| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://jocmr.elmerjournals.com |
Original Article
Volume 000, Number 000, November 2024, pages 000-000
Construction of a Clinical Prediction Model for Complications After Femoral Head Replacement Surgery
Ke Wei Lia, Shuai Ronga, Hao Lia, b
aPediatric Orthopedics, The Third Hospital of Shijiazhuang, Shijiazhuang City, Hebei Province, China
bCorresponding Author: Hao Li, Pediatric Orthopedics, The Third Hospital of Shijiazhuang, Shijiazhuang City, Hebei Province, China
Manuscript submitted August 26, 2024, accepted October 30, 2024, published online November 11, 2024
Short title: Construction of a Clinical Prediction Model
doi: https://doi.org/10.14740/jocmr6047
| Abstract | ▴Top |
Background: While femoral head replacement is widely used with remarkable efficacy, the complexity and diversity of postoperative complications pose a serious prognostic challenge. There is an urgent need to develop a clinical prediction model that can integrate multiple factors and accurately predict the risk of postoperative complications to guide clinical practice and optimize patient management strategies. This study is dedicated to constructing a postoperative complication prediction model based on statistics and machine learning techniques, in order to provide patients with a safer and more effective treatment experience.
Methods: A total of 186 patients who underwent femoral head replacement in the Orthopedic Department of our hospital were collected in this study. Forty-two of the patients had at least one postoperative complication, and 144 had no complications. The preoperative and postoperative data of patients were collected separately and medical history was collected to study the correlation factors affecting the occurrence of postoperative complications in patients and to establish a prediction model.
Results: Possibly relevant factors were included in a one-way logistic regression, which included the patient’s gender, age, body mass index, preoperative diagnosis of the mode of injury, osteoporosis or lack thereof, as well as medical history, surgical-related information, and laboratory indices. After analyzing the results, it was concluded that operation time, alanine transaminase (ALT), aspartate aminotransferase (AST), white blood cell count, serum albumin, and osteoporosis, were the risk factors affecting the development of complications after femoral head replacement in patients (P < 0.2). The data obtained were further included in a multifactorial regression, and the results showed that operation time, AST, white blood cell count, serum albumin, and osteoporosis were independent risk factors for complications after the patients underwent femoral head replacement (P < 0.05).
Conclusion: Based on the results of this study, five factors, including duration of surgery, AST, white blood cell count, serum albumin, and osteoporosis, were identified as independent risk factors for complications after patients underwent femoral head replacement. In addition, the prediction model developed in this study has a high scientific and clinical application value, providing clinicians and patients with an important tool for assessing the risk of complications after affected femoral head replacement.
Keywords: Femoral head replacement surgery; Complications; Logistic regression; Risk factor; Line graph
| Introduction | ▴Top |
Femoral head replacement has been widely used worldwide as an important treatment for femoral head necrosis and severe hip disease [1-3]. With the advancement of medical technology and improvement of surgical methods, the prognosis of patients has significantly improved, but the incidence of postoperative complications is still high, which seriously affects the quality of life of patients and the recovery process [4, 5]. Possible postoperative complications of femoral head replacement include, but are not limited to, postoperative infection, loosening of the prosthesis, dislocation, deep vein thrombosis, pulmonary embolism, and transfusion reactions, which not only increase the financial burden of the patient, but may also threaten his or her life [6, 7]. Currently, although some studies have focused on complications after femoral head replacement [8-10], clinical prediction models for these complications are still lacking, especially comprehensive prediction models that can take into account multiple factors, such as individual patient differences, preoperative conditions, surgical procedures, and postoperative recovery. Moreover, most of the current predictive models for complications after femoral head replacement only address single complications such as dislocation, deep venous thrombosis of lower limbs, occult postoperative blood loss, loss of walking independence, and blood transfusion [11-15]. There is no systematic predictive model for common complications after femoral head surgery. Therefore, constructing an accurate and effective clinical prediction model for postoperative complications is of great significance in guiding clinical decision-making and optimizing perioperative management. Clinical predictive modeling, as a tool based on statistical and machine learning techniques, is able to estimate the probability of having a certain disease or the probability of a certain outcome occurring in the future using multifactorial models to provide a scientific basis for clinical decision-making [16, 17]. Such models include diagnostic models, which are used for early diagnosis of diseases, and prognostic models, which are used to predict disease progression and complications [16]. In the field of femoral head replacement, the construction of a clinical prediction model for postoperative complications helps physicians to risk stratify patients before surgery and formulate personalized treatment strategies, thus improving the success rate of surgery and reducing the complication rate. In this study, we retrospectively analyzed clinical data from a large number of patients undergoing femoral head replacement to screen for independent risk factors for postoperative complications and the corresponding nomogram prediction model is constructed.
| Materials and Methods | ▴Top |
Research objects
This study adopts a retrospective case-control study, which was used to collect clinical data related to patients who underwent femoral head replacement in the Department of Orthopedics of our hospital during the period from March 2021 to June 2024. A total of 186 patients were enrolled in the group, including 98 males and 88 females. The study was approved by the Ethics Committee of our hospital. The Number is W-072-13. All methods were performed in accordance with the relevant guidelines and regulations.
Inclusion criteria were: 1) patients diagnosed with femoral neck fracture or caput femoris necrosis; 2) patients who underwent femoral head replacement surgery; 3) patients diagnosed with unilateral femoral neck fracture or caput femoris necrosis; 4) no combination of fractures elsewhere; and 5) complete documentation of patient perioperative treatment data and medical history.
Exclusion criteria were: 1) a history of old fractures, multiple fractures, and secondary fractures; 2) the clinical data are missing; 3) combined with severe heart, liver, lung, and kidney diseases; 4) history of malignant tumor; 5) individuals who are pregnant or lactating; 6) severe mental or psychological disorders; and 7) patients who died due to surgery.
Research methods
A total of 186 patients were collected in this study, of which 42 patients had at least one postoperative complication and 144 patients had no complications. Pre- and postoperative data were collected from the patients separately and medical histories were collected to study the correlates affecting the occurrence of postoperative complications in the patients.
Collect indicators
In this study, gender, age, body mass index (BMI), occurrence of complications or not, preoperative diagnosis of injury modality, osteoporosis or not of the patient, and the patient’s medical history were collected, as well as information related to the patient’s surgery and the patient’s laboratory parameters. The operation information includes the operation time, operation mode and whether bone cement is used during the operation. Laboratory tests include alanine transaminase (ALT), aspartate aminotransferase (AST), white blood cells, platelets, and albumin.
Statistical methods
The data were processed and statistically analyzed in this study using SPSS 25.0 and R language (R 4.1.2). Quantitative information that conformed to normal distribution was expressed as mean ± standard deviation, and differences between groups were analyzed using the independent samples t-test. Comparisons between groups that do not obey a normal distribution are made using nonparametric tests. Data for qualitative information were expressed as number of cases and percentages, and the Chi-square test was used to determine if there were differences between groups. Firstly, based on the analysis of the occurrence of postoperative complications in patients and various clinical indicators and other factors, and then based on the one-way logistic regression analysis of the collected data, to determine the potential risk factors for the occurrence of postoperative complications in patients with femoral head replacement. In the univariate analysis, the exposure factors with P ≤ 0.2 were selected and included in the multivariate analysis to derive the independent risk factors associated with the development of complications after femoral head replacement. P < 0.05 was considered a statistically significant difference.
Complications involved in this study and their definitions
Incision infection, dislocation, nerve injury, and deep venous thrombosis of lower limbs are common complications after surgery. If a lower extremity venous thrombus is dislodged, the embolus may follow the circulation and obstruct the pulmonary vessels causing pulmonary embolism, which may be fatal. Fracture around prosthesis seriously affects the patient’s postoperative recovery and surgical satisfaction.
Incision infection
Incision infection includes superficial incision infections and deep incision infections. Blood routine and C-reactive protein examination were routinely performed before operation. Postoperatively, the presence of incision infection is determined by observing the patient’s subcutaneous and deep tissues of the incision for redness, swelling, and fluid accumulation.
Deep venous thrombosis of lower limbs
By comparing the preoperative and postoperative deep vein ultrasound of the lower extremities of the affected patients, if no deep vein thrombosis of the lower extremities was detected in the preoperative examination but a thrombus was found in the lower extremities in the postoperative review, it was indicated that deep vein thrombosis of the lower extremities existed in the postoperative period.
Dislocation
Dislocation refers to prolapse or subluxation of the femoral head out of the acetabulum from any cause within 30 days after surgery, resulting in loss of normal anatomy between the femur and the pelvis.
Pulmonary embolism
Postoperative pulmonary embolism was considered to have occurred if the patient developed postoperative symptoms such as chest pain and dyspnea, which were clearly diagnosed by computed tomography angiography (CTA).
Fracture around prosthesis
Fracture around prosthesis refers to disruption of the integrity or continuity of the bone in the position of the prosthesis for any reason within 30 days after surgery.
Nerve injury
The sciatic nerve, femoral nerve, obturator nerve, and peroneal nerve can all be damaged, and patients with postoperative sensory abnormalities such as numbness of lower limbs or foot drop are defined as nerve injury.
Machine learning techniques
Machine learning technology is an important branch in the field of artificial intelligence science. In recent years, machine learning technology has been gradually used in the medical field for its efficiency and convenience, mainly including disease diagnosis and medical data analysis [18]. It has unique advantages that traditional statistics do not have. In this study, we predicted the occurrence of postoperative complications after femoral head replacement based on machine learning technology, found the related risk factors, and established the related prediction model, with a view to providing a reference basis for clinical diagnosis and treatment.
| Results | ▴Top |
Table 1 shows the assignment of related indicators in this study.
 Click to view | Table 1. Assignment of Related Indicators |
Baseline characteristics
Patients were grouped based on whether they had complications after undergoing femoral head replacement, with 144 in the non-complication group and 42 in the complication group. Gender, age, and BMI of patients in both groups were included in the statistical study. There was no significant difference in baseline characteristics (P > 0.05) (Table 2).
 Click to view | Table 2. Baseline Characteristics |
One-way logistic regression analysis
Possibly relevant factors were included in a one-way logistic regression, which included the patient’s gender, age, BMI, preoperative diagnosis of the mode of injury, osteoporosis or lack thereof, as well as medical history, surgical-related information, and laboratory indices. After analyzing the results, it was concluded that operation time (odds ratio (OR) = 1.12, P < 0.001), ALT (OR = 1.04, P = 0.038), AST (OR = 1.12, P < 0.001), white blood cell count (OR = 2.90, P < 0.001), serum albumin (OR = 0.84, P < 0.001), and osteoporosis (OR = 4.54, P < 0.001), were the risk factors affecting the development of complications after femoral head replacement in patients (P < 0.2) (Table 3).
 Click to view | Table 3. One-Way Logistic Regression Analysis of Complications After Femoral Head Replacement Surgery |
Multifactorial regression
The six risk factors of operation time, ALT, AST, white blood cell count, serum albumin, and osteoporosis derived from the one-way logistic regression analysis were further included in the multifactorial regression. The results showed that operation time (OR = 1.10, P = 0.001), AST (OR = 1.10, P = 0.002), white blood cell count (OR = 3.04, P < 0.001), serum albumin (OR = 0.83, P = 0.002), and osteoporosis (OR = 4.39, P = 0.004) were independent risk factors for complications after the patients underwent femoral head replacement (P < 0.05) (Table 4).
 Click to view | Table 4. Multifactorial Regression of Complications After Femoral Head Replacement |
Drawing of nomogram
A nomogram of the risk of complications after femoral head replacement was constructed based on five independent predictors tested by multivariate logistic regression analysis (Fig. 1). A Nomo score was assigned to each independent risk factor, and the total score was derived by summation based on the clinical characteristics of that patient, positioned on the total points axis. The value on the risk axis corresponding vertically downward is the probability of a complication after femoral head replacement in that patient. The score for each independent predictor corresponds to the upper limit of the score for each independent predictor, and the total score for each subject is the sum of the scores for each independent predictor. The risk of complications after femoral head replacement is determined by the total score on the axis of risk of complications after femoral head replacement. For example, if there is a patient with osteoporosis, the Nomo score assigned to osteoporosis is 20; if the operation time for the patient is 80 min, the Nomo score assigned to operation time is 20; if the white blood cell count is 9.5, the Nomo score is 70; if the AST is 20, the Nomo score is 20; if the serum albumin is 35, the Nomo score assigned to serum albumin is 50. After summation based on the clinical characteristics of the patient, we can calculate the total score is 185. Subsequently, the value on the risk axis corresponding vertically downward is over 0.9. The probability of a complication after femoral head replacement in the patient is over 0.9. Therefore, we can intervene with patients before complications occur and develop a reasonable treatment plan, such as enhancing dressing changes at the surgical site, moderate mobility of the lower extremities, and regular review of lower extremity deep vein ultrasound. Then the model is verified internally. Bootstrap method in R software is used to repeat sampling for 1,000 times to verify the nomogram. The calibration curve is close to the ideal curve, which shows that the nomogram predicts the incidence of complications after femoral head replacement with a high degree of coincidence with the actual incidence, showing good predictive performance, as shown in Figure 2. The receiver operating characteristic (ROC) curve of the nomogram has an area under the curve (AUC) of 0.90 (95% confidence interval (CI) = 0.84 - 0.96), as shown in Figure 3. It shows that the nomogram has a good degree of discrimination for the high-risk population with complications after femoral head replacement. The decision curve analysis (DCA) of the nomogram shows that in this nomogram, when the threshold probability of individuals is greater than 0.05, the model provides more net benefits than the strategy of “everyone intervenes” or “no one intervenes”. This conclusion shows that the nomogram model has good clinical application value in predicting the complications after femoral head replacement, as shown in Figure 4.
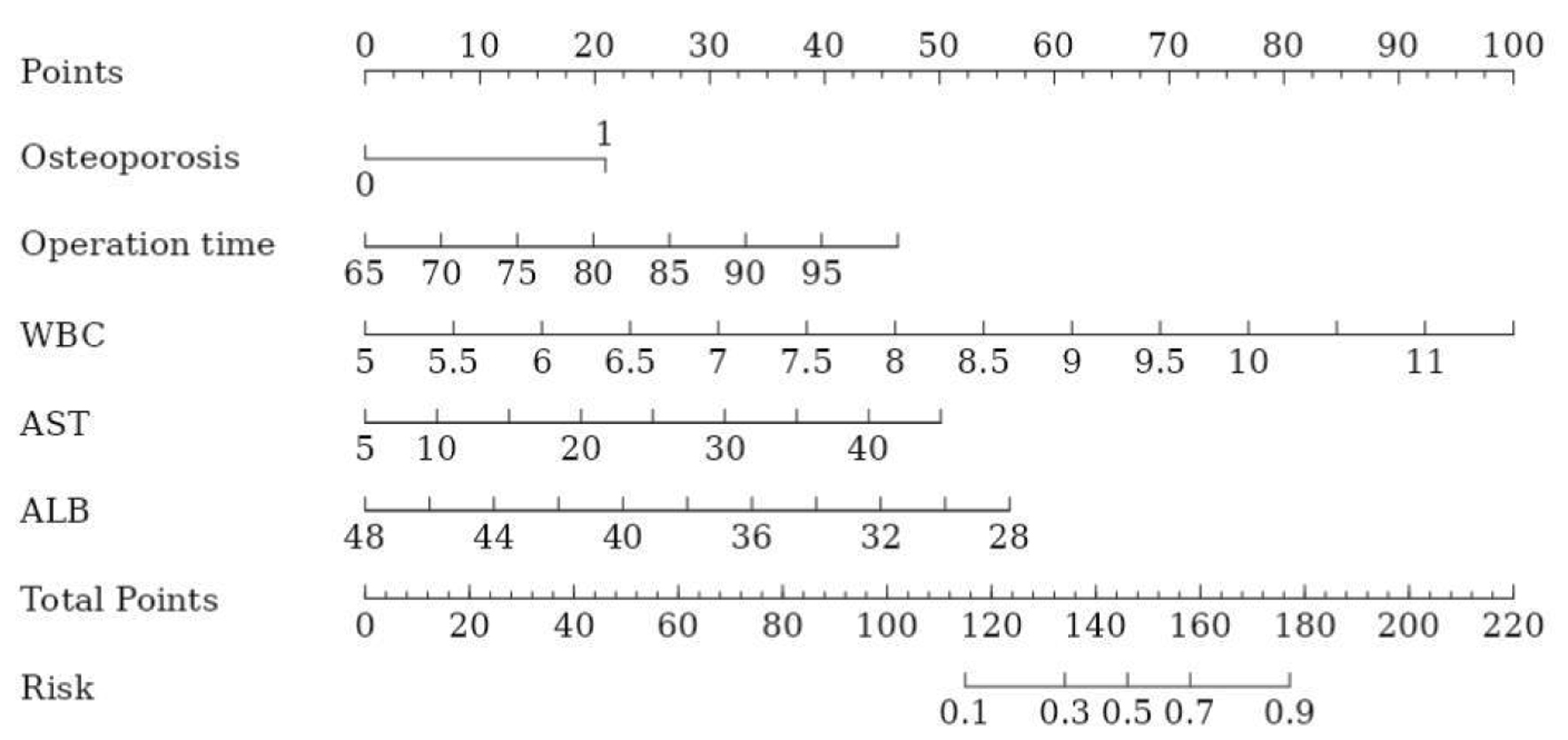 Click for large image | Figure 1. Nomogram prediction of the risk of complications after femoral head replacement. ALB: serum albumin; AST: aspartate aminotransferase; WBC: white blood cell. |
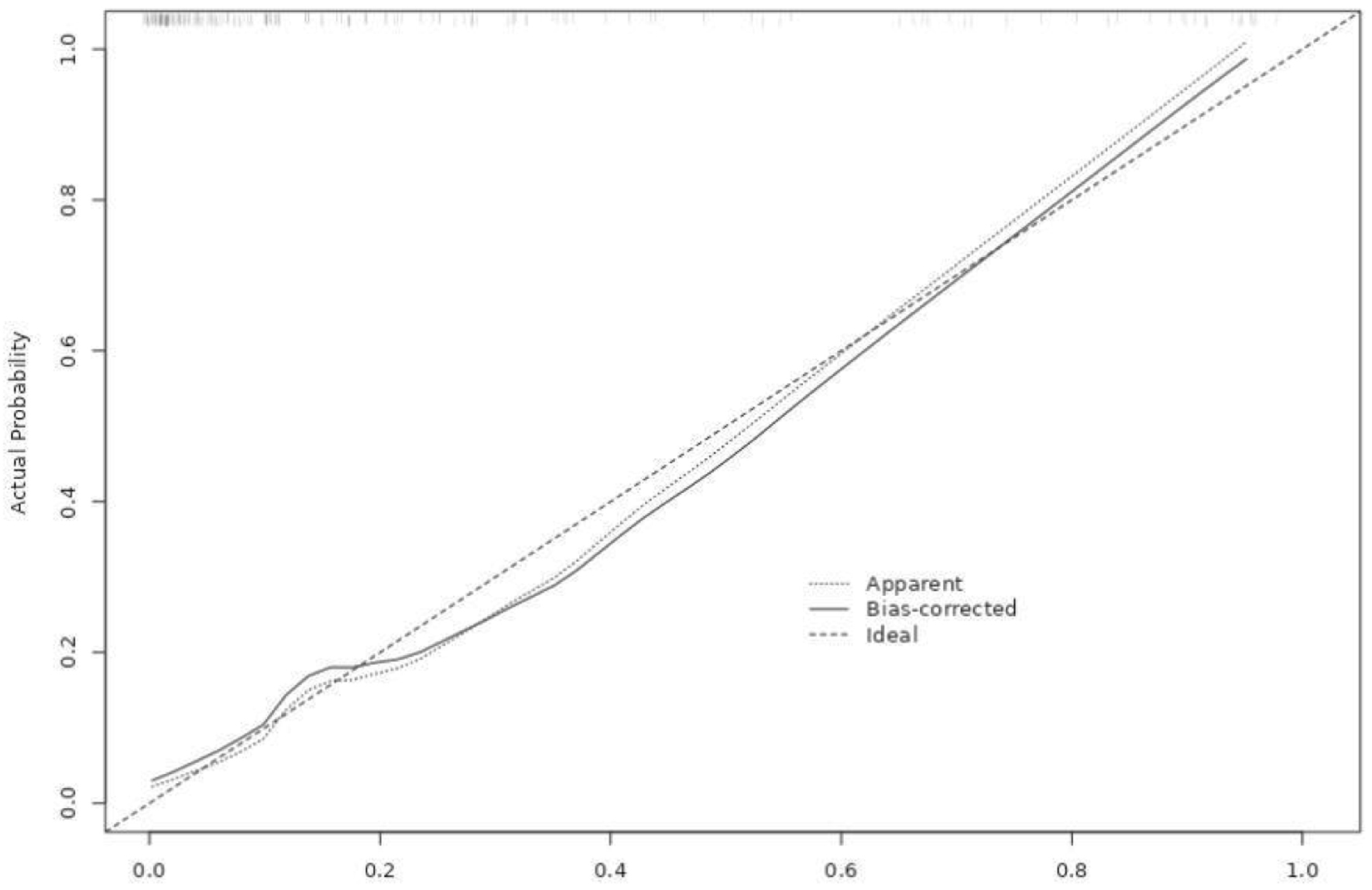 Click for large image | Figure 2. Internal verification of nomogram-calibration curve. |
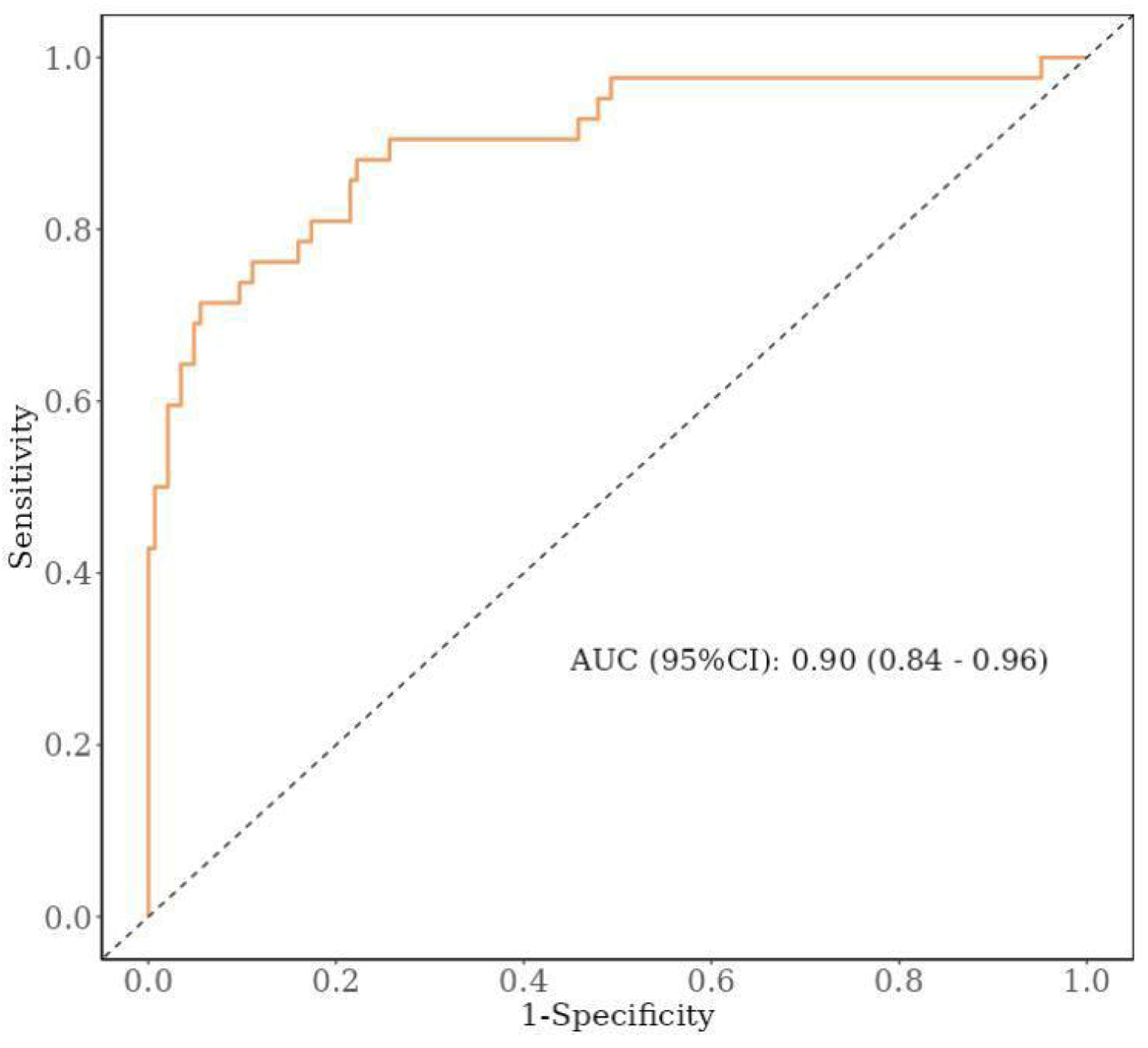 Click for large image | Figure 3. ROC curve. ROC: receiver operating characteristic; AUC: area under the curve; CI: confidence interval. |
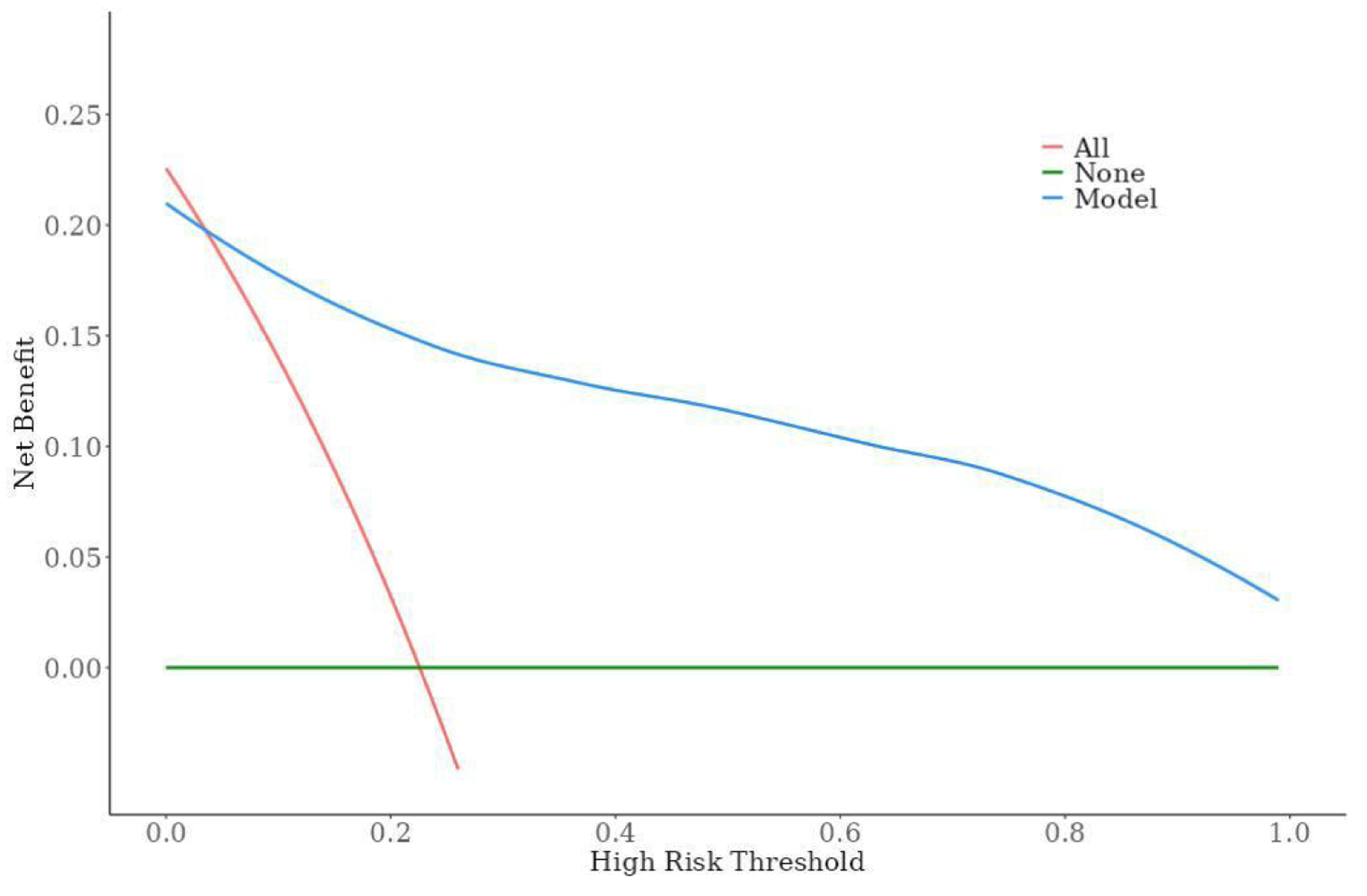 Click for large image | Figure 4. Decision curve in the model. |
| Discussion | ▴Top |
Significance of model construction
In this study, five independent predictors were screened from numerous potential factors by multivariate logistic regression analysis, and the results showed that operation time, AST, white blood cell count, serum albumin, and osteoporosis were independent risk factors for complications after the patients underwent femoral head replacement, and a risk prediction model for postoperative complications after femoral head replacement was constructed. This methodology is consistent with many previous studies of clinical disease prediction models [19-21]. For example, in Luo et al’s study, a similar multivariate regression analysis approach was used to emphasize the rigor and scientific validity of statistical models [20]. Similarly, Bayramoglu et al predicted whether patellofemoral osteoarthritis occurs or not based on deep learning of lateral knee radiographs, demographics and symptom assessment and is widely used [22]. However, this study is unique in that it focuses on the specific area of femoral head replacement and fills a gap in the field with regard to the prediction of postoperative complications.
Accuracy and performance evaluation of prediction model
The results of the internal validation of this model show that the calibration curve of the model is highly close to the ideal curve, indicating good agreement between the predicted values and the actual observed values, which is an important indicator for assessing the accuracy of the prediction model. Compared to the study by Cabrera et al in the prediction of problems related to orthopedic surgery [23], the AUC value of the present model (0.90) is at a high level, showing greater discriminatory power and higher prediction accuracy. The performance of high sensitivity and high specificity further validates the reliability of the model in clinical practice, which can effectively identify high-risk patients and provide strong support for clinical decision-making.
Discussion on independent risk prediction factors
This model confirms that operation time, AST, white blood cell count, serum albumin, and osteoporosis are all strongly associated with the development of postoperative complications after femoral head replacement. The intrinsic reason for this is to consider that prolonged surgery may lead to increased tissue damage, increased risk of infection, as well as compromised postoperative recovery, which in turn increases the incidence of postoperative complications. Shi et al conducted a retrospective study and found that the complications of artificial femoral head replacement is less than internal proximal femur locking plate fixation, and the operation time is less, too. This is consistent with our findings [24]. Also in femoral head replacement surgery, although the liver is not the direct surgical site, surgical stress, medication use, and potential complications (e.g., infection, bleeding) may affect liver function and result in elevated AST levels. High AST levels may suggest impaired liver function, which in turn affects systemic metabolism and detoxification and increases the risk of postoperative complications. Therefore, AST can be used as a reference index for assessing the systemic status of patients before and after surgery and for predicting the occurrence of postoperative complications. This is consistent with the findings of McLellan et al, who found that all patients in the abnormal aspartate aminotransferase-to-platelet ratio index (APRI) group had increased odds of complications after total hip arthroplasty compared to the normal APRI (P < 0.05) [25]. Meanwhile, a study by Matcovici et al showed that high APRI is a high-risk factor for failure of Kasai portoenterostomy [26]. At the same time, serum albumin is an important protein for maintaining plasma osmotic pressure and transporting nutrients. Low albumin levels may indicate that the patient is malnourished or has impaired liver function, which in turn affects the body’s immunity and ability to recover [27]. This is consistent with the study by Bohl et al, who showed that in elderly patients undergoing hip fracture surgery, patients with hypoproteinemia had higher rates of death, sepsis, and unplanned intubation compared to patients with normal albumin concentrations (P < 0.001) [28]. Finally, osteoporosis is one of the common comorbidities in patients undergoing femoral head replacement surgery, and the two interact. Osteoporosis patients have poorer bone quality, reduced bone density, and destruction of the trabecular structure of the bone, which may lead to postoperative complications such as poor fixation, loosening, or even sinking of the prosthesis. This is consistent with the study by Harris et al, who showed that the 5-year rate of all-cause revision surgery was higher for patients who had osteoporosis (hazard ratio (HR) 1.1, 95% CI: 1.0 - 1.2) [29].
Significance of nomogram model in risk assessment of postoperative complications
Nomogram constructed in this study provides an intuitive and convenient risk assessment tool for clinicians and patients. Through simple calculation, the probability of postoperative complications can be obtained, which is helpful for doctors to make personalized surgery and rehabilitation plans. In contrast to the study by Cichos et al on postoperative management strategies for femoral head replacement [30], the present model not only provides a risk assessment, but also emphasizes the importance of early intervention, which complements the existing management strategies and works together to promote the quality of patient recovery.
Limitations
Although some achievements have been made in this study, we still need to recognize the limitations of the model. First, as mentioned earlier, the sample size was relatively limited and from a single center, and future studies should consider expanding the sample size and multicenter collaboration to verify the general applicability of the model. In addition, due to the single center and small sample size, we were limited in the amount of data we could collect, and therefore there were some flaws in the design of the study. There is a clear clinical grading of the severity of comorbidities such as diabetes, hypertension, and osteoporosis. The impact of different clinical grades of diabetes mellitus or hypertension on postoperative complications after femoral head replacement in patients varies widely. In future studies, we will further improve the multicenter large sample size study, and then be able to do continuous variables that respond to the severity of complications, and then go on to better reflect the clinical significance. Furthermore, postoperative pain of varying degrees occurs at the surgical site and we give nonsteroidal anti-inflammatory drugs (NSAIDs) for symptomatic treatment. This drug is metabolized by the liver and may cause varying degrees of liver damage, which in turn may lead to elevated transaminases (such as AST). Therefore, we recognize that NSAIDs are confounding factors of our researches. Besides, in the data we collected, 70% was used for cross-validation. Then we can build a prediction model based on these data. Subsequently, we use the remaining 30% for internal validation. Future studies would aim to validate this model in a larger, multicenter cohort to assess its generalizability. Second, as medical technology and clinical practice continue to evolve, new risk factors may emerge and the model needs to be updated periodically to incorporate new variables. In addition, advanced technologies such as artificial intelligence and machine learning can be explored for application in model construction and optimization to improve prediction accuracy and generalization ability.
Conclusions
Based on the results of this study, five factors, including operation time, AST, white blood cell count, serum albumin, and osteoporosis were identified as independent risk factors for complications after patients underwent femoral head replacement. In addition, the prediction model developed in this study has a high scientific and clinical application value, providing clinicians and patients with an important tool for assessing the risk of complications after affected femoral head replacement. Future studies should aim to validate this model in a larger, multicenter cohort to assess its generalizability.
Acknowledgments
None to declare.
Financial Disclosure
Analysis of the Therapeutic Effect of Miniature Ilizarov External Fixation Technique in the Treatment of Soft Tissue-Type Syndactyly in Children. Number: 20191425. Key Scientific Research Plan Project of Medical Science Research in Hebei Province.
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
Informed consent was obtained from all subjects and/or their legal guardian(s).
Author Contributions
Hao Li participated in case collection; Ke Wei Li wrote the manuscript and raised idea; Shuai Rong revised the manuscript and raised critical editing. All authors have read and approved the manuscript.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
ALB: serum albumin; ALT: alanine transaminase; AST: aspartate aminotransferase; AUC: area under the curve; BMI: body mass index; CI: confidence interval; CTA: computed tomography angiography; DCA: decision curve analysis; OR: odds ratio; P: P-values; ROC: receiver operating characteristic; WBC: white blood cell
| References | ▴Top |
- Hines JT, Jo WL, Cui Q, Mont MA, Koo KH, Cheng EY, Goodman SB, et al. Osteonecrosis of the femoral head: an updated review of ARCO on pathogenesis, staging and treatment. J Korean Med Sci. 2021;36(24):e177.
doi pubmed pmc - Saueressig T, Owen PJ, Zebisch J, Herbst M, Belavy DL. Evaluation of exercise interventions and outcomes after hip arthroplasty: a systematic review and meta-analysis. JAMA Netw Open. 2021;4(2):e210254.
doi pubmed pmc - Stibolt RD, Jr., Patel HA, Huntley SR, Lehtonen EJ, Shah AB, Naranje SM. Total hip arthroplasty for posttraumatic osteoarthritis following acetabular fracture: a systematic review of characteristics, outcomes, and complications. Chin J Traumatol. 2018;21(3):176-181.
doi pubmed pmc - Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91(1):128-133.
doi pubmed - Yan L, Ge L, Dong S, Saluja K, Li D, Reddy KS, Wang Q, et al. Evaluation of comparative efficacy and safety of surgical approaches for total hip arthroplasty: a systematic review and network meta-analysis. JAMA Netw Open. 2023;6(1):e2253942.
doi pubmed pmc - Kim HS, Park JW, Ha JH, Lee YK, Ha YC, Koo KH. Third-generation ceramic-on-ceramic total hip arthroplasty in patients with osteonecrosis of the femoral head: a 10- to 16-year follow-up study. J Bone Joint Surg Am. 2022;104(Suppl 2):68-75.
doi pubmed - Youngman TR, Riepen DW, Rinehart DB, Thota DR, Sun JJ, Telford CL, Huo MH. Complications of primary total hip arthroplasty in human immunodeficiency virus-positive patients with femoral head osteonecrosis. Hip Int. 2023;33(1):62-66.
doi pubmed - Hailer NP, Garland A, Rogmark C, Garellick G, Karrholm J. Early mortality and morbidity after total hip arthroplasty in patients with femoral neck fracture. Acta Orthop. 2016;87(6):560-566.
doi pubmed pmc - Baek J, Kim HS, Kim NJ, Yoo JJ. Midterm results of total hip arthroplasty for osteonecrosis of the femoral head in human immunodeficiency virus-infected patients in South Korea. Clin Orthop Surg. 2023;15(3):367-372.
doi pubmed pmc - Lee YK, Won SH, Park JW, Im JW, Ha YC, Koo KH. Cementless hip arthroplasty in patients with subchondral insufficiency fracture of the femoral head. J Bone Joint Surg Am. 2022;104(Suppl 2):84-89.
doi pubmed - Zhang Y, Dai J, Tang X, Ma J. Establishment of a predictive model for blood transfusion after femoral head replacement in elderly patients. Jt Dis Relat Surg. 2024;35(3):538-545.
doi pubmed pmc - Huang G, Han F, Wu H, Fan T, Guo W. Risk factors of lower extremity deep vein thrombosis after artificial femoral head replacement for elderly femoral neck fractures and a nomogram model construction. Altern Ther Health Med. 2024;30(8):325-331.
pubmed - Li C, Wu D, He W, Wang T, Guo H, Yang Z, Cheng X, et al. Loss of walking independence one year after primary total hip arthroplasty for osteonecrosis of the femoral head: incidence and risk prediction model. J Orthop Surg Res. 2024;19(1):580.
doi pubmed pmc - Sun Y, Miao H, Gong H, Zhang Y, Hong W. Risk factors analysis and nomogram model establishment of hidden blood loss in overweight and obese elderly patients after total hip arthroplasty. Clin Interv Aging. 2024;19:57-66.
doi pubmed pmc - Rouzrokh P, Ramazanian T, Wyles CC, Philbrick KA, Cai JC, Taunton MJ, Maradit Kremers H, et al. Deep learning artificial intelligence model for assessment of hip dislocation risk following primary total hip arthroplasty from postoperative radiographs. J Arthroplasty. 2021;36(6):2197-2203.e2193.
doi pubmed pmc - Delbarre MA, Girardon F, Roquette L, Blanc-Durand P, Hubaut MA, Hachulla E, Semah F, et al. Deep learning on bone scintigraphy to detect abnormal cardiac uptake at risk of cardiac amyloidosis. JACC Cardiovasc Imaging. 2023;16(8):1085-1095.
doi pubmed - Zhang L, Zhang R, Wang J, Chen Y, Qiao C, Shi Q, Jin Y, et al. Identification of clinical implications and potential prognostic models of chromatin regulator mutations in multiple myeloma. Clin Epigenetics. 2022;14(1):93.
doi pubmed pmc - Handelman GS, Kok HK, Chandra RV, Razavi AH, Lee MJ, Asadi H. eDoctor: machine learning and the future of medicine. J Intern Med. 2018;284(6):603-619.
doi pubmed - Li X, Shang C, Xu C, Wang Y, Xu J, Zhou Q. Development and comparison of machine learning-based models for predicting heart failure after acute myocardial infarction. BMC Med Inform Decis Mak. 2023;23(1):165.
doi pubmed pmc - Luo XQ, Kang YX, Duan SB, Yan P, Song GB, Zhang NY, Yang SK, et al. Machine learning-based prediction of acute kidney injury following pediatric cardiac surgery: model development and validation study. J Med Internet Res. 2023;25:e41142.
doi pubmed pmc - Zhang B, Lian Z, Zhong L, Zhang X, Dong Y, Chen Q, Zhang L, et al. Machine-learning based MRI radiomics models for early detection of radiation-induced brain injury in nasopharyngeal carcinoma. BMC Cancer. 2020;20(1):502.
doi pubmed pmc - Bayramoglu N, Englund M, Haugen IK, Ishijima M, Saarakkala S. Deep learning for predicting progression of patellofemoral osteoarthritis based on lateral knee radiographs, demographic data, and symptomatic assessments. Methods Inf Med. 2024;63(1-02):1-10.
doi pubmed pmc - Cabrera A, Bouterse A, Nelson M, Dietrich C, Razzouk J, Oyoyo U, Bono CM, et al. Prediction of in-hospital mortality following vertebral fracture fixation in patients with ankylosing spondylitis or diffuse idiopathic skeletal hyperostosis: machine learning analysis. Int J Spine Surg. 2024;18(1):62-68.
doi pubmed pmc - Shi H, Xiao L, Wang Z. Curative effect of artificial femoral head replacement and its effect on hip joint function and complications of senile patients with femoral intertrochanteric fracture. Exp Ther Med. 2018;16(2):623-628.
doi pubmed pmc - McLellan MA, Donnelly MR, Callan KT, Lung BE, Liu S, DiGiovanni R, McMaster WC, et al. The role of preoperative aspartate aminotransferase-to-platelet ratio index in predicting complications following total hip arthroplasty. BMC Musculoskelet Disord. 2023;24(1):934.
doi pubmed pmc - Matcovici M, Stoica I, Smith K, Davenport M. What makes a "successful" Kasai portoenterostomy "unsuccessful"? J Pediatr Gastroenterol Nutr. 2023;76(1):66-71.
doi pubmed - Arvidsson Kvissberg ME, Hu G, Chi L, Bourdon C, Ling C, ChenMi Y, Germain K, et al. Inhibition of mTOR improves malnutrition induced hepatic metabolic dysfunction. Sci Rep. 2022;12(1):19948.
doi pubmed pmc - Bohl DD, Shen MR, Hannon CP, Fillingham YA, Darrith B, Della Valle CJ. Serum albumin predicts survival and postoperative course following surgery for geriatric hip fracture. J Bone Joint Surg Am. 2017;99(24):2110-2118.
doi pubmed - Harris AB, Lantieri MA, Agarwal AR, Golladay GJ, Thakkar SC. Osteoporosis and total knee arthroplasty: higher 5-year implant-related complications. J Arthroplasty. 2024;39(4):948-953.e941.
doi pubmed - Cichos KH, McGwin G, Jr., Boyd B, Arthroplasty for Hip Fracture Consortium, Ghanem ES. Direct anterior approach total hip arthroplasty is associated with reduced 1-year mortality and surgical complications after femoral neck fracture. J Arthroplasty. 2023;38(11):2347-2354.e2342.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.