| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://jocmr.elmerjournals.com |
Original Article
Volume 16, Number 7-8, August 2024, pages 335-344
Preoperative Autologous Blood Donation for Rh-Negative Pregnant Women Undergoing Cesarean Sections
Siriwan Wannoona , Parinya Saringkananb
, Rachasak Boonhokc, d
, Nateelak Kooltheate, d
, Nurdina Charonge, d, f
aDepartment of Medical Technology and Clinical Pathology, Takuapa Hospital, Phang Nga, Thailand
bDepartment of Obstretics and Gynecology, Takuapa Hospital, Phang Nga, Thailand
cSchool of Allied Health Sciences, and Research Excellence Center for Innovation and Health Products (RECIHP), Walailak University, Nakhon Si Thammarat, Thailand
dDepartment of Medical Technology, Walailak University, Nakhon Si Thammarat 80161, Thailand
eSchool of Allied Health Sciences, and Hematology and Transfusion Science Research Center, Walailak University, Nakhon Si Thammarat, Thailand
fCorresponding Author: Nurdina Charong, Department of Medical Technology, Walailak University, Nakhon Si Thammarat 80161, Thailand
Manuscript submitted June 7, 2024, accepted July 31, 2024, published online August 12, 2024
Short title: Transfusion for Rh-Negative C-Section
doi: https://doi.org/10.14740/jocmr5227
| Abstract | ▴Top |
Background: Cesarean sections (C-section) often require blood transfusions in cases of severe bleeding, particularly challenging in Rh-negative pregnancies due to the scarcity of Rh-negative donors, with only approximately 0.3% of the population in Thailand. Autologous blood donation, where individuals donate their own blood before surgery, offers a promising solution. Our study focused on preparing preoperative autologous blood donations (PAD) for Rh-negative pregnancies.
Methods: We conducted blood screening on 7,182 pregnancies at Takuapa Hospital from October 2013 to September 2018, identifying 21 Rh-negative pregnant women. We established criteria based on hemoglobin (Hb) levels, which are crucial for autologous blood preparation (Hb at 11.0 g/dL, and hematocrit (Hct) above 33%). Blood samples were collected twice during pregnancy, at 36 and 37 weeks, with the second collection 1 week before the C-section. Pregnancies testing positive for infectious markers were excluded following standard blood donation guidelines. Twelve pregnant women testing negative for infectious markers were enrolled.
Results: The demographic data showed 12 subjects aged 17 to 41 years, with an average of 27.83. Initial blood tests indicated Hb and Hct levels of 12.5 g/dL, and 36.4%, slightly decreasing to 12.2 g/dL and 35.8% in the second collection. On the day of the cesarean, levels further declined to 11.6 g/dL and 34.4%, respectively, within normal ranges. At discharge, the Hct measured 34.8%. Maternal and infant health post-C-section were good, with baby weights ranging from 2,640 to 4,080 g. None of the 12 cases required autologous blood transfusion, validating the safety of standard autologous blood preparation practices.
Conclusions: This study highlights the safety of autologous blood donation for pregnant women with rare blood types, which was achieved through effective planning and collaboration among hospital departments. These findings can serve as a model for other hospitals and significantly reduce the burden of searching for Rh-negative donors.
Keywords: Autologous blood; Rh negative; PAD; Hemoglobin; Hematocrit; Cesarean section
| Introduction | ▴Top |
Cesarean section (C-section) rates continue to rise globally in modern childbirth, as it offers the advantage of determining the delivery duration and often requires less time compared to natural childbirth [1]. In addition, a C-section can save a mother and baby from unnecessary risk of short- and long-term health problems [2, 3]. In every surgical procedure, the request for a few units of blood or preoperative autologous blood donations (PAD) serves as a preventive measure, anticipating emergencies and aiming to safeguard the mother’s life from severe blood loss during or after the surgery, a condition referred to as postpartum hemorrhage (PPH) [4]. Nevertheless, for pregnant women who have developed alloantibodies, such as those with anti-PP1PK or those possessing rare blood types like Rh-negative or the Bombay phenotype, finding compatible blood presents greater complexity and difficulty compared to individuals with more common blood types [5-7]. The concept of autologous blood donation, collecting a patient’s own blood for later reinfusion, gained substantial attention and advancements during the 1970s and 1980s and gained acceptance as a standard practice within specific elective surgical settings by 1993 [8, 9]. The process provides several advantages such as to treat surgical blood loss in very specific situations and to decrease risk of transfusion-transmitted disease, transfusion reaction and alloimmunization [10]. Additionally, given the limited availability of allogeneic blood supply resulting from the coronavirus disease 2019 (COVID-19) pandemic, utilizing autologous blood transfusion presents an alternative to allogeneic transfusion. This helps prevent the delay of numerous surgeries caused by the scarcity of blood during this crucial period [11]. Therefore, autologous blood preparation is primarily undertaken because obtaining compatible allogeneic blood poses significant challenges. Nowadays, the method has been developed based on the American Association of Blood Banks (AABB) standard and applied in many hospitals worldwide [12-14].
In Thailand, autologous blood donation is not widely practiced due to concerns about potential hemoglobin (Hb) decline, particularly when adequate specialized care from hospital medical staff is lacking. It is mainly performed in central hospitals, where clear donation criteria and post-donation care are established. The process is uncommon in regional hospitals due to concerns about post-donation complications. For Rh D-negative patients, this increases C-section risks. If Rh-negative blood is unavailable in an emergency, Rh-positive blood can be given if no anti-D is detected. However, for future transfusions, only Rh-negative blood can be used to avoid life-threatening reactions. This study collected the retrospective data on autologous donation among Rh-negative pregnant women, who was scheduled for C-section at Takuapa Hospital during the past 5 years. Due to the increased number of pregnancies with Rh-negative blood at the hospital, coupled with the difficulty of finding Rh-negative donors, the autologous blood preparation protocol has been revived and implemented for pregnant women. The process of preparing patients for blood collection was established, and their Hb and hematocrit (Hct) levels before and after donation were monitored to develop appropriate and standardized guidelines for autologous donation in pregnant women. This initiative aimed to create guidelines for autologous blood preparation in pregnant women with rare blood groups, such as Rh-negative, or those who produce clinically significant antibodies, such as anti-PP1PK and anti-U. The criteria of donor preparation and donor unit blood testing were developed in accordance with AABB standard and are based on the safety of the mother and newborn for widespread clinical use.
| Materials and Methods | ▴Top |
Patient selection
This study is a descriptive and retrospective investigation approved by the Ethics Committee of the Phangnga Provincial Public Health Office (AF 04-08/02.0). The subjects were pregnant women with a special blood type, Rh-negative, who underwent C-sections at Takuapa Hospital, Phang Nga Province, between October 1, 2013, and September 30, 2018. Selected pregnant patients eligible for autologous blood donation must have Rh-negative blood group with the following blood parameters: Hb ≥ 11 g/dL and Hct ≥ 33%, along with other general health checks according to the Thai Red Cross blood donation standards. If the patient does not meet these eligibility criteria, she will not be accepted for autologous blood preparation, and allogenic donated blood will be provided instead.
Institutional Review Board approval
The protocol was approved by Research Ethical Review Board of Phangnga Provincial Public Health Office, Ministry of Public Health of Thailand. The study was conducted in compliance with the ethical standards of the responsible institution on human subjects, in accordance with the Belmont Report, Nuremberg Code, Declaration of Helsinki, and the Medical Council Regulations on the Ethics of the Medical Profession 2006.
Study design
Blood group testing for ABO and Rh was conducted on 7,182 pregnancies at Takuapa Hospital between October 2013 and September 2018. Among these, 7,161 were Rh-positive, and 21 were Rh-negative. Rh-positive pregnancies underwent standard prenatal care procedures, while Rh-negative ones were designated for childbirth decision. In cases of C-section, extensive psychological preparation was provided through counseling sessions to educate expectant mothers about donor procedures and the option of self-donated blood. All participants met the minimum weight requirement for autologous donation, which is 50 kg. Blood samples were collected to measure Hb and Hct levels using hematology autoanalyzer Sysmex XN-2000 (Sysmex, Kobe, Japan). The criteria for these factors were set at Hb ≥ 11.0 g/dL or Hct above 33%. Pregnant women whose levels fell below these criteria were encouraged to undergo allogeneic blood donation, while those meeting or exceeding the criteria were eligible for autologous blood donation. Blood collection occurred twice during pregnancy, at 36 and 37 weeks, with the second collection taking place 1 week before the scheduled C-section. Pregnancies with positive infectious markers were excluded according to standard guidelines for blood donation and study criteria. Twelve pregnant women with negative infectious markers were enrolled in the study (Fig. 1). All methods and results have been reported in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.
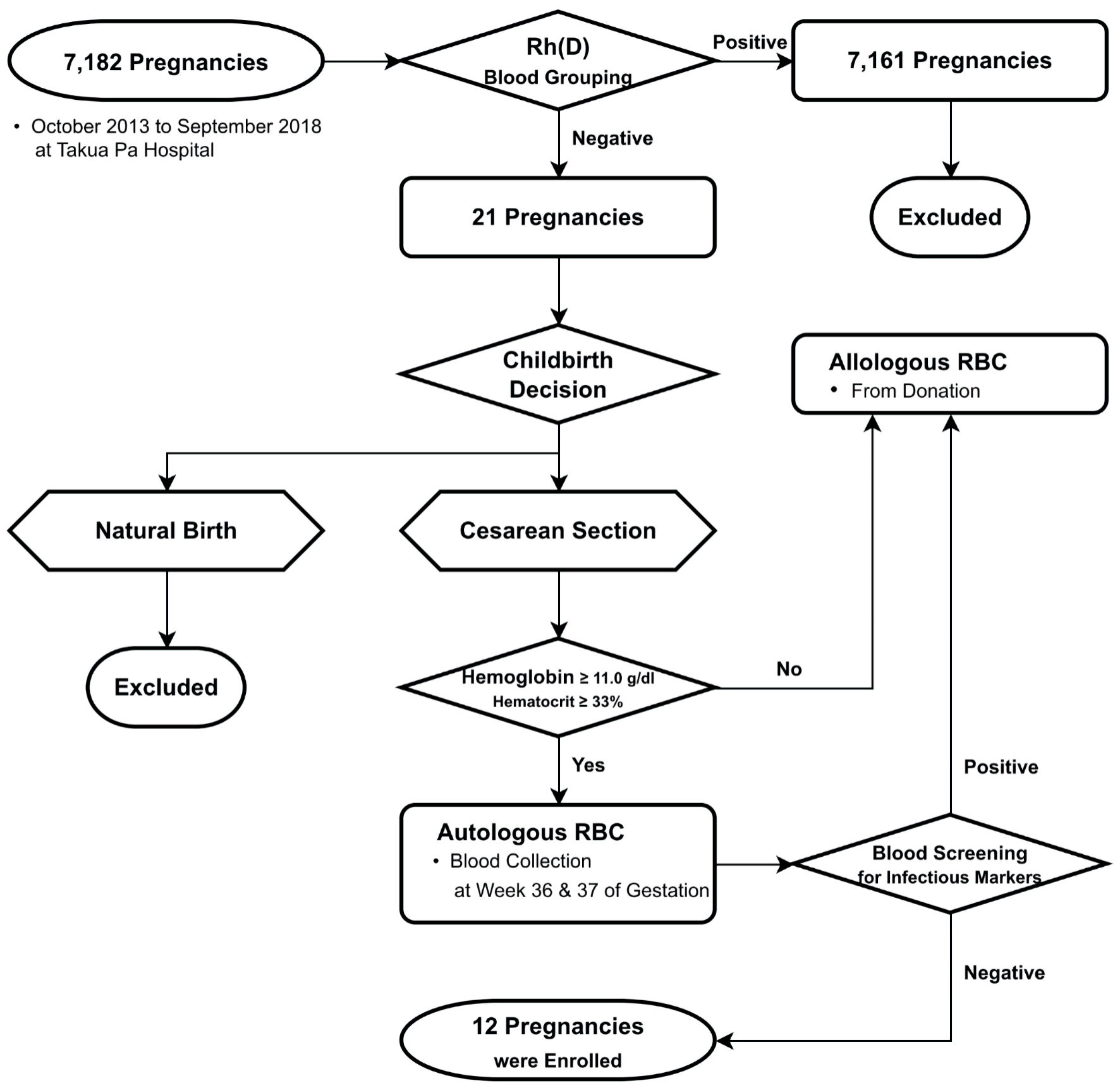 Click for large image | Figure 1. Flowchart illustrating the selection process for pregnancies enrolled in the autologous blood donation program. RBC: red blood cell. |
Statistical analysis
All demographic characteristic data were analyzed by GraphPad (Prism 5) software for mean, and one-way analysis of variance (ANOVA) was performed to test the mean difference of Hb or Hct level at each time point. A P < 0.05 was considered statistically significant for all parameters.
| Results | ▴Top |
History, demographic and clinical characteristics of participants enrolled in the study
The medical records of 12 Rh-negative pregnant women, who received antenatal care at Takuapa Hospital in PhangNga province, Thailand, are summarized in Table 1. This includes age, ABO blood group, Rh blood group, gender of the baby, and baby weight. The age range of participants is between 17 and 41 years, with a mean age of 27.83 years. Among the participants, the highest percentage had blood group O (41.67%), followed by A (25.00%), B (25.00%), and AB (8.33%) (Table 2). According to the World Health Organization (WHO) body mass index (BMI) categories [15], the distribution was as follows: normal weight (33.33%), overweight (50%), and obesity class I (16.67%) (Table 2). The babies were delivered via C-section from 12 Rh-negative mothers, with six girls and six boys. The range of baby weight is between 2,640 and 4,080 g, with a mean weight of 3,216 g (Table 3).
 Click to view | Table 1. History of Participants Enrolled in the Study at Takuapa Hospital, PhangNga, Thailand |
 Click to view | Table 2. Participating Pregnancy Demographics at Takuapa Hospital, PhangNga, Thailand |
 Click to view | Table 3. Baby Demographics of the Participating Pregnancies |
Hb and Hct levels during and after autologous blood donation
Hb and Hct levels were measured in 12 Rh-negative pregnancies at three different time points: 2 weeks and 1 week prior to the C-section, followed by a measurement during the C-section Additionally, Hct levels were monitored for 1 week post-C-section, on the discharge day. At 2 weeks, pre-C-section, initial Hb values ranged from 12.0 g/dL to 13.4 g/dL, with a mean Hb of 12.53 ± 0.39 g/dL. One week before the cesarean, the Hb range was 11.0 g/dL to 13.3 g/dL, with a mean of 12.2 ± 0.71 g/dL (Table 4). On the day of the cesarean, the mean Hb level declined to 11.58 g/dL, indicating a statistically significant difference (P = 0.0435) compared with 1 week before the cesarean but still above the minimum level of 11.0 g/dL [16] (Fig. 2a). The Hct levels 2 weeks and 1 week before the C-section ranged from 34.2% to 38.7% and 33.0% to 38.8%, respectively, with means of 36.42±1.30% and 35.80±1.90%. On the day of the cesarean, the mean Hct level decreased to 34.43%. Significant differences were observed only when compared to the 2-week pre-C-section level (P = 0.0248). On discharge day, 1-week post-C-section, the mean Hct was 34.83%, which is normal for pregnant women (Table 4). Between 2 weeks pre-C-section and the day of C-section, Hb and Hct levels showed a slight but significant decrease (P = 0.006 and P = 0.0248, respectively), while remaining within the minimum range. There was no significant difference in Hct levels on the day of discharge (Fig. 2b). Post-C-section, both mothers and babies were healthy, with baby weights ranging from 2,640 g to 4,080 g (Table 3). Takuapa Hospital successfully reduced the procurement of Rh-negative blood for pregnant women undergoing C-sections by 57.1% (data not shown).
 Click to view | Table 4. Levels of Hemoglobin and Hematocrit Measured at Different Time Points |
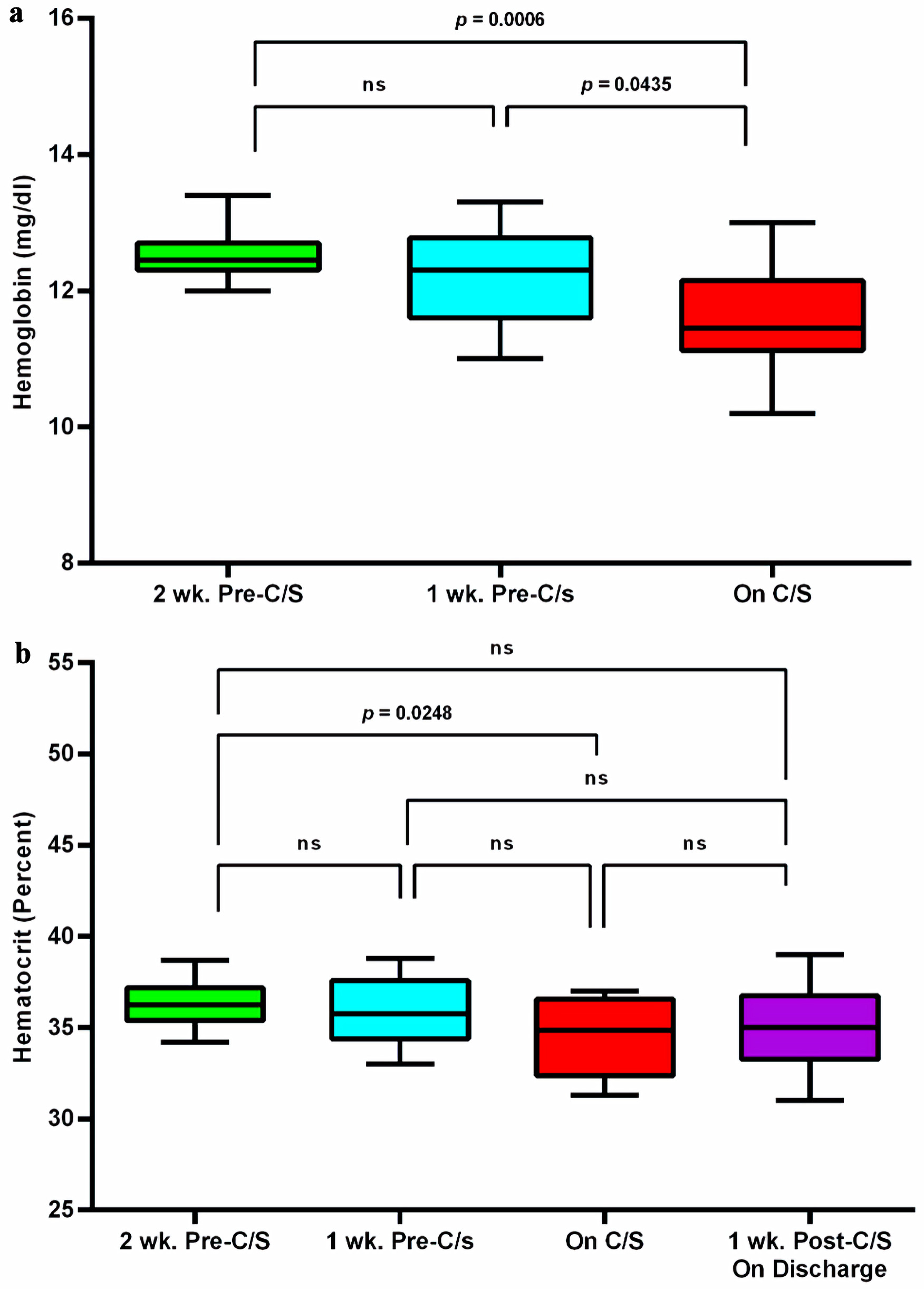 Click for large image | Figure 2. Hemoglobin (a) and hematocrit (b) levels were measured at three different time points: 2 weeks and 1 week before the C-section, during the C-section, and after the C-section. C/S: C-section; wk: week; C-section: cesarean sections. |
| Discussion | ▴Top |
Our study reported the successful implementation of guidelines for autologous blood collection from Rh-negative pregnant women at Takuapa Hospital in Phang Nga Province, Thailand, maintaining acceptable Hct levels until delivery. Additionally, this study highlights PAD for C-sections, which typically involve greater blood loss compared to vaginal deliveries. Although autologous blood transfusion is used in Thailand, its adoption varies by region and healthcare facility, which is influenced by factors such as hospital resources, medical protocols, and patient preferences. Obstetricians often prepare two units of blood reserves. Patients with common blood types can use the type and screen method or cross-matching from the blood bank. However, blood banks across the country frequently encounter difficulties in meeting the demand for specialized blood types like Rh-negative or for patients with specific alloantibodies [17-19]. In Thailand, since the prevalence of Rh-negative blood type is relatively low compared to Rh-positive blood types, pregnant patients with Rh-negative blood types require specific donor reserves, which can be challenging to procure [20]. Therefore, PAD serves as an effective solution to ensure the safety of both mother and fetus.
Takuapa Hospital has established criteria for autologous blood donation, particularly for pregnant women with Rh-negative blood types. The hospital has a structured pregnancy care pathway, requiring multiple visits to prepare blood for safe transfusions. We implemented PAD for 12 Rh-negative pregnancies where the patients chose to have a C-section. Patients’ Hb and Hct levels are typically monitored to assess their blood’s ability to carry oxygen adequately, and these levels should remain within normal ranges before and after autologous blood donation, transfusion, and discharge [21]. A drop in Hb and Hct levels below specific thresholds may indicate anemia or inadequate oxygen transport, potentially necessitating a blood transfusion. Identifying such levels before donation could render the patient unsuitable for PAD. Guidelines for blood donation, health records, and childbirth records were prepared. Previous studies indicate that autologous blood donation is feasible and safe for pregnant Japanese women and their infants. Despite the controversial indications, autologous blood donation should be considered in cases of placenta previa [22]. This technique is also safe for patients undergoing intracranial surgery and has been shown to be more cost-effective than allogenic blood transfusions [23]. Among the 12 Rh-negative patients, none had a history of smoking or comorbidities, and all were free of hemorrhagic risk factors such as preeclampsia, emergency C-sections, or previous abdominal surgery.
Blood collection was performed twice, with each session yielding 350 mL, separated by 1 week. If Hb and Hct levels fell below the criteria during the second collection, the second blood bag was not collected. The mean reported blood loss during delivery for pregnant women at the University Hospital in Japan was 1,976 ± 1,654 mL. The recommended range for donated blood volume typically spans from 400 to 2,000 mL [24]. Gari et al revealed that mathematical calculations tend to overestimate blood loss during C-sections, while obstetricians tend to underestimate it [25]. However, the amount of blood loss can vary significantly, ranging from below 500 mL to above 1,000 mL [26]. This variation in blood loss can influence the decision to proceed with a blood transfusion, especially if the blood loss exceeds this range or if the patient shows signs of significant anemia or has preoperative anemia [27]. Improving maternal Hb levels during pregnancy could potentially decrease the occurrence of blood transfusions related to C-sections [28]. On the day of surgery, certain pregnant women (subjects 7, 8, 10, and 12) had Hb or Hct levels below the standard for blood collection but within the safe range for surgery without additional care. This is likely due to pregnancy-related factors that increase the demand for iron, especially during the second trimester leading up to delivery [29]. The BMI of these individuals fell into both the normal and overweight categories. Importantly, on the day of surgery, no blood collection was performed, with only monitoring for potential postoperative blood loss to determine the necessity of a transfusion. After completing the surgery, the physician conducted wound inspection and confirmed no PPH within the first 24 h (assessed by monitoring for Hct ≤ 33%). If the patient appeared pale beforehand, closer monitoring was implemented. In all 12 cases included in this study, an autologous blood transfusion was unnecessary, confirming the safety of standard autologous blood preparation procedures. Additionally, wound inspection revealed no signs of infection. Interestingly, nowadays there are comprehensive strategies that incorporate multiple effective measures to manage PPH. Incorporating tranexamic acid (TA) into a comprehensive strategy for managing PPH after C-section, alongside other proven measures, could potentially improve outcomes [30].
From this study, we have developed a flowchart outlining the pregnancy care pathway in the Obstetrics and Gynecology Department, as depicted in Figure 3. Prior to delivery, patients make multiple visits to the hospital for blood preparation. Hospitals with robust teams ensure the safety of blood transfusions. Initial examinations with an obstetrician/gynecologist (OB/GYN) are conducted at 8 - 12 weeks of pregnancy. Upon pregnancy confirmation, they are referred for further obstetrical assessments, and health parameters are evaluated in the medical lab. Subsequent visits are scheduled for 24 - 26, 30 - 32, and 36 - 38 weeks to monitor health parameters. By the third visit, childbirth decisions and emergency plans are discussed in preparation for delivery. Figure 4 illustrates childbirth decisions and preparations for autologous blood donation in pregnancies with rare blood types like Rh-negative. At 30 - 32 weeks, pregnant women preferring a C-section will have bloodwork for ABO and Rh typing. If the patient is Rh-negative, an Hb test is conducted to check for anemia. With Hb above 11 g/dL, autologous blood donation is considered; if below 11 g/dL, allogenic RBC transfusion is prepared. Blood collection for crossmatching occurs at 36 - 37 weeks. Incompatible units are replaced, and compatible ones are prepared for transfusion during delivery at 38 - 41 weeks. Hb levels guide whether the collected blood is used or monitored, and postpartum care is provided as needed. The physician will determine the hospital’s discharge timing. A study by Yamada et al recommends starting blood collection at 32 weeks with weekly 400 mL phlebotomies to store 1,200 - 1,500 mL of blood [31].
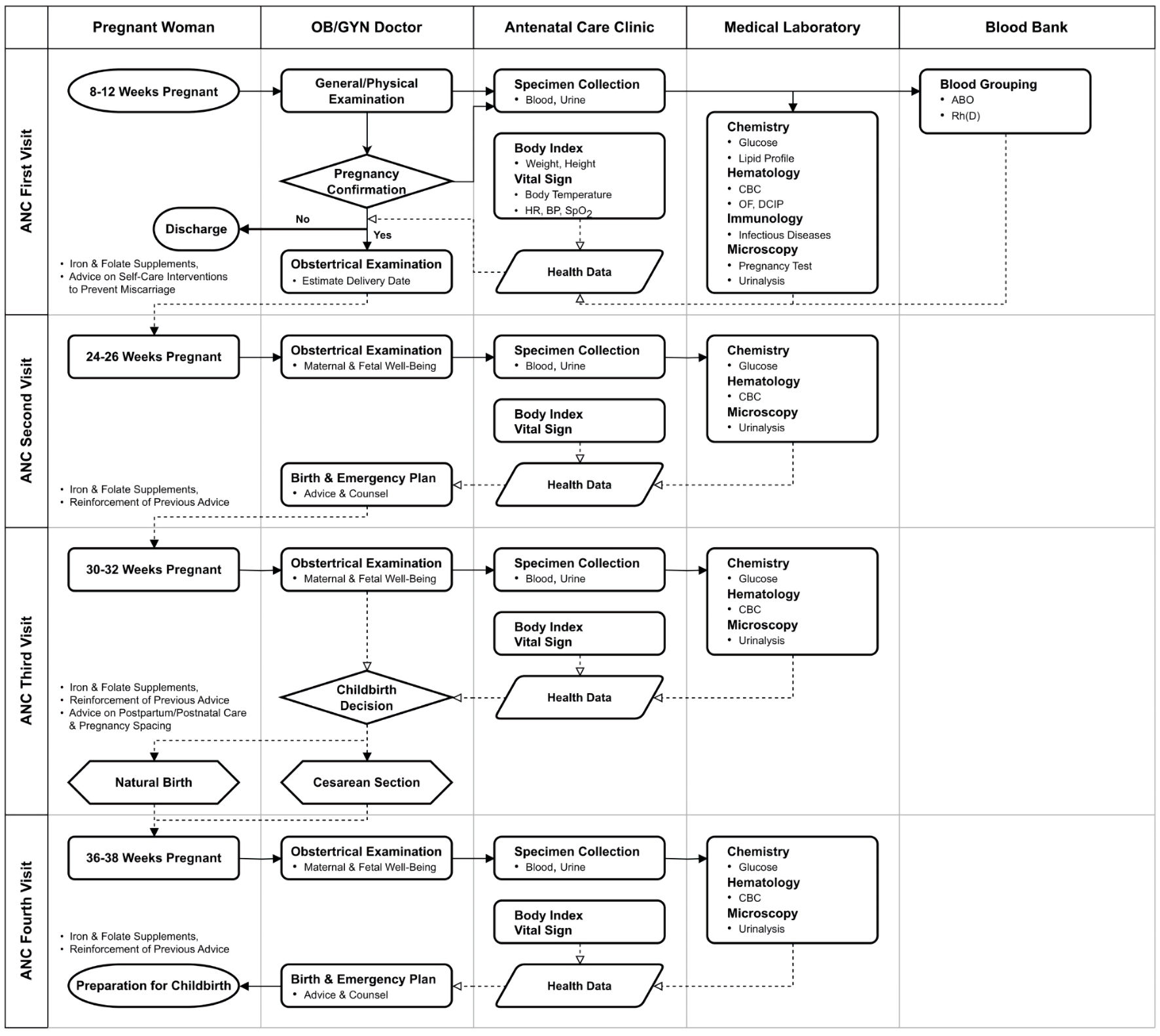 Click for large image | Figure 3. Flowchart depicting the pregnancy care pathway for women at different stages in the Obstetrics and Gynecology Department of the hospital, encompassing laboratory tests and decision-making regarding delivery. HR: heart rate; BP: blood pressure; SpO2: oxygen saturation; CBC: complete blood count; OF: osmotic fragility; DCIP: dichlorophenol indophenol precipitation. |
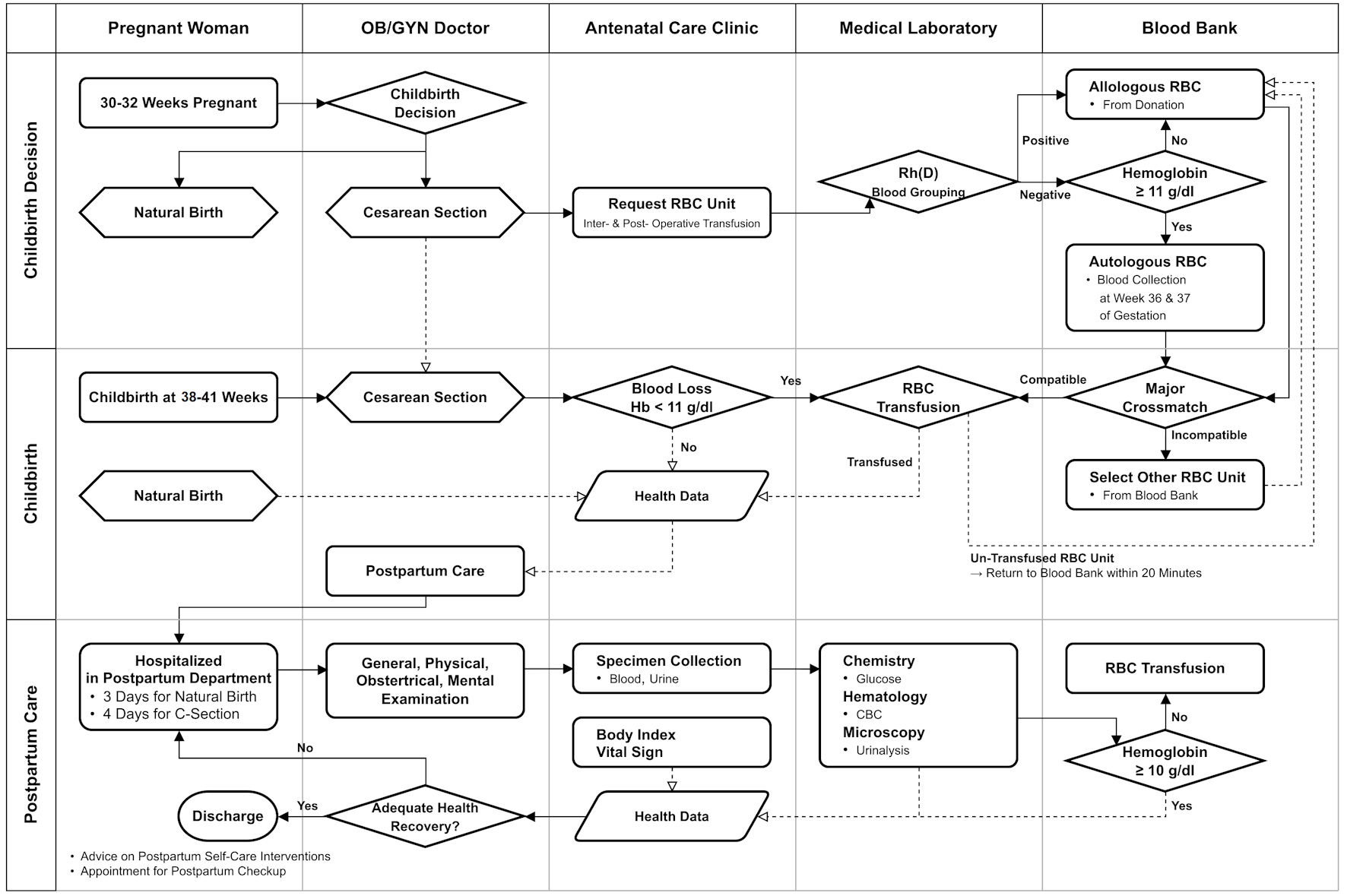 Click for large image | Figure 4. Flowchart illustrating childbirth decisions and preparations for autologous blood donation in pregnancies with rare blood groups (Rh-negative). RBC: red blood cell. |
The disadvantage of autologous blood donation is that if the prepared blood is not used by the patient, it must be discarded and cannot be given to other patients and can rarely be used for other patients because most autologous donors do not meet the stringent health requirements for allogeneic blood donation [32]. However, many pregnant women who have never donated blood before find the experience of donating blood for themselves memorable and become regular blood donors in the future. Regarding the cost-benefit, the hospital spent almost $600 ($25 per unit of blood and $120 per year), which is relatively low. Considering the immeasurable value of life, the preparation of two bags of blood before surgery is justified, even though Rh-negative blood is rare among Thais. In the future, satisfaction surveys will be conducted for individuals considering autologous blood donation, and systems for more efficient consultation networks will be developed.
Currently, the Health Committee for Mothers and Children in Phang Nga Province has designated Takuapa Hospital as a model for improving the health of pregnant women. This includes encouraging autologous blood donation for those scheduled to undergo C-sections at other hospitals within the province.
Conclusions
We successfully perform autologous blood collection from pregnant women, maintaining normal Hct levels until delivery. Preparing two bags of autologous blood for patients with special blood types is safe. Hb levels decreased by an average of 0.95 g/dL over 3 weeks, and Hct levels by 2.0%, both remaining within normal ranges. The average Hb was 12.1 g/dL, and Hct was 35.6%. All infants weighed over 2,600 g, indicating good health for both mother and child. Both mother and baby were safe with no adverse outcomes. The revived procedure of autologous blood preparation will be used as a standard protocol in the hospital, and the knowledge will be transferred to the hospital network.
Acknowledgments
We would like to thank Ms. Jurairat Rattanalertnavee, Head of the Medical Technology Department, who promoted the research, and Mr. Supoj Saithong, Medical Technologist at Sunpasitthiprasong Hospital, who assisted with research statistics, along with personnel from the Medical Technology Department, the Antenatal Care Unit, and the Obstetrics and Gynecology Department, who helped record and collect data. Their cooperation was crucial in successfully completing this research according to the set objectives.
Financial Disclosure
There was no specific source to be mentioned.
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
All subjects provided written informed consent.
Author Contributions
SW conceived the presented idea. All authors planned the experiments. SW and PS conducted the experiments. All authors contributed to the interpretation of the results. NK assisted with the statistical analysis. SW and NK led the manuscript writing. NC supervised and carefully edited the manuscript.
Data Availability
The authors declare that data supporting the findings of this study is available within the article.
| References | ▴Top |
- Angolile CM, Max BL, Mushemba J, Mashauri HL. Global increased cesarean section rates and public health implications: A call to action. Health Sci Rep. 2023;6(5):e1274.
doi pubmed pmc - Rahman M, Khan N, Rahman A, Alam M, Khan A. Long-term effects of caesarean delivery on health and behavioural outcomes of the mother and child in Bangladesh. J Health Popul Nutr. 2022;41(1):45.
doi pubmed pmc - Keag OE, Norman JE, Stock SJ. Long-term risks and benefits associated with cesarean delivery for mother, baby, and subsequent pregnancies: Systematic review and meta-analysis. PLoS Med. 2018;15(1):e1002494.
doi pubmed pmc - Magann EF, Evans S, Hutchinson M, Collins R, Lanneau G, Morrison JC. Postpartum hemorrhage after cesarean delivery: an analysis of risk factors. South Med J. 2005;98(7):681-685.
doi pubmed - Di Ciaccio P, Cutts B, Alahakoon TI, Dennington PM, Soo LA, Curnow J. Clinical consequences of the extremely rare anti-PP1Pk isoantibodies in pregnancy: a case series and review of the literature. Vox Sang. 2021;116(5):591-600.
doi pubmed - Joshi SR, Vasantha K. A profile of rare bloods in India and its impact in blood transfusion service. Asian J Transfus Sci. 2012;6(1):42-43.
doi pubmed pmc - da Silva Rodrigues de Araujo C, Machado BA, Reche CD, Maroni L, Garlet LC, Meinhardt Pinheiro Dos Santos M, Beber M, et al. Identification of rare blood types in southern Brazil: impact on transfusion support. Immunohematology. 2020;36(4):152-156.
pubmed - Transfusion alert: use of autologous blood. National heart, lung, and blood institute expert panel on the use of autologous blood. Transfusion. 1995;35(8):703-711.
doi pubmed - Goodnough LT, Brecher ME, Kanter MH, AuBuchon JP. Transfusion medicine. First of two parts—blood transfusion. N Engl J Med. 1999;340(6):438-447.
doi pubmed - Vassallo R, Goldman M, Germain M, Lozano M, BEST Collaborative. Preoperative autologous blood donation: waning indications in an era of improved blood safety. Transfus Med Rev. 2015;29(4):268-275.
doi pubmed - Sam AM, Gupta D, Radhakrishnan A, Sethuraman M, Dash PK, Pitchai S, Kesavapisharady K. Autologous versus allogeneic blood transfusion: A comparative study of the peri-operative outcomes in a tertiary care hospital in South India amidst the COVID-19 pandemic. Transfus Apher Sci. 2023;62(5):103753.
doi pubmed pmc - Jano A, Sula H, Domi R. Considerations on autologous blood transfusion. J Anesth Crit Care Open Access. 2016;6(2):00225.
doi - Adias TC, Jeremiah Z, Uko E, Osaro E. Autologous blood transfusion - a review. S Afr J Surg. 2006;44(3):114-116, 118.
pubmed - Nnodu OE, Odunukwe N, Odunubi O, Ekanem E, Njoku OS. Cost effectiveness of autologous blood transfusion—a developing country hospital's perspective. West Afr J Med. 2003;22(1):10-12.
doi pubmed - ACOG practice bulletin No 156: obesity in pregnancy. Obstet Gynecol. 2015;126(6):e112-e126.
doi pubmed - Abbassi-Ghanavati M, Greer LG, Cunningham FG. Pregnancy and laboratory studies: a reference table for clinicians. Obstet Gynecol. 2009;114(6):1326-1331.
doi pubmed - Ahmed SG. A strategic approach to the problems of providing rhesus D-negative blood transfusion in geographic areas with low RhD negativity: a Nigerian perspective. Transfus Med Rev. 2010;24(2):140-146.
doi pubmed - Maryam DU, Mukhtar IG, Yusuf AA, Salisu AI. High prevalence of serological weak D phenotype and preponderance of weak D type 4.0.1. genetic variant in a Nigerian population: implications for transfusion practice in a resource-limited setting. Hematol Transfus Cell Ther. 2022;44(3):386-391.
doi pubmed pmc - Pahuja S, Pujani M, Gupta SK, Chandra J, Jain M. Alloimmunization and red cell autoimmunization in multitransfused thalassemics of Indian origin. Hematology. 2010;15(3):174-177.
doi pubmed - Simtong P, Phothi R, Puapairoj C, Leelayuwat C, Romphruk AV. RHD 1227 A and hybrid Rhesus box analysis in Thai RhD+ and RhD- blood donors: Prevalence, RHD zygosity, and molecular screening. Transfus Apher Sci. 2022;61(6):103496.
doi pubmed - Zhou J. A review of the application of autologous blood transfusion. Braz J Med Biol Res. 2016;49(9):e5493.
doi pubmed pmc - Watanabe N, Suzuki T, Ogawa K, Kubo T, Sago H. Five-year study assessing the feasibility and safety of autologous blood transfusion in pregnant Japanese women. J Obstet Gynaecol Res. 2011;37(12):1773-1777.
doi pubmed - Cataldi S, Bruder N, Dufour H, Lefevre P, Grisoli F, Francois G. Intraoperative autologous blood transfusion in intracranial surgery. Neurosurgery. 1997;40(4):765-771; discussion 771-762.
doi pubmed - Yamamoto Y, Yamashita T, Tsuno NH, Nagamatsu T, Okochi N, Hyodo H, Ikeda T, et al. Safety and efficacy of preoperative autologous blood donation for high-risk pregnant women: experience of a large university hospital in Japan. J Obstet Gynaecol Res. 2014;40(5):1308-1316.
doi pubmed - Gari A, Hussein K, Daghestani M, Aljuhani S, Bukhari M, Alqahtani A, Almarwani M. Estimating blood loss during cesarean delivery: A comparison of methods. J Taibah Univ Med Sci. 2022;17(5):732-736.
doi pubmed pmc - Khan FA, Khan M, Ali A, Chohan U. Estimation of blood loss during Caesarean section: an audit. J Pak Med Assoc. 2006;56(12):572-575.
pubmed - Ozumba BC, Ezegwui HU. Blood transfusion and caesarean section in a developing country. J Obstet Gynaecol. 2006;26(8):746-748.
doi pubmed - Akinlusi FM, Rabiu KA, Durojaiye IA, Adewunmi AA, Ottun TA, Oshodi YA. Caesarean delivery-related blood transfusion: correlates in a tertiary hospital in Southwest Nigeria. BMC Pregnancy Childbirth. 2018;18(1):24.
doi pubmed pmc - Bothwell TH. Iron requirements in pregnancy and strategies to meet them. Am J Clin Nutr. 2000;72(1 Suppl):257S-264S.
doi pubmed - Ferrari FA, Garzon S, Raffaelli R, Cromi A, Casarin J, Ghezzi F, Uccella S, et al. Tranexamic acid for the prevention and the treatment of primary postpartum haemorrhage: a systematic review. J Obstet Gynaecol. 2022;42(5):734-746.
doi pubmed - Yamada T, Mori H, Ueki M. Autologous blood transfusion in patients with placenta previa. Acta Obstet Gynecol Scand. 2005;84(3):255-259.
doi pubmed - Vanderlinde ES, Heal JM, Blumberg N. Autologous transfusion. BMJ. 2002;324(7340):772-775.
doi pubmed pmc
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.