| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://jocmr.elmerjournals.com |
Original Article
Volume 16, Number 12, December 2024, pages 589-599
Association Between Chronic Kidney Disease Risk Categories and Abdominal Aortic Calcification: Insights From the National Health and Nutrition Examination Survey
Song Peng Anga, Jackson Rajendrana, Jia Ee Chiab, Pratiksha Singhc, Jose Iglesiasa, d, e
aDepartment of Internal Medicine, Rutgers Health/Community Medical Center, Toms River, NJ, USA
bDepartment of Internal Medicine, Texas Tech University Health Science Center, El Paso, TX, USA
cDepartment of Nephrology, Albany Medical College, Albany, NY, USA
dDepartment of Internal Medicine, Hackensack Meridian School of Medicine, Nutley, NJ, USA
eCorresponding Author: Jose Iglesias, Department of Internal Medicine, Hackensack Meridian School of Medicine, Nutley, NJ, USA
Manuscript submitted October 14, 2024, accepted November 30, 2024, published online December 20, 2024
Short title: CKD Risk Categories and AAC
doi: https://doi.org/10.14740/jocmr6101
| Abstract | ▴Top |
Background: Abdominal aortic calcification (AAC) is a critical indicator of cardiovascular risk, particularly in patients with chronic kidney disease (CKD). Traditional classification systems may underestimate the risk in those with moderate CKD. This study aimed to evaluate the association between CKD risk categories - defined by both estimated glomerular filtration rate (eGFR) and albuminuria - and the prevalence of severe AAC.
Methods: This cross-sectional study analyzed data from the National Health and Nutrition Examination Survey (NHANES) 2013-2014. We included adults aged ≥ 40 years who underwent imaging for AAC assessment, excluding pregnant individuals and those without AAC scores. Survey-weighted and multivariate logistic regression was employed to assess the relationship between CKD risk categories and severe AAC, adjusting for age, hypertension, and smoking history. Subgroup analyses were conducted to explore variability across demographic and clinical subgroups.
Results: We analyzed data from 3,140 participants in the NHANES, 423 (13.4%) of whom had severe AAC. The cohort was categorized into CKD risk categories 1 through 4, with the majority (76%) in stage 1. Severe AAC was more prevalent among older individuals and those with traditional cardiovascular risk factors. Initial unadjusted analyses revealed that CKD category 2 was associated with a nearly fourfold increase in severe AAC (odds ratio (OR): 3.93), while categories 3 and 4 showed 3.75-fold and over 10-fold increases, respectively (all P < 0.01). However, after adjusting for confounders, categories 2 and 4 showed higher risks of severe AAC compared to category 1, but these associations did not reach statistical significance (OR: 1.72, 95% confidence interval (CI): 0.90 - 1.86, P = 0.06 and OR: 5.70, 95% CI: 0.85 - 38.00, P = 0.07, respectively).
Conclusion: Our study offers insights that may complement the current reliance on eGFR and albuminuria in risk stratification, highlighting that CKD category 2, defined by mildly reduced eGFR and albuminuria, may be a potential marker for severe AAC. Although statistical significance was narrowly missed after full adjustment, the clinical implications remain significant, advocating for more aggressive cardiovascular risk management in this population. This understanding may contribute to evolving approaches in CKD-related cardiovascular risk assessment and inform potential intervention strategies.
Keywords: CKD; Risk categories; Abdominal aortic calcification; Cardiovascular; Risk factors; Prognosis
| Introduction | ▴Top |
Abdominal aortic calcification (AAC) is a significant indicator of systemic atherosclerosis and is associated with increased cardiovascular morbidity and mortality [1, 2]. Epidemiologically, AAC is prevalent among older adults and is strongly linked to traditional cardiovascular risk factors such as advanced age, hypertension, smoking, dyslipidemia, and diabetes mellitus [2-4]. The presence of AAC signifies a higher burden of atherosclerosis and is often considered a prognostic marker for adverse cardiovascular events. Within the last two decades, chronic kidney disease (CKD) has been found to be a significant risk factor and disease modifier for AAC. The progression of AAC can lead to increased arterial stiffness, reduced arterial compliance, and impaired blood flow, ultimately contributing to cardiovascular diseases (CVDs) and events.
Recent research has highlighted the role of various biomarkers in the pathogenesis and progression of arterial calcification. Proinflammatory biomarkers such as β2-microglobulin (B2M), fibroblast growth factor 23 (FGF23), interleukin-8 (IL-8), and IL-18 were found to be associated with arterial calcification [5]. Elevated levels of these biomarkers suggested a shared pathophysiological mechanism involving chronic inflammation, oxidative stress, and mineral metabolism dysregulation. In addition, these biomarkers may be a common pathophysiologic pathway in traditional risk factors for the development of AAC. Understanding the relationship between these biomarkers and AAC can provide insights into the underlying mechanisms driving vascular calcification and help identify individuals at higher risk for cardiovascular events.
CKD is a known risk factor for atherosclerosis because of inflammation, oxidative stress, defective calcium-phosphorus metabolism, and superimposed traditional risk factors such as smoking, diabetes, and hypertension [6]. Microalbuminuria, albuminuria, and CKD are known to be associated with increased risk of cardiovascular, cerebrovascular, and peripheral vascular diseases [7-9]. Additionally, there is a mounting body of evidence to support that microalbuminuria and albuminuria are independent risk factors for CVD in individuals with and without superimposed traditional risk factors for CVD [10]. To better understand the prognosis and severity of comorbid conditions in patients with CKD, The Kidney Disease: Improving Global Outcomes (KDIGO) 2012 guidelines recommend classifying patients based on glomerular filtration rate (GFR) and albuminuria [11]. Although multiple researchers in the past have studied the correlation of risk factors and various lab parameters and CKD, studies comparing these parameters with renal risk stratification are limited.
We aimed to study the association of risk factors for developing severe AAC. Specifically, we sought to evaluate the role of different CKD risk categories and traditional risk factors as drivers of the development of severe AAC in a nationally representative sample of the US adult population.
| Materials and Methods | ▴Top |
Study design and population
The study was conducted and reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. This cross-sectional study utilized data from the National Health and Nutrition Examination Survey (NHANES) 2013-2014. NHANES is a program designed to assess adults’ and children’s health and nutritional status in the United States through interviews, laboratory analysis, and physical examinations. The survey conducted by NHANES has regularly received IRB approval and its respective IRB protocol number is available in literature [12]. The study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
Individuals who participated in the NHANES 2013-2014 study cycle , were aged ≥ 40 years and underwent imaging for the assessment of AAC were included in the analysis. Pregnant participants and those who did not have AAC scores were excluded from the analysis. Smoking history was defined as lifetime smoking of 100 cigarettes. Hypertension, hypercholesterolemia, and diabetes mellitus were abstracted from the NHANES 2013-2014 questionnaire and examination. Patients with diabetes were defined as taking hypoglycemic medications or having a diagnosis of diabetes, having either a hemoglobin A1c (HbA1c) level of greater than 6.4% or having a fasting plasma glucose greater than 125 mg/dL. Hypertension was defined as taking antihypertensive medications, having a history of hypertension, or having a systolic blood pressure of greater than 140 mm Hg. Hypercholesterolemia was defined as either having a history of hypercholesterolemia or being on antihyperlipidemic medications.
AAC assessment
AAC was assessed using dual-energy X-ray absorptiometry (DXA) scans. NHANES 2013-2014 employed both AAC-24 (Kaupilla) and AAC-8 (Schouseboe) methods for assessing AAC [13-15]. The AAC-24 score described by Kauppila evaluates calcification of the walls of the abdominal aorta along the first and fourth lumbar vertebra as visualized on lateral lumbar radiography. The degree of calcification of the anterior and posterior wall of the aorta is scored along these vertebral segments: a score of 0 if there is no calcification, 1 if one-third or less of the aortic wall in that segment is calcified, 2 if greater than one-third but less than two-thirds of the aortic wall is calcified and 3 if greater than two-thirds of the aortic wall is calcified. The total score is the sum of anterior and posterior aortic calcification scores along each vertebral segment (0 - 6), rendering a total score of 24 [15]. Conversely, the AAC-8 score is the sum of the anterior and posterior abdominal aortic wall calcification observed along the length of L1-L4. A score of 0 if no calcification is observed along the length of a vertebral body, a score of 1 if the calcification is observed involving ≤ 1 vertebral length, 2 if > 1 but ≤ 2 vertebral lengths, 3 if > 2 but ≤ 3 vertebral lengths and 4 if > 3 vertebral lengths [13]. We define severe AAC score as greater than 3 (0 - 8 score) and greater than or equal to 5 (0 - 24 score) [14]. Further information on the AAC grading system can be found in literature [16].
CKD risk categories
The CKD risk categories (renal risk) are defined based on KDIGO 2012 guidelines and range from low to very high risk [17]. Low risk (category 1) includes individuals with normal or high GFR (≥ 90 mL/min/1.73 m2) and normal to mildly increased albuminuria (A1: < 30 mg/g), as well as those with mildly decreased GFR (60 - 89 mL/min/1.73 m2) and normal to mildly increased albuminuria (A1: < 30 mg/g). Moderately increased risk (category 2) encompasses individuals with normal or high GFR (≥ 90 mL/min/1.73 m2) and moderately increased albuminuria (A2: 30 - 299 mg/g), mildly decreased GFR (60 - 89 mL/min/1.73 m2) and moderately increased albuminuria (A2: 30 - 299 mg/g), and mildly to moderately decreased GFR (45 - 59 mL/min/1.73 m2) with normal to mildly increased albuminuria (A1: < 30 mg/g). High risk ( category 3) includes those with normal or high GFR (≥ 90 mL/min/1.73 m2) and severely increased albuminuria (A3: ≥ 300 mg/g), mildly decreased GFR (60-89 mL/min/1.73 m2) and severely increased albuminuria (A3: ≥ 300 mg/g), mildly to moderately decreased GFR (45 - 59 mL/min/1.73 m2) and moderately increased albuminuria (A2: 30 - 299 mg/g), and moderately to severely decreased GFR (30 - 44 mL/min/1.73 m2) with normal to mildly increased albuminuria (A1: < 30 mg/g). Very high risk (category 4) is characterized by individuals with mildly to moderately decreased GFR (45 - 59 mL/min/1.73 m2) and severely increased albuminuria (A3: ≥ 300 mg/g), moderately to severely decreased GFR (30 - 44 mL/min/1.73 m2) with moderately increased albuminuria (A2: 30 - 299 mg/g) or severely increased albuminuria (A3: ≥ 300 mg/g), severely decreased GFR (15 - 29 mL/min/1.73 m2) with any level of albuminuria (A1, A2, or A3), and those with kidney failure (GFR < 15 mL/min/1.73 m2) regardless of albuminuria levels (A1, A2, or A3).
The association between CKD stages, with other risk factors, and severe AAC was evaluated using multivariable logistic regression models. The current study included demographics and health condition covariates. The demographic covariates included sex, age, and race. Several anthropometric and laboratory covariates also have been included, such as body mass index (BMI, kg/m2, calculated as weight in kilograms divided by height in meters squared), serum creatinine (mg/dL), serum uric acid (mg/dL), low-density lipoprotein (LDL, mg/dL), triglycerides (mg/dL), serum total calcium (mg/dL), serum phosphorus (mg/dL), serum chloride (mmol/L), serum potassium (mmol/L), serum bicarbonate (mmol/L), serum sodium (mmol/L), serum potassium (mmol/L), 25-OH vitamin D3 (nmol/L), neutrophile count (1,000 × 103/µL), platelet count (1,000 × 103/µL), lymphocyte count (1,000 × 103/µL), Hb (g/dL), and HbA1c (%). Estimated GFR (eGFR) was calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) (no race equation) [18]. Platelet/lymphocyte ratio and neutrophile/lymphocyte ratio were evaluated as inflammatory biomarkers determined by platelet count divided by lymphocyte count, and neutrophile count divided by lymphocyte count, respectively. Missing values were substituted using multiple imputations. Data found to be missing completely at random (MCAR) were determined according to Little’s MCAR test [19].
Descriptive statistics were used to summarize the characteristics of the study population, stratified by the presence of severe AAC. All analyses were weighted and conducted using survey-specific and complex sample procedures in STATA version 17 (College State, TX, USA) to account for the complex sampling design of NHANES. Results are statistically significant if the two-sided P-value is less than 0.05. Continuous variables were summarized as means with standard deviation, and categorical variables as frequencies and percentages. Continuous variables were analyzed using univariate binary logistic regression, and categorical variables were analyzed using the Chi-squared test. Those variables found to be statistically significant by univariate analysis (P < 0.05) were entered simultaneously into a multivariable regression model. The model retained variables that remained statistically significant (P < 0.05), with odds ratio (OR) and 95% confidence intervals (CIs). Stepwise selections for logistic regression were based on the maximum likelihood ratio. For continuous variables, the OR represents the relative amount by which the probability of observing risk for severe AAC increases or decreases if the independent variable is increased by exactly one unit. ORs and their 95% CIs were determined by exponentiation of the regression coefficient and its upper and lower 95% CI, respectively.
We initially ascertained what clinical, laboratory, and demographic variables were independent risk factors associated with AAC by employing binary multivariable logistic regression. To determine if renal risk categories were associated with severe AAC, we next created logistic regression models with gradational adjustment, adding those risk factors that had been found to be independent predictors associated with severe AAC in the previous multivariable logistic regression. As GFR is included in the renal risk stratification, GFR was excluded from the models. Model 1 was unadjusted. In model 2, age was added, and in model 3, age and hypertension were added. Model 4 was additionally adjusted by age, hypertension, and smoking history. In order to determine the magnitude and significance of predefined subgroups with renal risk and severe AAC, we performed an interaction test and subgroup analysis stratified by age ≥ 65, age < 65, Caucasian race, non-Caucasian, gender, hypertension, no hypertension, diabetes, and no diabetes.
| Results | ▴Top |
Univariate analysis of participant characteristics
Of the 3,140 individuals, 423 (13.4%) were classified as having severe AAC (Fig. 1). There were marked differences in those with and without severe AAC in age, smoking history, hypertension, diabetes mellitus, blood urea nitrogen (BUN), serum chloride, eGFR, serum phosphorus, platelet count, neutrophil/lymphocyte ratio, and HbA1c. Tables 1 and 2 describe participant characteristics, comorbidities, and laboratory values. Within the setting of renal risk categories, 2,375 (76%) individuals were classified as stage 1, 584 (19%) as stage 2, 86 (3%) as stage 3, and 95 (3%) as stage 4.
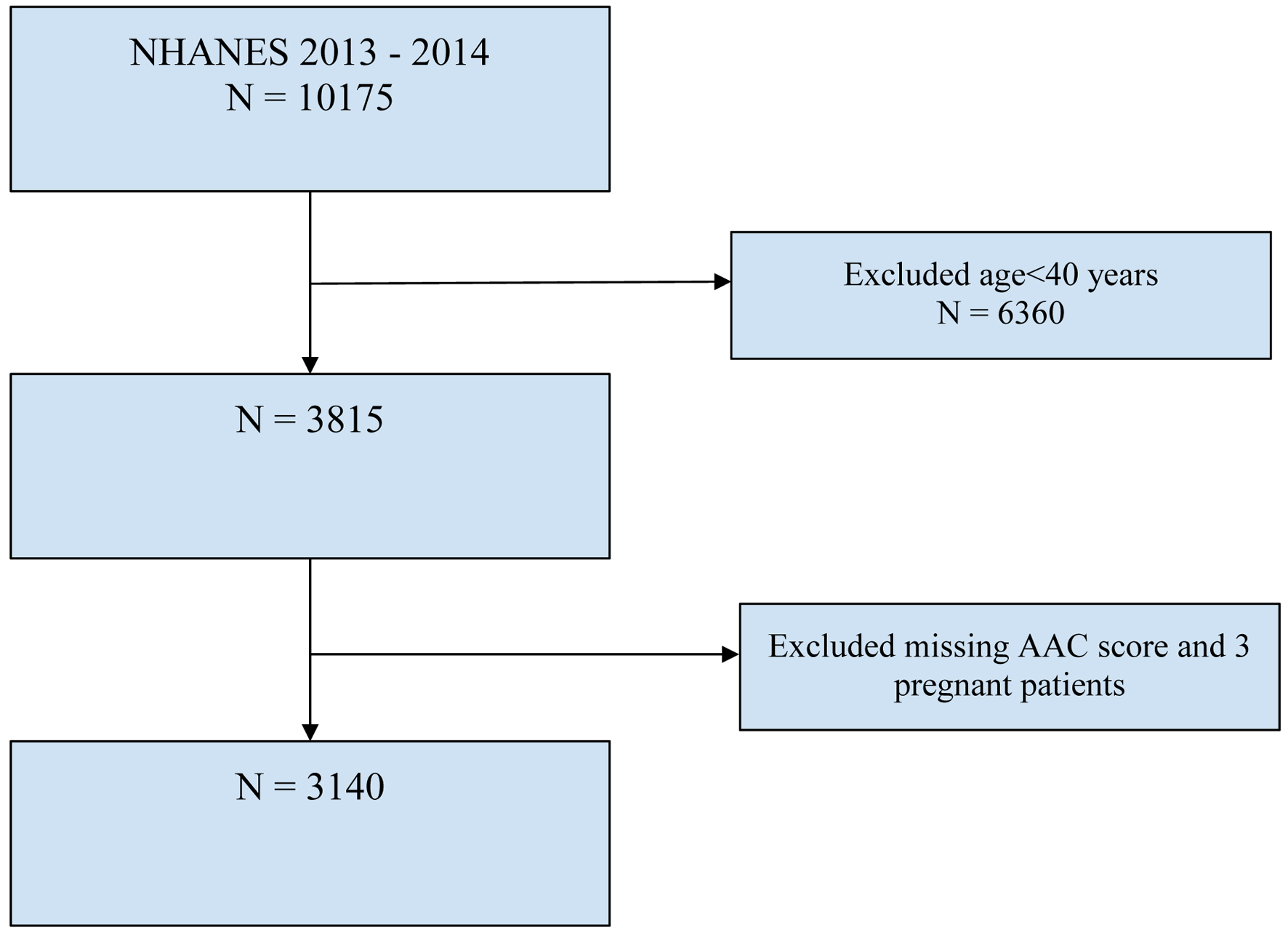 Click for large image | Figure 1. Flowchart of selection of participants. AAC: abdominal aortic calcification; NHANES: National Health and Nutrition Examination Survey. |
 Click to view | Table 1. Demographics and Laboratory Findings of Included Patients |
 Click to view | Table 2. Univariate Analysis |
Table 3 presents a multivariable logistic regression analysis examining the risk factors for severe ACC. The analysis analyzes four traditional CV risk factors: age, history of hypertension, smoking history, and eGFR. Each year of increasing age is associated with a 10% increase in the odds of severe AAC, as indicated by an OR of 1.10 (P < 0.0001). Hypertension and smoking history are also significant risk factors, with ORs of 1.83 and 1.76, respectively, suggesting that individuals with these conditions are more likely to develop severe AAC compared to their counterparts. Conversely, higher eGFR is associated with a reduced risk of severe AAC (OR: 0.98, 95% CI: 0.97 - 0.98, P = 0.004).
 Click to view | Table 3. Multivariable Logistic Regression of Risk Factors for Severe AAC |
We performed a series of multivariable logistic regressions with gradation adjustment to ascertain the relationship between renal risk categories and the development of severe AAC (Table 4). The first, unadjusted model shows strong associations, indicating significant increases in the likelihood of severe AAC as renal risk increases: category 2 shows a nearly fourfold increase (OR: 3.93), category 3 approximately a 3.75-fold increase, and category 4 over a 10-fold increase in risk, all statistically significant.
 Click to view | Table 4. Multivariate Analysis of Renal Risk for CKD and AAC |
When adjustments are made for age, the strength of these associations diminishes. In the age-adjusted model, category 2 retains a statistically significant, albeit reduced, association with severe AAC (OR: 1.8), while categories 3 and 4 see a significant drop in OR, with category 4’s wide CI suggesting high variability in the estimate. Further adjustments for hypertension show a continued decrease in OR for all categories of renal risk. The final adjustments, which include age, hypertension, and smoking history, show a slight increase in OR for categories 2 and 4 compared to the previous model, but these associations still do not reach statistical significance. Notably, category 2 is associated with a 70% increased risk of severe AAC relative to category 1 but marginally missed the statistical significance threshold (OR: 1.72, 95% CI: 0.90 - 1.86, P = 0.06).
Additionally, we performed multivariable logistic regressions with gradation adjustment to evaluate the association between CKD stages based on KDIGO 2012 guidelines and the risk of severe AAC. In the initial unadjusted model, CKD stages 3 and above are significantly associated with the risk of severe AAC. However, after adjustment for other confounders, this association attenuates (Supplementary Materials 1-3, jocmr.elmerjournals.com).
Subgroup analysis
The current subgroup analysis showed that the association between renal risk categories and severe AAC was inconsistent (Table 5). For the association between renal risk categories and severe AAC stratified into predetermined subgroups, we observed positive associations for participants in renal risk for category 4 stratified by age < 65 (OR: 14.5, 95 CI: 2.9 - 70.8), and those whose age was ≥ 65 for renal risk for CKD categories 2 and 4 (OR: 2.27, 95% CI: 1.2 - 4.35 and OR: 4.41, 95% CI: 1.15 - 16.29). When participants were stratified according to gender, we observed a positive association for renal risk categories 2, 3, 4 and severe AAC in male gender participants (OR: 4.85, 95% CI: 2.66 - 8.83; OR: 5.42, 95% CI: 1.37 - 21.5; OR: 7.99, 95% CI: 1.31 - 48.6) and renal risk category 2 and 4 in female participants (OR: 3.32, 95% CI: 1.67 - 6.57, and OR: 39.9, 95% CI: 3.20 - 498). Stratified by the presence or absence of diabetes, in those with diabetes, a positive association was found in renal risk for category 4 and severe AAC (OR: 5.29, 95% CI: 1.16 - 25.8), and in those without diabetes, a positive association was found in renal risk and severe AAC in category 2 (OR: 4.7, 95% CI: 2.54 - 8.74). Stratified by Caucasian and non-Caucasian race, among Caucasians, there was a positive association in renal risk categories 2, 3 and 4 and severe AAC (OR: 3.93, 95% CI: 1.8 - 8.5; OR: 4.57, 95% CI: 1.3 - 15.9; and OR: 11, 95% CI: 1.5 - 80.6, respectively). Among non-Caucasians, there was a positive association among those in renal risk category 4 and severe AAC (OR: 14.5, 95% CI: 3 - 71). Stratified by hypertension and no hypertension, a positive association was found in renal risk categories 2 and 4 and severe AAC in the hypertension subgroup (OR: 3.01, 95% CI: 1.8 - 5.01; OR: 6.82, 95% CI: 1.90 - 24.47), and among the non-hypertension subgroup, a positive association was found in renal risk category 2 and severe AAC (OR: 3.59, 95% CI: 1.35 - 9.54). Predefined subgroup analysis and interaction test demonstrated that there was no significant interaction across all subgroups between renal risk categories and severe AAC: age (P = 0.453), gender (P = 0.714), diabetes (P = 0.288), race (P = 0.818), and hypertension (P = 0.411), indicating that there was no significant dependence of age, gender, diabetes, race, and hypertension.
 Click to view | Table 5. Subgroup Analyses Based on Patients’ Demographics and Comorbidities and Renal Risk Categories |
| Discussion | ▴Top |
The current study underlines the complexities of traditional risk factors in developing severe AAC. We show that traditional risk factors for severe AAC, such as hypertension, advancing age, and smoking history, are independently associated with severe AAC. In addition, eGFR was negatively associated with severe AAC, with participants with higher eGFR demonstrating less evidence of severe AAC. Although there was an association with increases in renal risk with severe AAC, these findings were inconsistent despite there being no interaction between renal risk and traditional risk factors for severe AAC.
Consistent with other studies, the current study found traditional risk factors of advancing age and hypertension to be associated with severe AAC [20]. There is a growing body of evidence showing that advancing age is associated with both the presence and severity of aortic calcification [21, 22]. Likewise, several studies have provided evidence that cigarette smoking is associated with AAC [21-23]. Witteman et al, in a study with a 9-year follow-up, revealed that compared with non-smokers, smoking 1 - 9 cigarettes a day was associated with a 40% risk of developing AAC, those who smoke 10 - 19 cigarettes per day demonstrated a 100% risk of AAC and those who smoked greater than 20 cigarettes a day, the risk rose to 130% [24]. Hypertensive individuals are at risk for the development of atherosclerosis [20]. Several studies indicate that compared to non-hypertensive individuals, hypertensive subjects have more severe AAC [20, 23, 25].
Advancing age is associated with increased circulating reactive oxygen and nitrogen species, leading to oxidative stress inflammation and endothelial dysfunction [26]. Aging is also associated with an imbalance in circulating antioxidants leading to a pro-oxidant state, an imbalance between circulating vasodilators and vasoconstrictors, endothelial dysfunction and attenuation of nitric oxide-mediated endothelial-derived vasodilation [27-29]. Inflammatory proteins and cytokines such as IL-1β, tumor necrosis factor (TNF)-α, IL-6, and C-reactive protein (CRP) are elevated in advancing age [30]. This proinflammatory pro-oxidant state leads to vascular remodeling and atherosclerosis. The above proinflammatory and pro-oxidant state is not dissimilar in patients with hypertension and cigarette smoking history [31, 32].
Over the last two decades, evidence has established that CKD may be a significant risk factor for the development of vascular calcification [20, 33, 34]; in contrast to traditional risk factors such as hypertension and smoking, which usually involve intimal calcification, individuals with CKD, like those with diabetes also develop calcification of the tunica media. In addition, CKD is a pro-oxidant proinflammatory state characterized by endothelial dysfunction and vascular remodeling [20, 23, 35].
Wang et al studied the relationship between eGFR and the risk of AAC. In their study of approximately 3,000 participants, it was observed that there was a U-shaped association between eGFR and AAC score, with an inflection point of 76.43 mL/min/1.73 m2. In other words, participants with eGFR beyond or lower than the inflection point are associated with a higher AAC score [36]. A similar U-shaped relationship has been shown in a meta-analysis of 14 studies analyzing the association of eGFR and mortality [37]. Investigators demonstrated a significant exponential increase in mortality risk at low eGFR levels. For instance, this risk became statistically significant around an eGFR of 60 mL/min/1.73 m2 and was found to be twice as high at eGFR levels between 30 and 45 mL/min/1.73 m2 compared to optimal eGFR levels, independent of albuminuria. Mortality risk remained relatively constant at eGFR levels of 75 - 105 mL/min/1.73 m2 but increased above 105 mL/min/1.73 m2, particularly for all-cause mortality. The idea of increased risk of atherosclerosis or other cardiovascular outcomes at a higher eGFR warrants attention. Several theories may explain the latter scenario, including the measurement discrepancy with the overestimation of eGFR with the modification of diet in renal disease (MDRD) equation, sarcopenia due to malnutrition, and the higher prevalence of other traditional cardiovascular risk factors among those with higher eGFR.
An intriguing finding of our study indicates that the significance of CKD risk category 3 in relation to AAC was notably attenuated after adjusting for confounders. This reduction in significance may be attributed to several factors. First, the potential for measurement error, particularly because of the reliance on a one-time urine sample collection, could have introduced variability that weakened the observed associations. Additionally, the overestimation of eGFR, which is not adjusted for lean body mass, might have skewed the categorization, leading to an inaccurate classification of patients into CKD risk categories. The possibility of a curvilinear relationship between eGFR and AAC also suggests that the risk might increase significantly between lower categories but plateau or diminish in higher categories like category 3, as shown by Wang et al [36]. Furthermore, the sample size for category 3 might have been insufficient to detect a significant effect, particularly after adjusting for multiple covariates. Notably, while the data emphasized a stronger association for category 2 compared to category 1, category 3 did not demonstrate the same significance level, potentially because of these factors.
Our findings underscore that CKD risk category 2, which includes individuals with mildly reduced eGFR (40 - 59 mL/min/1.73 m2) and mild albuminuria (30 - 300 mg/g), may offer a more effective tool for capturing cardiovascular risk compared to the traditional eGFR-based classification system. The conventional classification system typically emphasizes an eGFR below 60 as the critical threshold for increased risk. However, this approach may mask or overlook a significant population within category 2 who may inherently carry a higher risk of severe AAC. By integrating moderately increased albuminuria with a mildly reduced eGFR, category 2 potentially identifies patients who might not be flagged by the traditional eGFR cutoff alone but still carry a substantial risk of severe AAC.
Limitations
One of the primary limitations of this study stems from the use of data derived from the NHANES. As a cross-sectional survey, NHANES provides a snapshot of data at a single time, limiting our ability to infer causality or observe temporal changes in risk factors and outcomes. The nature of the NHANES survey also introduces the possibility of recall bias, particularly for self-reported data such as medical history, lifestyle factors, and medication use. Participants might not accurately recall or report their information, leading to potential misclassification and measurement error. Furthermore, the reliance on single measurements of eGFR and albuminuria is a significant limitation. Kidney function and proteinuria are dynamic, and single-point measurements may not accurately reflect the long-term status of these parameters. Another limitation is the potential for systematic errors in estimating eGFR, such as individual variations in muscle mass, which could lead to the potential overestimation or underestimation of kidney function. This systematic error could have affected the categorization of CKD risk, particularly in distinguishing between categories 2 and 3. Finally, the survey’s cross-sectional design limits our ability to fully adjust for confounding variables. While adjustments were made for key comorbidities such as age, hypertension, and smoking history, the possibility of residual confounding remains, particularly for unmeasured or inadequately measured variables. In addition, in terms of smoking history, there is significant amount of missing data on the years smoked and number of cigarettes used per day in the NHANES database. We have opted to use smoking of at least 100 cigarettes since this variable has the least missing data. Furthermore, the data on pharmacotherapy are not extracted and are beyond the scope of data collection in our study. Nevertheless, we believe that this represents an important avenue for future research. Overall, these limitations suggest that while the NHANES dataset provides valuable insights into population health, the findings should be interpreted cautiously, particularly when extrapolating to clinical practice or informing policy decisions. Further, longitudinal studies are needed to confirm these associations and better understand the progression of CKD and its related risks.
Conclusion
Our study reveals that traditional CKD risk stratification may underestimate cardiovascular risk, particularly in patients categorized as CKD category 2, where mildly reduced eGFR and albuminuria are associated with a heightened risk of severe AAC. Although the associations did not reach statistical significance after adjusting for confounders, the findings still carry significant clinical implications. They suggest that patients in this category could benefit from more aggressive cardiovascular risk management. The study’s limitations include its cross-sectional design, which precludes causal inferences, and potential measurement errors related to single-time assessments of eGFR and albuminuria. The reliance on survey data might introduce bias due to self-reported information. Despite these limitations, our findings emphasize the need to refine CKD-related cardiovascular risk assessment to better identify and mitigate risks in this population, supporting the development of targeted interventions and guiding future research to improve patient outcomes.
| Supplementary Material | ▴Top |
Suppl 1. Association between CKD stages and severe AAC (unadjusted).
Suppl 2. Multivariable logistic regression analysis of CKD stages and AAC adjusted for age and hypertension.
Suppl 3. Multivariable logistic regression analysis of CKD stages and AAC adjusted for age, hypertension, and smoking history.
Acknowledgments
None to declare.
Financial Disclosure
All the authors had no financial disclosure.
Conflict of Interest
All the authors had no conflict of interest.
Informed Consent
Informed consents were obtained by National Center for Health Statistics and details of consent documents are available at https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/documents.aspx?BeginYear=2013.
Author Contributions
SPA and JI: study conception and design; SPA, JR, JEC, PS, and JI: data acquisition, analysis, or interpretation; SPA, JR, JEC, and JI were involved in drafting the manuscript; SPA and JI critically revised the manuscript. All authors provided final approval and agreed to be accountable for all aspects of work ensuring integrity and accuracy.
Data Availability
The authors declare that data supporting the findings of this study are available within the article and its supplementary information files.
Abbreviations
AAC: abdominal aortic calcification; Apo B: apolipoprotein B; CI: confidence interval; CKD: chronic kidney disease; eGFR: estimated glomerular filtration rate; Hb: hemoglobin; HDL: high-density lipoprotein; LDL: low-density lipoprotein; KDIGO: Kidney Disease, Improving Global Outcomes; NHANES: National Health and Nutrition Examination Survey; OR: odds ratio; SE: standard error
| References | ▴Top |
- Bartstra JW, Mali W, Spiering W, de Jong PA. Abdominal aortic calcification: from ancient friend to modern foe. Eur J Prev Cardiol. 2021;28(12):1386-1391.
doi pubmed - Leow K, Szulc P, Schousboe JT, Kiel DP, Teixeira-Pinto A, Shaikh H, Sawang M, et al. Prognostic value of abdominal aortic calcification: a systematic review and meta-analysis of observational studies. J Am Heart Assoc. 2021;10(2):e017205.
doi pubmed - Horbal SR, Derstine BA, Brown E, Su GL, Wang SC, Holcombe SA. Reference distributions of aortic calcification and association with Framingham risk score. Sci Rep. 2023;13(1):9421.
doi pubmed - Rahman EU, Chobufo MD, Farah F, Elhamdani A, Khan A, Thompson EA, Aronow WS, et al. Prevalence and risk factors for the development of abdominal aortic calcification among the US population: NHANES study. Arch Med Sci Atheroscler Dis. 2021;6:e95-e101.
doi pubmed - Kiu Weber CI, Duchateau-Nguyen G, Solier C, Schell-Steven A, Hermosilla R, Nogoceke E, Block G. Cardiovascular risk markers associated with arterial calcification in patients with chronic kidney disease Stages 3 and 4. Clin Kidney J. 2014;7(2):167-173.
doi pubmed - Sarnak MJ, Amann K, Bangalore S, Cavalcante JL, Charytan DM, Craig JC, Gill JS, et al. Chronic kidney disease and coronary artery disease: JACC State-of-the-Art review. J Am Coll Cardiol. 2019;74(14):1823-1838.
doi pubmed - de Zeeuw D, Parving HH, Henning RH. Microalbuminuria as an early marker for cardiovascular disease. J Am Soc Nephrol. 2006;17(8):2100-2105.
doi pubmed - Weir MR. Microalbuminuria and cardiovascular disease. Clin J Am Soc Nephrol. 2007;2(3):581-590.
doi pubmed - Barzilay JI, Farag YMK, Durthaler J. Albuminuria: an underappreciated risk factor for cardiovascular disease. J Am Heart Assoc. 2024;13(2):e030131.
doi pubmed - Arnlov J, Evans JC, Meigs JB, Wang TJ, Fox CS, Levy D, Benjamin EJ, et al. Low-grade albuminuria and incidence of cardiovascular disease events in nonhypertensive and nondiabetic individuals: the Framingham Heart Study. Circulation. 2005;112(7):969-975.
doi pubmed - Murton M, Goff-Leggett D, Bobrowska A, Garcia Sanchez JJ, James G, Wittbrodt E, Nolan S, et al. Burden of chronic kidney disease by KDIGO categories of glomerular filtration rate and albuminuria: a systematic review. Adv Ther. 2021;38(1):180-200.
doi pubmed - https://www.cdc.gov/nchs/nhanes/irba98.htm.
- Schousboe JT, Wilson KE, Kiel DP. Detection of abdominal aortic calcification with lateral spine imaging using DXA. J Clin Densitom. 2006;9(3):302-308.
doi pubmed - Ramos Barron MC, Pariente Rodrigo E, Arias Lago M, Cepeda Blanco JL, Casal Calvo A, Landeras Alvaro R, Hernandez Hernandez JL. Radiologic assessment of abdominal aortic calcifications, atherosclerotic burden levels and statistical bias affecting the reliability. Radiography (Lond). 2021;27(2):340-345.
doi pubmed - Kauppila LI, Polak JF, Cupples LA, Hannan MT, Kiel DP, Wilson PW. New indices to classify location, severity and progression of calcific lesions in the abdominal aorta: a 25-year follow-up study. Atherosclerosis. 1997;132(2):245-250.
doi pubmed - https://wwwn.cdc.gov/Nchs/Nhanes/2013-2014/DXXAAC_H.htm.
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Inter Suppl. 2013;3:1-150.
- Munch PV, Heide-Jorgensen U, Jensen SK, Birn H, Vestergaard SV, Frokiaer J, Sorensen HT, et al. Performance of the race-free CKD-EPI creatinine-based eGFR equation in a Danish cohort with measured GFR. Clin Kidney J. 2023;16(12):2728-2737.
doi pubmed - Li C. Little's test of missing completely at random. The Stata Journal. 2013;13:795-809.
doi - Jayalath RW, Mangan SH, Golledge J. Aortic calcification. Eur J Vasc Endovasc Surg. 2005;30(5):476-488.
doi pubmed - Allison MA, Criqui MH, Wright CM. Patterns and risk factors for systemic calcified atherosclerosis. Arterioscler Thromb Vasc Biol. 2004;24(2):331-336.
doi pubmed - Reaven PD, Sacks J, Investigators for the Veterans Affairs Cooperative Study of Glycemic Control, Complications in Diabetes Mellitus Type. Reduced coronary artery and abdominal aortic calcification in Hispanics with type 2 diabetes. Diabetes Care. 2004;27(5):1115-1120.
doi pubmed - Matsushita M, Nishikimi N, Sakurai T, Nimura Y. Relationship between aortic calcification and atherosclerotic disease in patients with abdominal aortic aneurysm. Int Angiol. 2000;19(3):276-279.
pubmed - Witteman JC, Grobbee DE, Valkenburg HA, van Hemert AM, Stijnen T, Hofman A. Cigarette smoking and the development and progression of aortic atherosclerosis. A 9-year population-based follow-up study in women. Circulation. 1993;88(5 Pt 1):2156-2162.
doi pubmed - Kimura K, Saika Y, Otani H, Fujii R, Mune M, Yukawa S. Factors associated with calcification of the abdominal aorta in hemodialysis patients. Kidney Int Suppl. 1999;71:S238-241.
doi pubmed - Izzo C, Vitillo P, Di Pietro P, Visco V, Strianese A, Virtuoso N, Ciccarelli M, et al. The Role of Oxidative Stress in Cardiovascular Aging and Cardiovascular Diseases. Life (Basel). 2021;11(1):60.
doi pubmed - Higashi Y, Kihara Y, Noma K. Endothelial dysfunction and hypertension in aging. Hypertens Res. 2012;35(11):1039-1047.
doi pubmed - Jia G, Aroor AR, Jia C, Sowers JR. Endothelial cell senescence in aging-related vascular dysfunction. Biochim Biophys Acta Mol Basis Dis. 2019;1865(7):1802-1809.
doi pubmed - Herrera MD, Mingorance C, Rodriguez-Rodriguez R, Alvarez de Sotomayor M. Endothelial dysfunction and aging: an update. Ageing Res Rev. 2010;9(2):142-152.
doi pubmed - Ferrucci L, Corsi A, Lauretani F, Bandinelli S, Bartali B, Taub DD, Guralnik JM, et al. The origins of age-related proinflammatory state. Blood. 2005;105(6):2294-2299.
doi pubmed - Elisia I, Lam V, Cho B, Hay M, Li MY, Yeung M, Bu L, et al. The effect of smoking on chronic inflammation, immune function and blood cell composition. Sci Rep. 2020;10(1):19480.
doi pubmed - Ardiana M, Santoso A, Hermawan HO, Nugraha RA, Pikir BS, Suryawan IGR. Acute effects of cigarette smoke on Endothelial Nitric Oxide synthase, vascular cell adhesion molecule 1 and aortic intima media thickness. F1000Res. 2021;10:396.
doi pubmed - Porter CJ, Stavroulopoulos A, Roe SD, Pointon K, Cassidy MJ. Detection of coronary and peripheral artery calcification in patients with chronic kidney disease stages 3 and 4, with and without diabetes. Nephrol Dial Transplant. 2007;22(11):3208-3213.
doi pubmed - Sigrist M, Bungay P, Taal MW, McIntyre CW. Vascular calcification and cardiovascular function in chronic kidney disease. Nephrol Dial Transplant. 2006;21(3):707-714.
doi pubmed - Jankowski J, Floege J, Fliser D, Bohm M, Marx N. Cardiovascular disease in chronic kidney disease: pathophysiological insights and therapeutic options. Circulation. 2021;143(11):1157-1172.
doi pubmed - Wang L, Li Q, Su B, Zhang E, Zhang S, Tu H, Zhang L, et al. The estimated glomerular filtration rate was U-shaped associated with abdominal aortic calcification in US adults: findings from NHANES 2013-2014. Front Cardiovasc Med. 2023;10:1261021.
doi pubmed - Chronic Kidney Disease Prognosis Consortium, Matsushita K, van der Velde M, Astor BC, Woodward M, Levey AS, de Jong PE, et al. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet. 2010;375(9731):2073-2081.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.