| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://jocmr.elmerjournals.com |
Original Article
Volume 16, Number 12, December 2024, pages 578-588
The Impact on Patient Prognosis of Changes to the Method of Notifying Staff About Accepting Patients With Out-of-Hospital Cardiac Arrest
Youichi Inouea, j, Keisuke Okamurab, c, j, k, Hideaki Shimadad, Shinobu Watakabea, Shiori Hirayamaa, Machiko Hirataa, Ayaka Kusudaa, Arisa Matsumotoa, Miki Inouea, Emi Matsuishia, Mizuki Yamadaa, Sachiko Iwanagae, Shogo Narumie, Shiki Nakayamaf, Hideto Sakob, c, Akihiro Udob, Kenichiro Taniguchib, Shogo Morisakib, Souichiro Ideg, Yasuyuki Nomotoh, Shin-ichiro Miurac, Osamu Imakyured, Ichiro Imamurai
aEmergency Room, Imamura Hospital, Tosu, Saga, Japan
bDepartment of Cardiology and Cardiovascular Center, Imamura Hospital, Tosu, Saga, Japan
cDepartment of Cardiology, Fukuoka University School of Medicine, Fukuoka, Fukuoka, Japan
dClinical Research Support Center, Fukuoka University Chikushi Hospital, Chikushino, Fukuoka, Japan
eSaga University Hospital Trauma and Resuscitation, Saga, Saga, Japan
fDepartment of Emergency, Takagi Hospital, Ookawa, Fukuoka, Japan
gDepartment of Respiratory Medicine, Imamura Hospital, Tosu, Saga, Japan
hDepartment of Neurosurgery, Imamura Hospital, Tosu, Saga, Japan
iDepartment of Surgery, Imamura Hospital, Tosu, Saga, Japan
jThese authors contributed equally to this work.
kCorresponding Author: Keisuke Okamura, Department of Cardiology and Cardiovascular Center, Imamura Hospital, Tosu, Saga 841-0061, Japan
Manuscript submitted October 19, 2024, accepted December 11, 2024, published online December 20, 2024
Short title: Notifying Staff About Cardiac Arrest
doi: https://doi.org/10.14740/jocmr6111
| Abstract | ▴Top |
Background: Our hospital is a designated emergency hospital and accepts many patients with out-of-hospital cardiac arrest (OHCA). Previously, after receiving a direct call from emergency services to request acceptance of an OHCA patient, the emergency room (ER) chief nurse notified medical staff. However, this method delayed ER preparations, so a Code Blue system (CB) was introduced in which the pending arrival of an OHCA patient was broadcast throughout the hospital.
Methods: In this study, we retrospectively analyzed the impact of introducing CB at our hospital on OHCA patient prognosis to examine whether the introduction of CB is clinically meaningful. We compared consecutive cases treated before introduction of the CB (March 3, 2022, to March 22, 2023) with those treated afterwards (March 23, 2023, to July 23, 2024).
Results: A total of 30 cases per group were included. The mean number of medical staff present at admissions increased significantly from 5.4 ± 0.6 to 15.0 ± 3.0 (P < 0.001). Although not statistically significant, the introduction of the CB increased the return of spontaneous circulation (ROSC) rate from 20% to 30%, survival to discharge rate from 3% to 10%, and social reintegration rate from 0% to 3%. ROSC occurred in 15 patients. Among OHCA patients with cardiac disease, the ROSC rate tended to increase from 0% to 43% (P = 0.055). In addition, in OHCA patients with cardiac disease whose electrocardiogram initially showed ventricular fibrillation or pulseless electrical activity, the ROSC rate increased from 0% to 100%. ROSC tended to be influenced by the total number of staff and physicians present and the number of staff such as medical clerks, clinical engineers, and radiology technicians (P = 0.095, 0.076, 0.088, respectively).
Conclusions: Introduction of a CB may increase the ROSC rate and the number of patients surviving to discharge. It also appears to improve the quality of medical care by quickly gathering all necessary medical staff so that they can perform their predefined roles.
Keywords: Emergency room; Cardiopulmonary resuscitation; Return of spontaneous circulation; Out-of-hospital cardiac arrest
| Introduction | ▴Top |
Our hospital is an emergency hospital that accepts about 100 out-of-hospital cardiac arrest (OHCA) cases per year. Previously, when an emergency ambulance was headed for the emergency room (ER), the ER chief nurse first received a direct call from emergency services and then used a personal handy phone system (PHS; a low-powered wireless communication service phone used in Japan) to contact the emergency duty physician and medical clerks (Fig. 1a). The medical clerk then informed other relevant staff members via the loudspeaker of the in-hospital landline phone. Although staff were informed within 1 min of the emergency services call, it sometimes took more than 2 to 3 min for staff to arrive in the ER, depending on the situation. Furthermore, if the involved staff members were not near the loudspeaker, they may not have heard the announcement. For these reasons, when expecting a critically ill patient such as one with OHCA, the ER nurse also used their PHS to call each relevant staff member in advance. However, OHCA patients usually arrive within 3 to 7 min after the direct call from emergency services. Therefore, if the notification system did not work smoothly, OHCA patients would arrive without sufficient staff being present. The arrival of staff was often delayed because the ER nurse had to concentrate on calling all staff individually. Our hospital is a medium-sized facility (with approximately 200 beds), so unlike large, critical care centers, it is not able to continuously have enough stand-by staff in the ER.
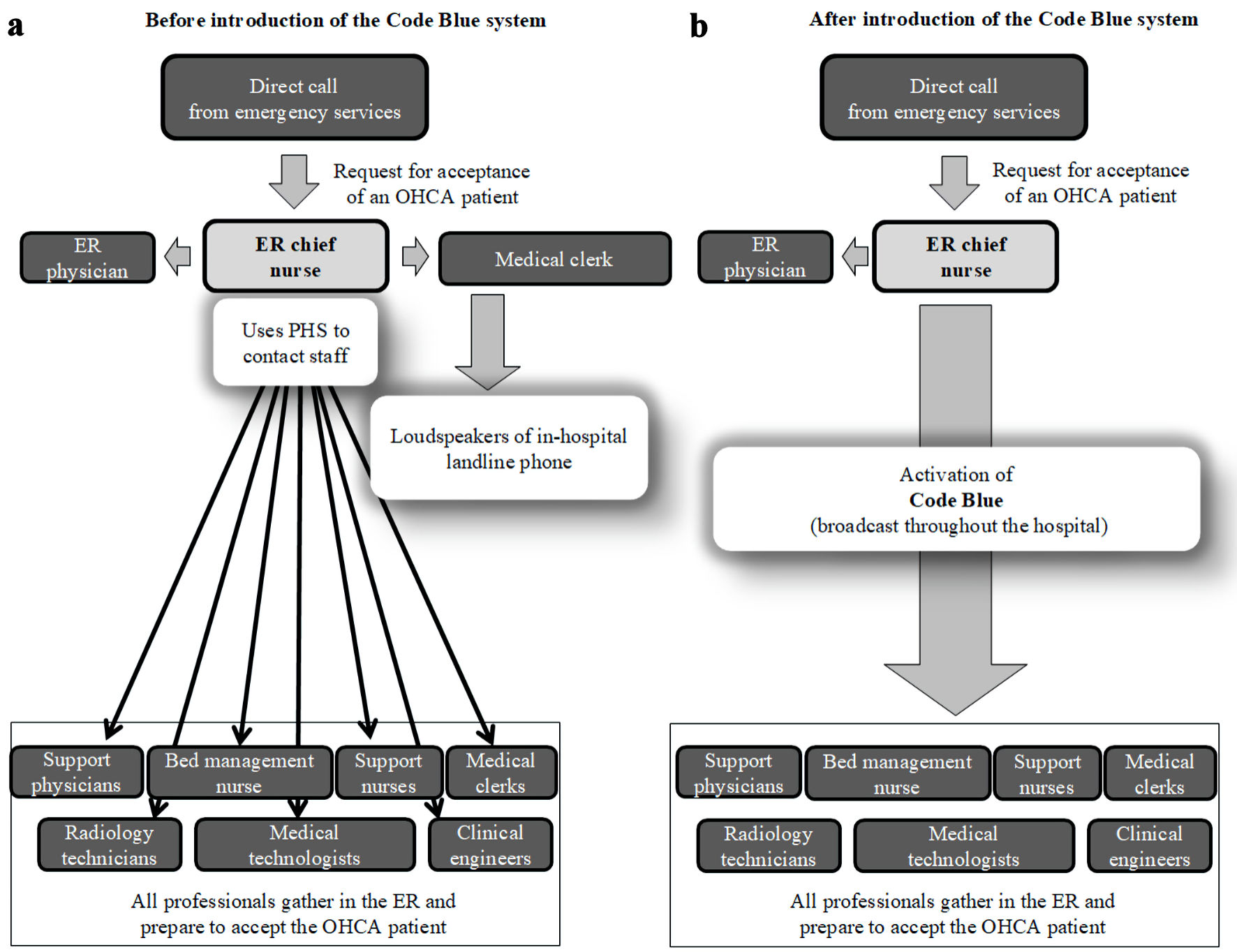 Click for large image | Figure 1. Comparison of communication systems used to gather staff in the ER in preparation for accepting OHCA patients. (a) Situation before introduction of the Code Blue system. (b) After the introduction of the Code Blue system. For example, if a patient with OHCA will arrive in 10 min, the ER nurse will twice broadcast “Code Blue, Code Blue, 10 minutes” via the Code Blue system. ER: emergency room; OHCA: out-of-hospital cardiac arrest; PHS: personal handy phone system. |
To provide advanced medical care in an ER, a system is required that enables staff to convene quickly, which in turn allows them to perform tasks according to their expertise and profession. Therefore, in March 2023, we introduced a Code Blue system (CB) at our hospital to improve the method for quickly convening staff from various departments in preparation for the arrival of an OHCA patient. We expected that the introduction of this system would improve the quality of medical care, because medical staff would be assembled more quickly and able to take on their predefined roles. However, it remained unclear whether introduction of the CB actually improved patient prognosis. Although many reports have been published on in-hospital emergency response systems, such as medical emergency teams [1] and rapid response systems [2], there is surprisingly little literature on developing systems for accepting OHCA patients, even though the development of such a system can be expected to have a major impact on clinical practice. Therefore, we retrospectively investigated the changes in prognosis of OHCA patients after the introduction of the CB at our hospital to examine whether the introduction of CB was clinically meaningful.
| Materials and Methods | ▴Top |
Details of the CB
On March 23, 2023, the method used to convene staff when accepting OHCA patients was changed from PHS calls and broadcast via the loudspeaker of the in-hospital landline phone to a CB, i.e., a hospital-wide broadcast (Fig. 1b). The CB was activated by the ER chief nurse during the day shift after they received a direct call from emergency services about an incoming OHCA patient, including those with return of spontaneous circulation (ROSC) after cardiac arrest and those with post-resuscitation shock. However, the system was not activated if patients had already signed a do-not-resuscitate order. During non-day shift hours, the conventional method continued to be used to gather staff, as it was not possible to broadcast information to the entire hospital at night, and there were few staff members in the hospital to begin with.
When the CB was activated, the following staff members convened in the ER: emergency and support physicians; ER chief nurses; ER, support, and bed management nurses; clinical engineers (medical engineers); radiology technicians; medical technologists; and medical clerks. This system ensured that at least 10 staff members were present in the ER when emergency services arrived with an OHCA patient. The general roles of these staff members had been clarified in advance (Table 1). The staff members performed the initial treatment, and once their respective duties were completed, they returned to their usual tasks. The ever-changing patient information, treatment details, and progress were recorded on a whiteboard and shared among the staff.
 Click to view | Table 1. Main Roles of Medical Staff When the CB Is Activated |
Study population
Participants were consecutive OHCA patients (including patients with ROSC before arrival at the hospital), who were admitted to our hospital after the introduction of the CB (After CB group), and the same number of consecutive OHCA patients admitted before the introduction of the CB (Before CB group). Both groups were limited to cases who visited the hospital during the day shift (Fig. 2).
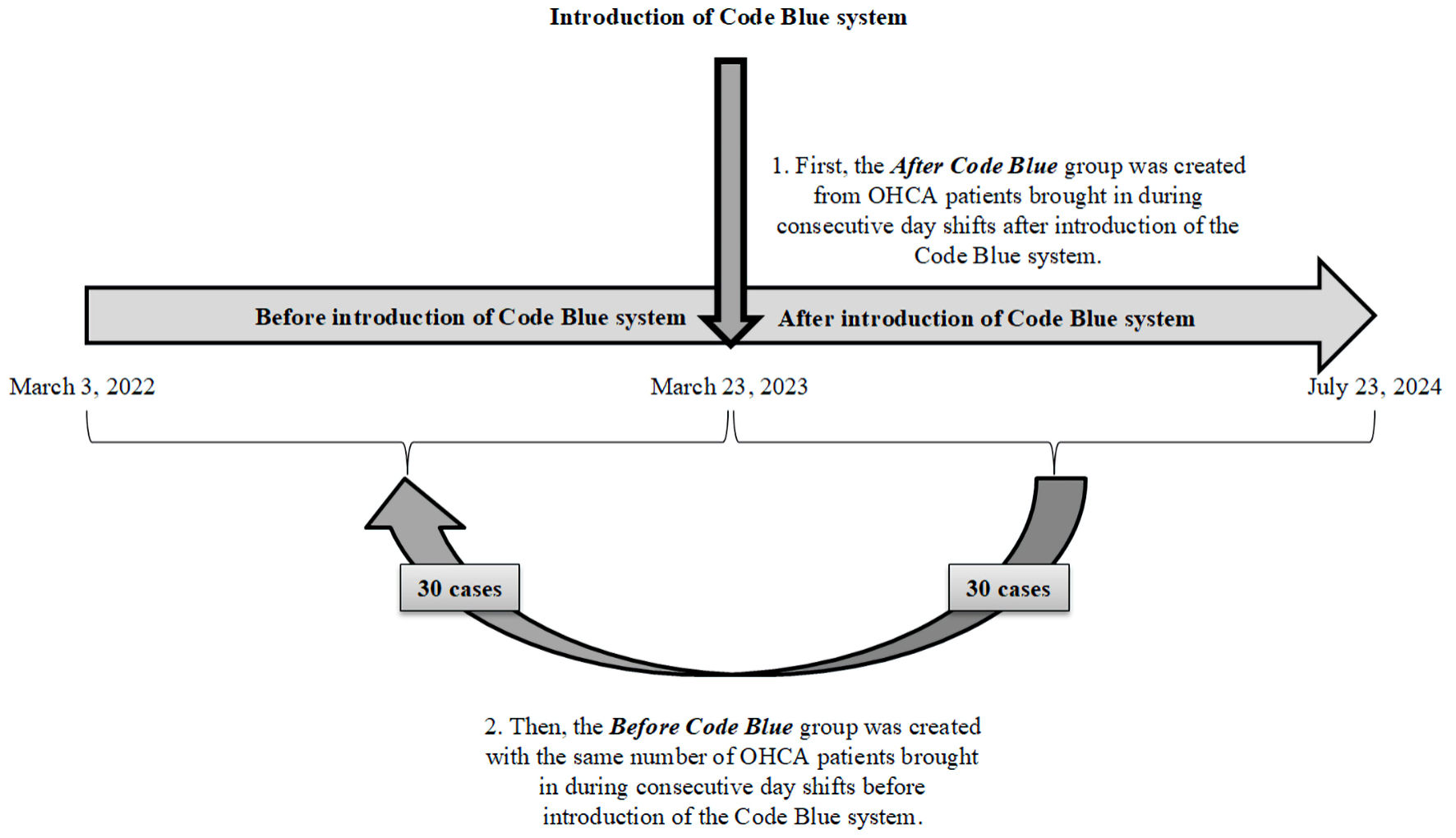 Click for large image | Figure 2. Patient enrollment. Participants were consecutive OHCA patients (including patients with return of spontaneous circulation before arrival at the hospital) who were admitted to our hospital before and after introduction of the Code Blue system. All participants were admitted during the daytime shift. Patients in the After CB group (n = 30) were admitted from March 23, 2023, to July 31, 2024, and patients in the Before CB group were admitted from March 30, 2022, to March 22, 2023. OHCA: out-of-hospital cardiac arrest. |
The study protocol was approved by Fukuoka University Medical Ethics Review Board (approval no. C24-03-003) and the Ethics Review Board of Imamura Hospital (approval no. 6-3). The study was performed in compliance with the ethical standards of the responsible institution on human subjects and with the Declaration of Helsinki. Patients were informed about the study by notices posted in the hospital and were able to opt out via the hospital website.
Outcomes
The main outcome was the ROSC rate during the day shift. The ROSC rate was the percentage of patients who achieved ROSC even once during the period from the onset of cardiac arrest till treatment in the ER to those who were transported due to OHCA.
Sample size estimation
The ROSC rate during day shifts was assumed to be 5% in the Before CB group and 30% in the After CB group. This rate of Before CB group was assumed by calculation from previous discharge summaries at our hospital. Assuming a 70% probability of detecting significance at the 5% level, a total of 52 patients were required. These values were calculated by “sealed envelope TM”.
Exclusion criteria
Exclusion criteria were defined as patients for whom the response policy in the case of an emergency was decided in advance as “do not attempt resuscitate”, patients who expressed their intention to refuse the use of existing information, and patients who were transported during non-day shift hours.
Statistical analysis
Statistical analyses were performed with the EZR application (version 1.61) [3]. To analyze differences between the two groups, the Student’s t-test was performed if normality was present and the Levene test indicated equal variance, and the Welch test was performed if the Levene test did not indicate equal variance. If normality was not present, the Mann-Whitney test was used. To analyze changes over time, paired t-test was used if normality was confirmed, and Wilcoxon single-rank test was used if it was not. The Chi-square test was used to analyze associations between categories. Numerical results were expressed as mean (standard deviation (SD)), median (interquartile range (IQR)), or number (frequency or proportion). A P value of less than 0.05 was considered statistically significant.
| Results | ▴Top |
The After CB group comprised 30 consecutive OHCA patients who were treated during the daytime shift from March 23, 2023, to July 31, 2024, and the Before CB group comprised 30 consecutive OHCA patients who were treated during the daytime shift from March 30, 2022, to March 22, 2023 (Fig. 2). Table 2 compares the patient characteristics between the Before and After CB groups. There were no significant differences in basic characteristics, bystander cardiopulmonary resuscitation (CPR), or adrenaline administration in the emergency ambulance.
 Click to view | Table 2. Characteristics of Patients With OHCA Admitted Before and After Introduction of the Code Blue System |
Although the time from arrival at the hospital to administration of adrenaline did not change after the introduction of the CB, the amount of adrenaline used in the ER tended to decrease.
Figure 3 shows the changes in the total number of medical staff and in the number of physicians, nurses, and co-medical staff (i.e., medical clerks, clinical engineers, and radiology technicians) gathered in the ER. After the introduction of the CB, the total number of medical staff and the number of staff from each professional group increased significantly.
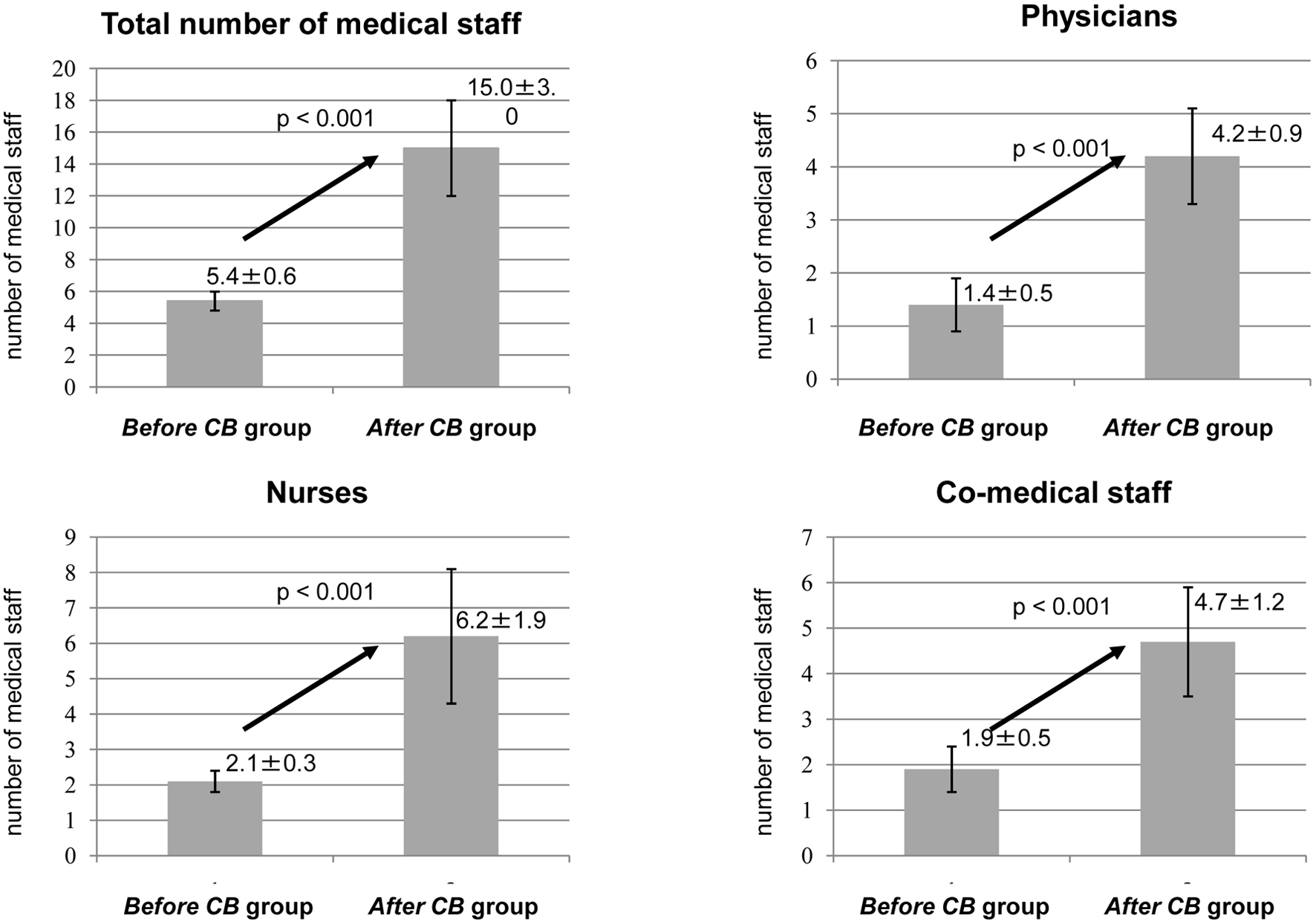 Click for large image | Figure 3. Changes in the number of medical staff present in the emergency room when out-of-hospital cardiac arrest patients arrived. CB: Code Blue system. |
Figure 4 shows the changes in the ROSC rate, survival to discharge rate, and social reintegration (patients with a Cerebral Performance Category of 1 or 2 were defined as having social reintegration) rate from before to after introduction of the CB [4, 5]. Although the changes were not statistically significant, all three rates increased.
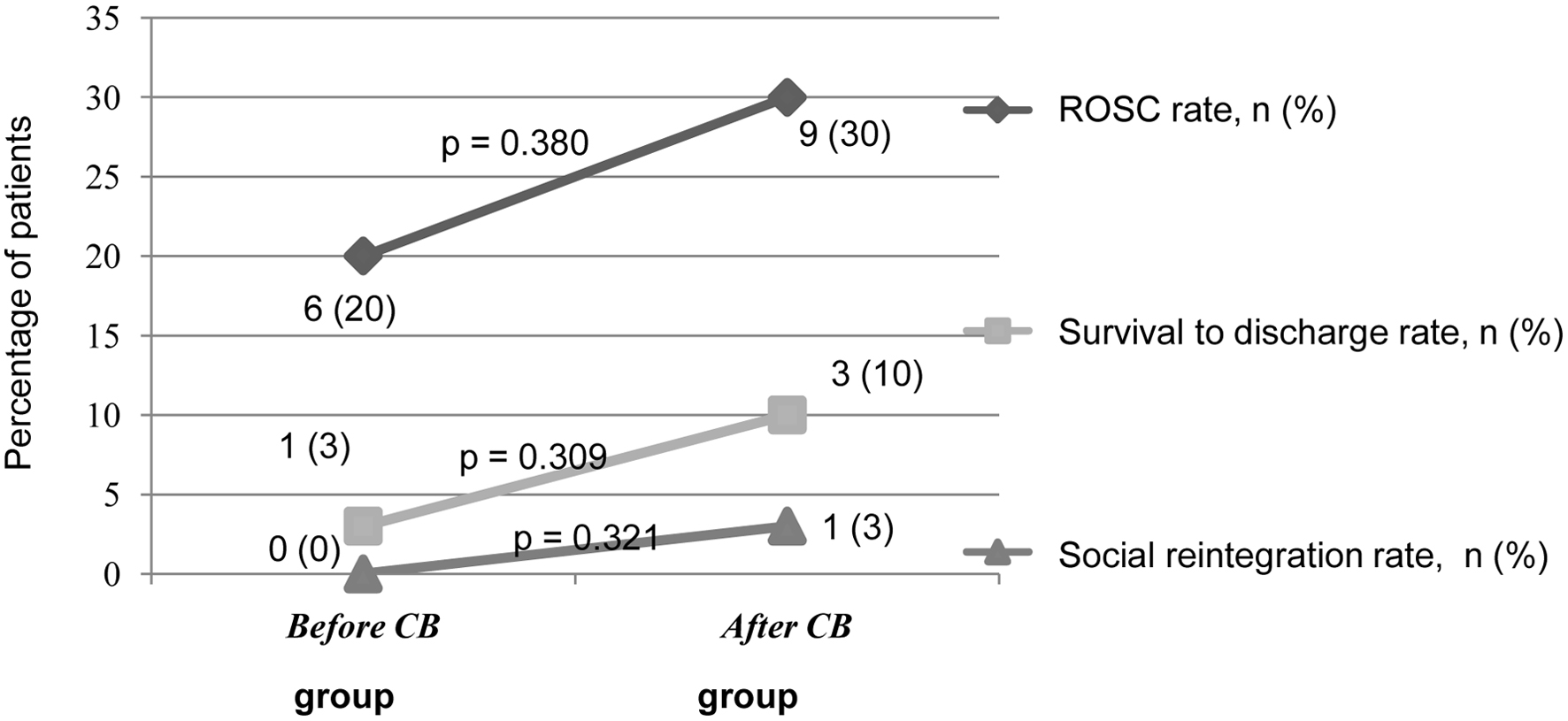 Click for large image | Figure 4. Changes in ROSC, survival to discharge, and social reintegration rates after introduction of the CB. ROSC: return of spontaneous circulation; CB: Code Blue system. |
Table 3 shows the change in the ROSC rate after introduction of the CB according to the location, pre-hospital care, cause, and electrocardiogram (ECG) findings at onset of each OHCA patient. Introduction of the CB did not lead to a change in ROSC rate according to the location of OHCA onset or whether or not pre-hospital care was provided. When analyzing the data on the cause of OHCA, the ROSC rate showed a nonsignificant increase in patients with OHCA due to cardiovascular disease. There was no significant change in ROSC rate among patients whose ECG at first contact showed asystole, pulseless electrical activity (PEA), or ventricular fibrillation (VF). However, when limited to patients whose ECG at first contact showed PEA or VF due to cardiovascular disease, the ROSC rate changed from 0% to 100% after the introduction of the CB.
 Click to view | Table 3. Changes in ROSC Rate With the Introduction of the CB According to the Patients’ Location at Onset of OHCA, the Presence or Absence of Pre-Hospital Care, the Causes, and ECG Findings |
Table 4 compares patients with and without ROSC. Factors influencing ROSC tended to include the total number of medical staff and the numbers of physicians and co-medical staff. Significantly less adrenaline was administered in patients with ROSC than in those without. An analysis of the 15 cases with ROSC showed that the amount of adrenaline administered in the ER tended to decrease after introduction of the CB (Table 5). In the analysis of the 45 cases without ROSC, the introduction of the CB tended to shorten the time from arrival at the hospital to confirmation of death (Table 6).
 Click to view | Table 4. Factors Affecting ROSC in Patients With OHCA |
 Click to view | Table 5. Comparison of Patients With OHCA and ROSC Who Were Treated Before and After the Introduction of the CB |
 Click to view | Table 6. Comparison of Patients With OHCA and Non-ROSC Who Were Treated Before and After the Introduction of the Code Blue System |
| Discussion | ▴Top |
This retrospective study on the influence of introduction of a CB revealed that the introduction of the CB significantly increased the total number of medical staff, and the number of physicians, nurses, and co-medical staff present in the ER when the emergency ambulance arrived with an OHCA patient. Although not statistically significant, it also increased the ROSC, survival to discharge, and social reintegration rates. There was no change in the time from arrival at hospital to administration of adrenaline. The amount of adrenaline used in the ER tended to decrease. Furthermore, it tended to increase the ROSC rate in patients with OHCA due to cardiac disease. Before introduction of the CB, ROSC did not occur in any of the patients with VF or PEA on ECG at first contact and cardiac disease, but after introduction of the system, all patients achieved ROSC. The factors that influenced ROSC tended to include the total number of medical staff and the number of physicians and co-medical staff. Significantly less adrenaline was administered in patients with ROSC than in those without it. In cases with ROSC, the amount of adrenaline administered tended to decrease after introduction of the CB. In cases without ROSC, the time to confirmed death tended to decrease after introduction of the CB.
The introduction of the CB enabled rapid notification of staff, reduced the time the ER chief nurse spent with communication tasks, and enabled adequate preparation and response. These changes can be expected to improve the ROSC rate because systemic management, including coronary artery assessment and temperature and circulatory management, contributes to outcomes after ROSC [6-9]. The introduction of a CB was found to improve the transition to integrated post-cardiac arrest care [9]. In the present analysis of 60 cases, although the introduction of the CB led to the presence of more staff in the ER and to an increase in ROSC, survival to discharge, and social reintegration rates, these changes were not statistically significant. However, the number of registered cases was small, so the study may have been underpowered.
Although the rate of social reintegration of OHCA patients is generally very low, the presence of a witness at the onset of cardiac arrest predicts a good outcome [10]. Favorable prognostic factors for unwitnessed cardiac arrest are younger age, ROSC during transport, chest compressions by the person who found the patient, and an indication of adaptation of electrical defibrillation on the initial ECG. If a Cerebral Performance Category of 1 or 2 at 30 days after the onset of OHCA is considered to be a good neurological prognosis [4, 5], in the present study, only one patient who was transported after bystander CPR and defibrillation with an automated external defibrillator (AED) fell into this category. However, the introduction of the CB was unlikely to be directly related to this result. Although only 17% of patients underwent bystander CPR, we found no change in ROSC rate with the introduction of the CB. The Hypothermia after Cardiac Arrest Study (HACA) study, which served as the basis for hypothermia therapy for OHCA patients, found high rates of around 50% for survival to hospital discharge and of good neurological prognosis [11]. These rates may have been the result of early withdrawal of CPR after neurological outcome assessment [12].
The geographic region covered by our facility does not have any advanced emergency medical facilities, and our hospital accepts a fairly large number of OHCA cases; however, the results of this study must be considered with the understanding that patients with VF or pulseless ventricular tachycardia and young patients tend to be transported to an emergency center approximately 10 km away that can perform extracorporeal CPR.
A secondary effect of introducing the CB was that support staff from departments other than the ER were able to regularly experience basic life support and advanced cardiac life support, which provided training in responding to emergencies within the hospital. Because nurse education progresses through stages such as noticing, interpreting, responding, and reflecting [13], education that includes hands-on experience through the CB was found to be effective. Additionally, members of the emergency ambulance staff commented that the fact that our hospital now has sufficient personnel waiting to accept OHCA patients gives them a sense of security.
The disadvantage of the CB is that when it is activated, other departments may be left with too few staff, which could disrupt normal operations. Furthermore, gathering too many staff can cause confusion, so a leader needs to take control. Another issue is that the CB is currently only used during day shifts, and during non-day shift hours, staff are still called to the ER by the traditional method. One study reported that organizing a medical emergency team in advance to respond to emergencies within a hospital is effective in reducing the number of in-hospital cardiac arrests and mortality rates [1]. It appears to be effective also for OHCA, but this approach is difficult for a medium-sized hospital like ours because establishing such a team requires a more flexible working system to ensure that a team is present at all times.
This study found no significant effect of adrenaline administration in the ambulance on the ROSC rate. Early administration of adrenaline is generally recommended in patients with non-shockable rhythms, and early administration of adrenaline to patients with OHCA before arrival at the hospital has been reported to improve life and neurological prognosis [14-16], although some studies found that it improves the ROSC rate but not neurological prognosis [17, 18]. Furthermore, a prolonged stay at the location where the OHCA occurs worsens patient prognosis [19, 20]. Ideally, a hospital is found quickly, and patients are rapidly transported there; however, it is not always possible to immediately find a hospital that will accept a patient. In any case, it is advisable that adrenaline is administered as soon as possible after the patient arrives at the hospital. In this study, introduction of the CB did not shorten the time from arrival at the hospital to administration of adrenaline, but this may have been because the time was already sufficiently short (3.3 min). However, we assume that introduction of the CB and the associated increase in available manpower allowed simultaneous securing of peripheral blood vessels and central lines for administering adrenaline. The CB may also improve early advanced airway management, which in turn may improve neurological outcome [21]; although the present study did not consider airway management, the introduction of the CB may have made endotracheal intubation smoother.
In this study, bystander CPR was performed in 17% of OHCA patients and more frequently in patients in elderly care facilities (40%) than in those where the OHCA occurred outdoors or at home (9%; P < 0.005; data not shown). There was no significant difference in ROSC rate between patients with and without bystander CPR. A smooth chain of care is necessary to save the life of someone experiencing OHCA [20], and as the first step, bystander CPR is crucial. This study found that although bystander CPR was performed more frequently in elderly care facilities than in the outdoors or at home, the rate was not high enough in view of the fact that such facilities have paramedical staff. The reason for this may be that these facilities house elderly people with chronic diseases, so staff members have insufficient awareness of and ability to respond to OHCA. In addition, the age of the OHCA patients at the facilities (89.7 ± 6.5) was higher than that of patients who experienced OHCA outdoors or at home (76.9 ± 11.0), and staff at the facilities may have been hesitant to resuscitate patients (data not shown). However, elderly care facilities generally do not have a system such as a rapid response system [2] for treating patients whose condition suddenly worsens. In fact, current policies for dealing with sudden changes in patients’ conditions are often not widely known and are unclear within elderly care facilities.
The survival rate of OHCA patients is high when the public has access to an AED [22], and it has improved with the widespread use of AED [23]. Furthermore, verbal instructions from telecommunicator CPR were found to be an effective means of increasing the rate of bystander CPR [24]. In addition to providing resuscitation training to the general public, there is a need to increase opportunities for self-learning [25], focus on early recognition of OHCA [26], and provide training in chest compression-only CPR [27].
The analysis of cases without ROSC found that introduction of the CB tended to shorten the time from arrival at the hospital to confirmation of death. We considered that introduction of the CB enabled the decision to terminate resuscitation to be made more quickly, since more physicians and staff members were present and able discuss the situation. In OHCA cases, conditions such as the absence of witnesses, no indication for defibrillation on the initial ECG, defibrillation not being performed, and absence of ROSC before arrival at the hospital were reported to indicate a very poor prognosis and require consideration of termination of resuscitation [28-32].
Unfortunately, most of the OHCA patients enrolled in this study fell into one of the categories in which termination of resuscitation is recommended. Therefore, the data may indicate that there is no point in improving OHCA response after patients arrive at the hospital, as was done with the introduction of the CB. However, we believe that introduction of the CB may improve the chance, although rare, that some patients will be able to return to society. Achieving ROSC also gives the patient’s family time to accept the patient’s condition. Unfortunately, the vast majority of OHCA patients die, but providing adequate medical care promptly at the end of life may alleviate the family’s regret. Furthermore, it is important to note that the hospital staff improved their ability to respond to sudden changes in the condition of patients. The consequences of improving a CB and striving for ROSC need to be comprehensively evaluated across the entire medical system.
Conclusions
There is surprisingly little literature on the preparation of hospitals to accept OHCA cases. Most OHCA patients are transported to emergency medical centers that have ample staff, so even if medium-sized hospitals have implemented various measures, these may not be reported in the literature. Although not statistically significant, the introduction of the CB increased the ROSC rate and resulted in some patients surviving to hospital discharge. The introduction of the CB was expected to improve the quality of medical care by convening medical staff more quickly and allowing multiple professions to perform their predefined tasks within the scope of their expertise. We plan to continue to work on improving the CB at our hospital and to provide high-quality emergency medical care to the local community.
Study limitations
This study has some limitations. It was a retrospective study and performed at a single center. Furthermore, the number of enrolled cases was small, so that study may have been underpowered. Initially, although we felt that the introduction of CB had significantly improved the ROSC rate, the ROSC rate had not changed significantly when we actually performed statistical analysis. Therefore, the expected sample size was calculated to be small. Also, the prescribed study period could not be extended. Since our CB system was defined as being activated in OHCA patients including those with ROSC after cardiac arrest and those with post-resuscitation shock, we suggested that including cases who had already achieved ROSC in this study would be biased.
Acknowledgments
We would like to thank the medical staff at our hospital.
Financial Disclosure
The authors have no financial disclosure or funding conflicts of interest directly relevant to the content of this article.
Conflict of Interest
The authors have no conflict of interest directly relevant to the content of this article.
Informed Consent
Because the study retrospectively collected information from medical records, informed consent was not required.
Author Contributions
Youichi Inoue: study design, data collection, data interpretation, manuscript preparation, and literature search. Keisuke Okamura: study design, data collection, statistical analysis, data interpretation, manuscript preparation, and literature search. Hideaki Shimada, Osamu Imakyure: study design. Shinobu Watakabe, Shiori Hirayama, Machiko Hirata, Ayaka Kusuda, Arisa Matsumoto, Miki Inoue, Emi Matsuishi, Mizuki Yamada: study design, data collection, and data interpretation. Sachiko Iwanaga, Shogo Narumi, Shiki Nakayama, Hideto Sako, Akihiro Udo, Kenichiro Taniguchi, Shogo Morisaki, Souichiro Ide, Yasuyuki Nomoto, Shin-ichiro Miura, Ichiro Imamura: data interpretation.
Data Availability
Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.
| References | ▴Top |
- Buist MD, Moore GE, Bernard SA, Waxman BP, Anderson JN, Nguyen TV. Effects of a medical emergency team on reduction of incidence of and mortality from unexpected cardiac arrests in hospital: preliminary study. BMJ. 2002;324(7334):387-390.
doi pubmed - Hongo T, Naito H, Fujiwara T, Naito T, Homma Y, Fujimoto Y, Takaya M, et al. Prevalence and predictors of direct discharge home following hospitalization of patients with serious adverse events managed by the rapid response system in Japan: a multicenter, retrospective, observational study. Acute Med Surg. 2021;8(1):e690.
doi pubmed - Kanda Y. Investigation of the freely available easy-to-use software 'EZR' for medical statistics. Bone Marrow Transplant. 2013;48(3):452-458.
doi pubmed - A randomized clinical study of cardiopulmonary-cerebral resuscitation: design, methods, and patient characteristics. Brain Resuscitation Clinical Trial I Study Group. Am J Emerg Med. 1986;4(1):72-86.
pubmed - Ajam K, Gold LS, Beck SS, Damon S, Phelps R, Rea TD. Reliability of the Cerebral Performance Category to classify neurological status among survivors of ventricular fibrillation arrest: a cohort study. Scand J Trauma Resusc Emerg Med. 2011;19:38.
doi pubmed - Nielsen N, Wetterslev J, Cronberg T, Erlinge D, Gasche Y, Hassager C, Horn J, et al. Targeted temperature management at 33 degrees C versus 36 degrees C after cardiac arrest. N Engl J Med. 2013;369(23):2197-2206.
doi pubmed - Strote JA, Maynard C, Olsufka M, Nichol G, Copass MK, Cobb LA, Kim F. Comparison of role of early (less than six hours) to later (more than six hours) or no cardiac catheterization after resuscitation from out-of-hospital cardiac arrest. Am J Cardiol. 2012;109(4):451-454.
doi pubmed - Callaway CW, Donnino MW, Fink EL, Geocadin RG, Golan E, Kern KB, Leary M, et al. Part 8: post-cardiac arrest care: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18 Suppl 2):S465-482.
doi pubmed - Peberdy MA, Callaway CW, Neumar RW, Geocadin RG, Zimmerman JL, Donnino M, Gabrielli A, et al. Part 9: post-cardiac arrest care: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122(18 Suppl 3):S768-786.
doi pubmed - Nishikimi M, Ogura T, Nishida K, Takahashi K, Nakamura M, Matsui S, Matsuda N, et al. External validation of a risk classification at the emergency department of post-cardiac arrest syndrome patients undergoing targeted temperature management. Resuscitation. 2019;140:135-141.
doi pubmed - Hypothermia after Cardiac Arrest Study Group. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002;346(8):549-556.
doi pubmed - Hsu CH, Li J, Cinousis MJ, Sheak KR, Gaieski DF, Abella BS, Leary M. Cerebral performance category at hospital discharge predicts long-term survival of cardiac arrest survivors receiving targeted temperature management*. Crit Care Med. 2014;42(12):2575-2581.
doi pubmed - Tanner CA. Thinking like a nurse: a research-based model of clinical judgment in nursing. J Nurs Educ. 2006;45(6):204-211.
doi pubmed - Ueta H, Tanaka H, Tanaka S, Sagisaka R, Takyu H. Quick epinephrine administration induces favorable neurological outcomes in out-of-hospital cardiac arrest patients. Am J Emerg Med. 2017;35(5):676-680.
doi pubmed - Ran L, Liu J, Tanaka H, Hubble MW, Hiroshi T, Huang W. Early administration of adrenaline for out-of-hospital cardiac arrest: a systematic review and meta-analysis. J Am Heart Assoc. 2020;9(11):e014330.
doi pubmed - Hansen M, Schmicker RH, Newgard CD, Grunau B, Scheuermeyer F, Cheskes S, Vithalani V, et al. Time to epinephrine administration and survival from nonshockable out-of-hospital cardiac arrest among children and adults. Circulation. 2018;137(19):2032-2040.
doi pubmed - Loomba RS, Nijhawan K, Aggarwal S, Arora RR. Increased return of spontaneous circulation at the expense of neurologic outcomes: Is prehospital epinephrine for out-of-hospital cardiac arrest really worth it? J Crit Care. 2015;30(6):1376-1381.
doi pubmed - Perkins GD, Ji C, Deakin CD, Quinn T, Nolan JP, Scomparin C, Regan S, et al. A randomized trial of epinephrine in out-of-hospital cardiac arrest. N Engl J Med. 2018;379(8):711-721.
doi pubmed - Shin SD, Kitamura T, Hwang SS, Kajino K, Song KJ, Ro YS, Nishiuchi T, et al. Association between resuscitation time interval at the scene and neurological outcome after out-of-hospital cardiac arrest in two Asian cities. Resuscitation. 2014;85(2):203-210.
doi pubmed - Iwami T, Nichol G, Hiraide A, Hayashi Y, Nishiuchi T, Kajino K, Morita H, et al. Continuous improvements in "chain of survival" increased survival after out-of-hospital cardiac arrests: a large-scale population-based study. Circulation. 2009;119(5):728-734.
doi pubmed - Nakagawa K, Sagisaka R, Morioka D, Tanaka S, Takyu H, Tanaka H. The association of delayed advanced airway management and neurological outcome after out-of-hospital cardiac arrest in Japan. Am J Emerg Med. 2022;62:89-95.
doi pubmed - White RD, Bunch TJ, Hankins DG. Evolution of a community-wide early defibrillation programme experience over 13 years using police/fire personnel and paramedics as responders. Resuscitation. 2005;65(3):279-283.
doi pubmed - Kitamura T, Kiyohara K, Sakai T, Matsuyama T, Hatakeyama T, Shimamoto T, Izawa J, et al. Public-access defibrillation and out-of-hospital cardiac arrest in Japan. N Engl J Med. 2016;375(17):1649-1659.
doi pubmed - Vaillancourt C, Verma A, Trickett J, Crete D, Beaudoin T, Nesbitt L, Wells GA, et al. Evaluating the effectiveness of dispatch-assisted cardiopulmonary resuscitation instructions. Acad Emerg Med. 2007;14(10):877-883.
doi pubmed - Lynch B, Einspruch EL. With or without an instructor, brief exposure to CPR training produces significant attitude change. Resuscitation. 2010;81(5):568-575.
doi pubmed - Bobrow BJ, Zuercher M, Ewy GA, Clark L, Chikani V, Donahue D, Sanders AB, et al. Gasping during cardiac arrest in humans is frequent and associated with improved survival. Circulation. 2008;118(24):2550-2554.
doi pubmed - Bohm K, Rosenqvist M, Herlitz J, Hollenberg J, Svensson L. Survival is similar after standard treatment and chest compression only in out-of-hospital bystander cardiopulmonary resuscitation. Circulation. 2007;116(25):2908-2912.
doi pubmed - Goto Y, Funada A, Goto Y. Relationship between the duration of cardiopulmonary resuscitation and favorable neurological outcomes after out-of-hospital cardiac arrest: a prospective, nationwide, population-based cohort study. J Am Heart Assoc. 2016;5(3):e002819.
doi pubmed - Goto Y, Maeda T, Goto YN. Termination-of-resuscitation rule for emergency department physicians treating out-of-hospital cardiac arrest patients: an observational cohort study. Crit Care. 2013;17(5):R235.
doi pubmed - Morrison LJ, Verbeek PR, Zhan C, Kiss A, Allan KS. Validation of a universal prehospital termination of resuscitation clinical prediction rule for advanced and basic life support providers. Resuscitation. 2009;80(3):324-328.
doi pubmed - Bailey ED, Wydro GC, Cone DC. Termination of resuscitation in the prehospital setting for adult patients suffering nontraumatic cardiac arrest. National Association of EMS Physicians Standards and Clinical Practice Committee. Prehosp Emerg Care. 2000;4(2):190-195.
doi pubmed - Hauk L. AHA Updates guidelines for CPR and emergency cardiovascular care. Am Fam Physician. 2016;93(9):791-797.
pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.