli M, Coccolini F, Ball CG, Brambillasca P, Chiarugi M, Campanile FC, et al. Intraoperative surgical site infection control and prevention: a position paper and future addendum to WSES intra-abdominal infections guidelines. World J Emerg Surg. 2020;15(1):10.
doi pubmed pmc - Jatoliya H, Pipal RK, Pipal DK, Biswas P, Pipal VR, Yadav S, Verma B, et al. Surgical site infections in elective and emergency abdominal surgeries: a prospective observational study about incidence, risk factors, pathogens, and antibiotic sensitivity at a government tertiary care teaching hospital in India. Cureus. 2023;15(10):e48071.
doi pubmed pmc - Bhat RA, Isaac NV, Joy J, Chandran D, Jacob KJ, Lobo S. The effect of American society of anesthesiologists score and operative time on surgical site infection rates in major abdominal surgeries. Cureus. 2024;16(2):e55138.
doi pubmed pmc - Xu Z, Qu H, Gong Z, Kanani G, Zhang F, Ren Y, Shao S, et al. Risk factors for surgical site infection in patients undergoing colorectal surgery: a meta-analysis of observational studies. PLoS One. 2021;16(10):e0259107.
doi pubmed pmc - Martin ET, Kaye KS, Knott C, Nguyen H, Santarossa M, Evans R, Bertran E, et al. Diabetes and risk of surgical site infection: a systematic review and meta-analysis. Infect Control Hosp Epidemiol. 2016;37(1):88-99.
doi pubmed pmc - Liu J, Li G, Chen Z, Jiang H. A meta-analysis of the effect of different body mass index on surgical wound infection after colorectal surgery. Int Wound J. 2023;20(6):2151-2158.
doi pubmed pmc - Cotterell A, Griffin M, Downer MA, Parker JB, Wan D, Longaker MT. Understanding wound healing in obesity. World J Exp Med. 2024;14(1):86898.
doi pubmed pmc - Qiao Y, Zhang T, Bai T, Peng X, Lin H, Zhang A. Effect of body mass index on surgical site wound infection, mortality, and postoperative hospital stay in subjects undergoing possibly curative surgery for colorectal cancer: A meta-analysis. Int Wound J. 2023;20(1):164-172.
doi pubmed pmc - Gilbert-Kawai N, Hogan B, Milan Z. Perioperative management of patients with liver disease. BJA Educ. 2022;22(3):111-117.
doi pubmed pmc - Lin X, Su J, Yang Z. Optimising wound care for patients with cirrhosis: A study of the effect of combination therapy on wound healing. Int Wound J. 2024;21(2):e14727.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.