| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://jocmr.elmerjournals.com |
Original Article
Volume 17, Number 4, April 2025, pages 200-207
Evaluating Postural Sway in the Elderly Using Inertial Measurement Units: A Study on Center of Mass Measurements via Accelerometers and Gyroscopes
Siriphan Kongsawasdia , Pummarirat Bunjana, Molthicha Wongjaka, Witchayaphorn Saenmuenga, Kittichai Wantanajittikulb, c
aDepartment of Physical Therapy, Faculty of Associated Medical Sciences, Chiang Mai University, Chiang Mai, Thailand
bDepartment of Radiologic Technology, Faculty of Associated Medical Sciences, Chiang Mai University, Chiang Mai, Thailand
cCorresponding Author: Kittichai Wantanajittikul, Department of Radiologic Technology, Faculty of Associated Medical Sciences, Chiang Mai University, Chiang Mai, Thailand
Manuscript submitted January 12, 2025, accepted March 24, 2025, published online April 11, 2025
Short title: IMU Evaluation of Elderly Postural Sway
doi: https://doi.org/10.14740/jocmr6184
| Abstract | ▴Top |
Background: Assessment of center of mass (COM) changes during static stance control has practical implications in clinical settings, notably among older adults. Recently portable and wearable devices, including accelerometers and gyroscopes, have emerged as a promising alternative to traditional clinical and laboratory assessments. The objectives of the study were to evaluate COM postural sway parameters derived from accelerometer and gyroscope data during static balance tasks with varying bases of support in healthy elderly individuals, and to examine the correlation and agreement between accelerometer-based and gyroscope-based parameters in postural sway assessment.
Methods: One hundred and fourteen healthy elderly individuals who had not experienced falls within the preceding 6 months and were confirmed to have no risk of falling as determined by the timed up and go test, were included in this study. They were evaluated for postural sway while standing, using the sensor securely with a belt attached to the L5 vertebra. The four-stage balance test, including standing in a double stance (SO), semi-tandem stance (STO), tandem stance (TO), and single-leg stance (SL), was employed to assess each participant’s ability to maintain balance under increasingly challenging standing positions on a stable surface.
Results: The study demonstrated that COM posture sway increased with a demanding position and a decreasing base of support. Spearman’s rho correlation coefficients from the anteroposterior and mediolateral planes exhibited strong correlation (0.75 - 0.9). Moderate reliability was observed for both the accelerometer and gyroscope parameters in both planes (intraclass correlation coefficient: 0.5 and 0.75).
Conclusions: Accelerometry and gyroscopes provide objective quantification of balance that have the potential to be utilized in conjunction with clinical tests to effectively evaluate the risk of falling.
Keywords: Inertial measurement unit; Accelerometer; Gyroscope; Center of mass; Falls
| Introduction | ▴Top |
Balance impairment among older adults represents a major public health challenge, with falls leading to severe outcomes including fractures, mobility loss, and reduced independence [1, 2]. Approximately one-third of adults aged 65 and older fall each year, making early detection of balance deficits crucial for fall prevention [3]. Balance assessment methods range from clinical tools to laboratory-based equipment. Clinical tools included the Berg balance scale [4], timed up and go (TUG) test [5], functional reach test [6] and Tinetti test [7]. While these tests are relatively expeditious, reliable, and offer potentially valuable information on fall risk, they are dependent on subjective evaluations by assessors. This subjectivity can compromise their precision and reliability, and they appear to lack the capacity to differentiate effectively among relatively healthy populations [8]. In contrast, posturographic measures by laboratory equipment such as motion capture systems and force platform provide gold-standard measurements of center of mass (COM) and center of pressure (COP) for balance evaluation. Although these systems offer superior accuracy, their implementation in clinical settings is often constrained due to their high costs and the requirement for specialized spaces [9]. Since 2002, inertial measurement units (IMUs) have emerged as promising low-cost alternatives for objective human movement assessment [8, 10-13]. Body-worn inertial sensors, which include accelerometers and gyroscopes, possess the potential to enhance balance assessments in ambulatory care settings. These devices expand the range of balance control parameters that can be evaluated and enable a more comprehensive analysis; however, they have unique capabilities [14]. Accelerometers, now ubiquitous in smart devices such as mobile phones, watches, and tablets, show potential for clinical balance assessment applications [15]. These sensors measure three-dimensional linear acceleration (x, y, and z) to capture COM displacements during daily activities, enabling evaluation of both static and dynamic balance through sway patterns and stability during standing tasks [16-18]. Previous studies have demonstrated significant correlations between accelerometer-derived measures and force plate COP data in balance assessment [19-22]. However, accelerometer measurements can be affected by external vibrations and movements, potentially compromising accuracy of balance evaluations [16]. The gravity component detected by a non-horizontal measuring axis appears to be one evident cause of variability [18]. Gyroscopes measure the rate of rotation around an axis, providing critical information about body orientation and movement dynamics, although, less frequently utilized and more complex to analyze, requiring integration over time to derive angles and positions, they provide valuable insights into capturing balance control [13, 23]. Therefore, the aims of this study were to evaluate COM postural sway parameters derived from accelerometer and gyroscope data during static balance tasks with varying bases of support (BOS) in healthy elderly individuals, and to examine the correlation and agreement between accelerometer-based and gyroscope-based parameters in postural sway assessment.
| Materials and Methods | ▴Top |
Participants
One hundred and fourteen healthy individuals aged over 60 years were included, comprising 56 females and 58 males. The participants had mean values for age, weight, height, and body mass index: 65.90 years, 57.4 kg, 158.8 cm, and 22.8 kg/m2, respectively. They were initially selected and screened by healthcare providers at the local health-promoting hospital prior to study enrollment. Eligibility criteria required the absence of neurological or musculoskeletal conditions and cognitive impairments, as well as the ability to independently perform professional or routine activities and exhibit good social interaction, indicative of normal mental health and behavior. To ensure participants demonstrated adequate balance control, they were required to achieve a score of less than 4 points on the Thai falls risk assessment test (Thai-FRAT) [24] and complete the TUG test in under 13.5 s [25]. Participants were excluded from this study if they had severe vision impairments, a history of falling more than twice within the previous 6 months, or any chronic illnesses or conditions that might affect their balance. The Ethics Committee of the Faculty of Associated Medical Sciences at Chiang Mai University approved all procedures (study code AMSEC-66EX-088; 2023). The study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
Protocol and process of data
Participants were evaluated for postural sway while standing, with the sensor securely with belt attached to the L5 vertebra in the lower back, near the COM of the human body [26, 27]. The four-stage balance test was employed to assess each participant’s ability to maintain balance under increasingly challenging standing positions on a stable surface. These positions included standing in a double stance (SO), semi-tandem stance (STO), tandem stance (TO), and single-leg stance (SL) (Fig. 1). For each test, participants were instructed to stand on the ground for 20 consecutive seconds, with resting periods of 1 - 2 min or until they returned to a stable state. Clear instructions were provided, directing participants to maintain a forward gaze throughout the trials. If a participant was unable to complete a 20-s trial, the minimum required duration was reduced to 15 s. The experimental procedure is illustrated in Figure 1.
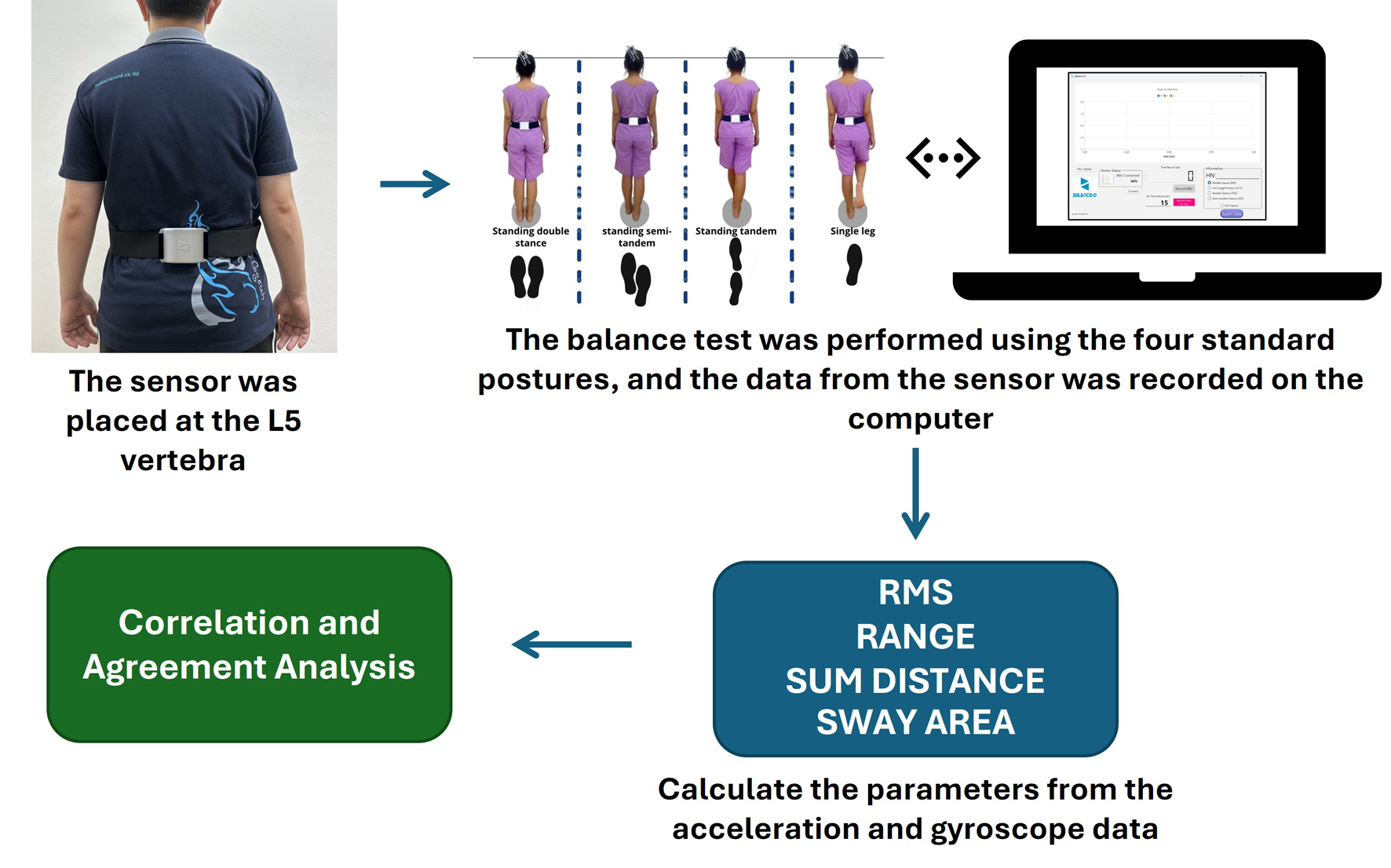 Click for large image | Figure 1. The diagram for the experimental procedure. |
Instrument
We developed the prototype of customized triaxial inertial sensor of: 1) a 3-Space Sensor™ Nano; 2) an ESP8266 Node MCU Wi-Fi; and 3) a 3 V, 2,000 mAh lithium polymer battery with a charging module. The data were filtered using a third-order high-pass Butterworth filter with a 50 Hz sampling rate to reduce the influence of high-frequency noise and transmitted to a personal computer (PC) through the use of Wi-Fi. A customized MATLAB script was utilized to compute the postural sway measures that were obtained from the IMUs (Mathworks Inc., Natick, MA). Overall, the accelerometers and gyroscopes provide accurate information for estimate motion.
Postural sway metrics
The evaluation of accelerometer- and gyroscope-derived outcome measures involved calculating specific parameters for each axis (x, y, and z) and representing them in the anteroposterior (AP) and mediolateral (ML) planes. The balance parameters of interest were derived as time-domain features which were commonly used in the literature to quantify postural stability including the root mean square of magnitude (RMS), calculated as the square root of average of the squared values of accelerations; range of magnitude (RANGE), defined as the range of acceleration signals; sway area (SA), representing the area covered by the acceleration signals normalized to the duration of the measurement; and summation of distance (SD), defined as the total distance from the center of the acceleration trajectory, also normalized to the duration of the measurement [11, 26]. These four parameters were systematically computed and analyzed, providing a comprehensive basis for comparison between accelerometer and gyroscope outcomes. All signal processing, feature extraction, and analyses were performed using MATLAB version 2021a (The Mathworks Inc., Natick, MA, USA).
Statistical analysis
Descriptive statistics were conducted to describe the COM postural sway values from the IMU. In order to quantify the correlation between the accelerometer and gyroscope data obtained from the IMU, Spearman’s correlation was utilized since the data from the IMU did not conform to the normal distribution criterion. Intraclass correlation coefficients (ICC2,1), two-way mixed-effects model, and 95% confidence intervals were conducted to evaluate agreement between sway metrics from the accelerometer and gyroscope [28].
| Results | ▴Top |
A total of 114 healthy elderly participants, aged 60 to 86 years, were included in the study, as shown in Table 1.
 Click to view | Table 1. Demographic and Clinical Data |
The average values of the accelerometer-derived metrics for all four positions, as measured by RMS, RANGE, SA, and SD, are presented in Table 2 and presented as bar graphs in Figure 2. These values showed an ascending order of magnitude as the BOS decreased, in both the AP and ML planes, across the following positions: SO, STO, TO, and SL.
 Click to view | Table 2. AP and ML Planes of Accelerometer-Derived Sway Metrics for Each Test Condition |
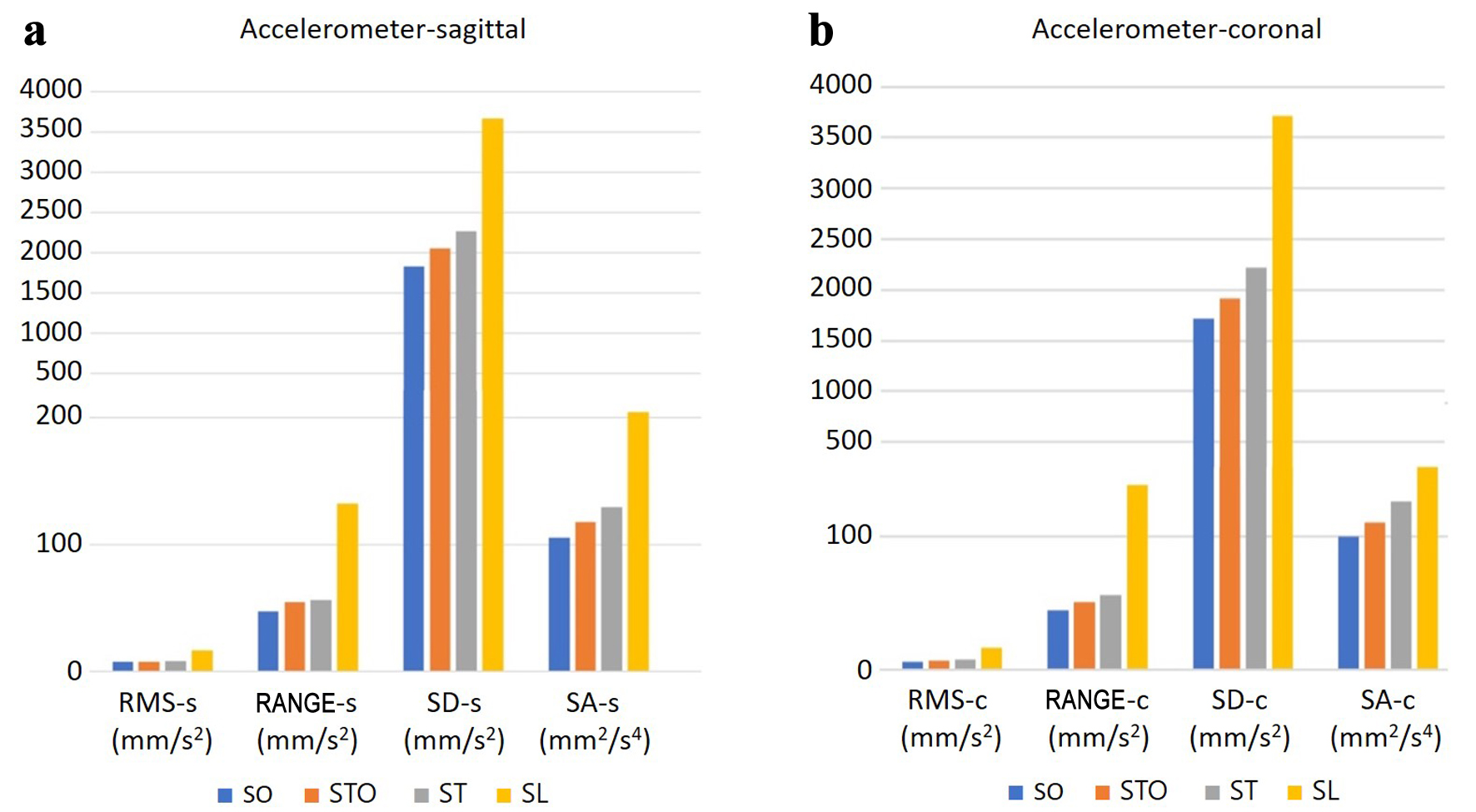 Click for large image | Figure 2. Bar graph depicting COM postural sway in accelerometer (RMS, RANGE, SA, and SD) ranging from a variety of increasingly challenging conditions of base of support in (a) AP and (b) ML planes. COM: center of mass; RMS: root mean square of magnitude; RANGE: summation of the range of signals; SA: sway area; SD: summation of distance; AP: anteroposterior; ML: mediolateral. |
Similarly, the gyroscope-derived metrics for all four positions, using the RMS, RANGE, SA, and SD variables, are detailed in Table 3 and presented as bar graphs in Figure 3.
 Click to view | Table 3. AP and ML Planes of Gyroscope-Derived Sway Metrics for Each Test Condition |
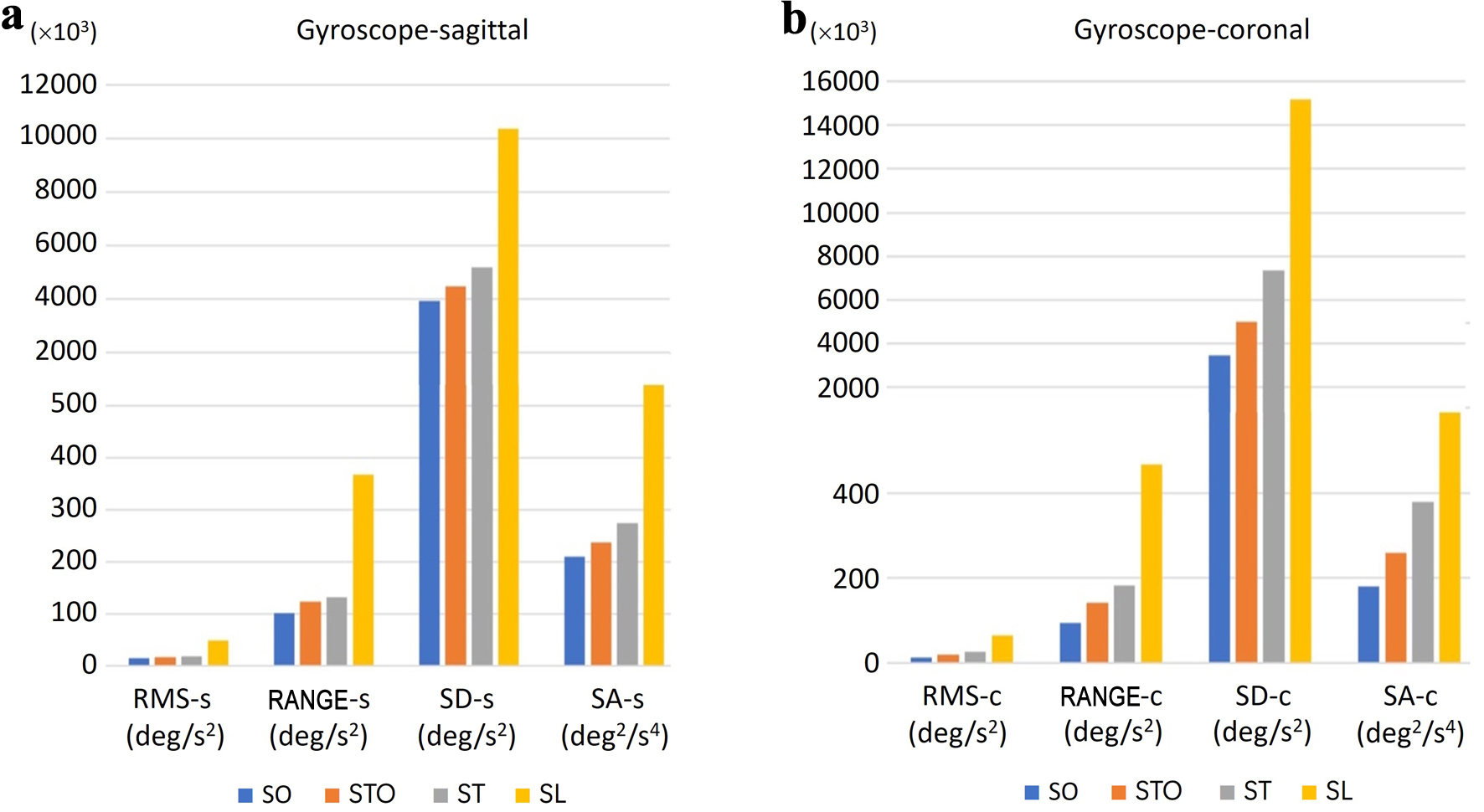 Click for large image | Figure 3. Bar graph depicted COM postural sway in gyroscope (RMS, RANGE, SA, and SD) ranging from a variety of increasingly challenging conditions of base of support in (a) AP and (b) ML planes. COM: center of mass; RMS: root mean square of magnitude; RANGE: summation of the range of signals; SA: sway area; SD: summation of distance; AP: anteroposterior; ML: mediolateral. |
The correlation between sway metrics from the accelerometer and gyroscope was evaluated, as shown in Table 4. The results indicated a strong correlation between the gyroscope and accelerometer sway metrics. Spearman’s rho correlation coefficients for both the AP and ML planes demonstrated a good correlation, with values ranging from 0.75 to 0.90.
 Click to view | Table 4. Spearmen’s Rho Correlation Coefficient of Accelerometer Compared With Gyroscope Derived From Inertial Measurement Unit |
The ICC was then calculated to assess the agreement between sway metrics from the accelerometer and gyroscope. The parameters evaluated included the RMS, RANGE, SA, and SD. Results showed that all parameters from both the accelerometer and gyroscope demonstrated moderate reliability, with ICC values ranging from 0.50 to 0.70 in both AP and ML planes (Table 5).
 Click to view | Table 5. ICC of Accelerometer Compared With Gyroscope Derived From Inertial Measurement Unit |
| Discussion | ▴Top |
Falls are a primary concern for older adults, requiring objective evaluation of balance and postural control to provide reliable measures of an individual’s ability to maintain stability. Wearable sensors, characterized by their portability, can be utilized in diverse environments and offer enhanced sensitivity and objectivity in detecting balance impairments compared to traditional methods such as clinical assessments or gold standard tools, which are often costly and immobile. Recognizing the unique potential of these sensors to gather data on balance and postural control, a triaxial IMU with a 50 Hz sampling rate was developed to measure the COM postural sway in healthy elderly individuals across different BOS, with a particular focus on comparing accelerometer and gyroscope data. The study evaluated participants’ ability to maintain balance with open eyes in four progressively difficult standing positions on a stable surface. We analyzed sensor-derived parameters, including RMS, RANGE, SA, and SD in both AP and ML planes. The magnitude of acceleration and gyroscope measurements demonstrated increased postural sway as the BOS progressively decreased from SO to STO, TO, and SL positions. Both devices showed sufficient sensitivity to detect balance adjustments during increasingly challenging conditions. These findings align with previous researches and the fundamental principle of postural control, where maintaining stability becomes more demanding as the BOS decreases, requiring enhanced neuromuscular control to keep the COM within the limits of support [17, 29-31].
The correlation between accelerometers and gyroscopes reveals a strong relationship in the parameter values obtained from both sensors. This study found that all parameters exhibited good correlation coefficient values (values between 0.75 and 0.90 indicate good reliability). The highest correlation coefficient values were obtained with RMS-ML (r = 0.86). This result was consistent with the previous study that RMS of acceleration increased as the complexity of the tasks increased. RMS is commonly employed to measure postural sway and has been demonstrated to be responsive to alterations in balance function values [32]. It also significantly differentiated between various test conditions and establishes criterion validity [31, 32].
This study utilized the ICC to investigate the agreement between the accelerometer and gyroscope. The results revealed that all parameters exhibited moderate agreement (ICC: 0.58 and 0.71) between the accelerometer and the gyroscope across both planes. This moderate reliability indicates that, although there is consistency between the measurements, some variability persists. This level of agreement may be attributed to the intrinsic differences in the measurement properties of each sensor. Accelerometers measure linear acceleration and are particularly sensitive to gravitational forces, whereas gyroscopes measure angular velocity and rotational movements, potentially exhibiting greater sensitivity to rotational adjustments used to maintain balance [13, 17, 23]. The moderate agreement underscores the utility of the measurement approach while acknowledging the challenges of achieving perfect reproducibility in assessments such as dynamic movement. This degree of reliability is adequate for group-level analyses and clinical applications, although individual measurements should be interpreted with appropriate caution. Recent studies support the combination of gyroscopes with accelerometers with the advantage that both linear and angular motions are recorded, reducing calibration biases [33]. Consequently, this may enhance the accuracy of balance and movement assessment for fall-risk detection. The moderate ICC suggests that employing both sensors might provide a more comprehensive representation of an individual’s balance control mechanisms. This approach could be particularly relevant when assessing complex balance tasks or when detailed analysis of balance strategies is required [10, 34-36].
To summarize, wearable sensors offer various advantages, including continuous data obtaining, portability, higher sensitivity, and cost-effectiveness. Even though IMUs cannot completely replace force platforms for research-level precision, they provide a cost-effective and portable alternative, necessitate minimal training, and allow for tests in a variety of clinical and community settings. Evaluation of COM trajectory metrics could be integrated into comprehensive geriatric assessments. By quantifying subtle COM deviations undetectable via observation, IMUs could enhance early identification of high-risk elderly, enabling timely referral for multifactorial interventions, e.g., strength training, home modifications. The study demonstrated the efficacy of the developed IMU prototype in evaluating postural sway among healthy elderly individuals. All sensor-derived parameters exhibited a strong correlation between the accelerometer and gyroscope in both the AP and ML planes, indicating a relationship between the two devices. However, they demonstrated moderate agreement, thus highlighting significant considerations regarding sensor selection and data interpretation. Future research should focus on enhancing the performance of the IMU by integrating time-synchronized accelerometer and gyroscope signals to improve the precision of sway metrics. This approach is supported by recent studies [33], indicating that sensor fusion algorithms, such as Kalman filters or machine learning models like random forest, can effectively integrate these signals to enhance sway metric precision. The study provides valuable insights into the application of IMU technology for postural sway assessment in healthy elderly individuals. However, some limitations warrant consideration. Although the study aimed to incorporate healthy older participants, it is concerning that factors such as lifestyle and comorbidities may influence the test findings. Further investigation into the performance of IMU prototype in populations with varying levels of fall risk should be conducted.
Acknowledgments
The authors gratefully acknowledge the elderly volunteers who participated in this study.
Financial Disclosure
This work was funded by the Faculty of Associated Medical Sciences, Chiang Mai University, Thailand.
Conflict of Interest
None to declare.
Informed Consent
The participants read and completed written informed consent prior to participating.
Author Contributions
Conceptualization: SK and KW; development of prototype and software: KW; data collection: SK, PB, MW, and WS; data analysis: SK, PB, MW, and WS; writing the article: SK, PB, MW, WS, and KW. All authors have read and agreed to the published version of the manuscript.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
AP: anteroposterior; BMI: body mass index; BOS: base of support; COM: center of mass; COP: center of pressure; ML: mediolateral; RMS: root mean square of magnitude; SA: sway area; SD: summation of distance; SL: single-leg stance; SO: standing in a double stance; STO: semi-tandem stance; Thai-FRAT: Thai falls risk assessment test; TO: tandem stance; TUG: timed up and go
| References | ▴Top |
- Nnodim JO, Yung RL. Balance and its clinical assessment in older adults - a review. J Geriatr Med Gerontol. 2015;1(1):003.
doi pubmed - Horak FB. Clinical measurement of postural control in adults. Phys Ther. 1987;67(12):1881-1885.
doi pubmed - James SL, Lucchesi LR, Bisignano C, Castle CD, Dingels ZV, Fox JT, Hamilton EB, et al. The global burden of falls: global, regional and national estimates of morbidity and mortality from the Global Burden of Disease Study 2017. Inj Prev. 2020;26(Supp 1):i3-i11.
doi pubmed - Bogle Thorbahn LD, Newton RA. Use of the berg balance test to predict falls in elderly persons. Phys Ther. 1996;76(6):576-583; discussion 584-575.
doi pubmed - Podsiadlo D, Richardson S. The timed "Up & Go": a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142-148.
doi pubmed - Duncan PW, Weiner DK, Chandler J, Studenski S. Functional reach: a new clinical measure of balance. J Gerontol. 1990;45(6):M192-197.
doi pubmed - Omana H, Bezaire K, Brady K, Davies J, Louwagie N, Power S, Santin S, et al. Functional reach test, single-leg stance test, and Tinetti performance-oriented mobility assessment for the prediction of falls in older adults: a systematic review. Phys Ther. 2021;101(10):pzab173.
doi pubmed - Patel M, Pavic A, Goodwin VA. Wearable inertial sensors to measure gait and posture characteristic differences in older adult fallers and non-fallers: A scoping review. Gait Posture. 2020;76:110-121.
doi pubmed - Noamani A, Riahi N, Vette AH, Rouhani H. Clinical static balance assessment: a narrative review of traditional and IMU-based posturography in older adults and individuals with incomplete spinal cord injury. Sensors (Basel). 2023;23(21):8881.
doi pubmed - Sipp AR, Rowley BA. Alternative devices for the quantification of human motion. Crit Rev Biomed Eng. 2007;35(5):413-442.
doi pubmed - McManus K, Greene BR, Ader LGM, Caulfield B. Development of data-driven metrics for balance impairment and fall risk assessment in older adults. IEEE Trans Biomed Eng. 2022;69(7):2324-2332.
doi pubmed - O'Brien MK, Hidalgo-Araya MD, Mummidisetty CK, Vallery H, Ghaffari R, Rogers JA, Lieber R, et al. Augmenting clinical outcome measures of gait and balance with a single inertial sensor in age-ranged healthy adults. Sensors (Basel). 2019;19(20):4537.
doi pubmed - Mayagoitia RE, Nene AV, Veltink PH. Accelerometer and rate gyroscope measurement of kinematics: an inexpensive alternative to optical motion analysis systems. J Biomech. 2002;35(4):537-542.
doi pubmed - Culhane KM, O'Connor M, Lyons D, Lyons GM. Accelerometers in rehabilitation medicine for older adults. Age Ageing. 2005;34(6):556-560.
doi pubmed - Bohlke K, Redfern MS, Rosso AL, Sejdic E. Accelerometry applications and methods to assess standing balance in older adults and mobility-limited patient populations: a narrative review. Aging Clin Exp Res. 2023;35(10):1991-2007.
doi pubmed - Leiros-Rodriguez R, Garcia-Soidan JL, Romo-Perez V. Analyzing the use of accelerometers as a method of early diagnosis of alterations in balance in elderly people: a systematic review. Sensors (Basel). 2019;19(18):3883.
doi pubmed - Heebner NR, Akins JS, Lephart SM, Sell TC. Reliability and validity of an accelerometry based measure of static and dynamic postural stability in healthy and active individuals. Gait Posture. 2015;41(2):535-539.
doi pubmed - Moe-Nilssen R, Helbostad JL. Trunk accelerometry as a measure of balance control during quiet standing. Gait Posture. 2002;16(1):60-68.
doi pubmed - Noamani A, Nazarahari M, Lewicke J, Vette AH, Rouhani H. Validity of using wearable inertial sensors for assessing the dynamics of standing balance. Med Eng Phys. 2020;77:53-59.
doi pubmed - Noonan M, Axelrod S. The stability and interest consonance of lateral postural—motor biases in rats: results and implications. Behav Neural Biol. 1989;52(3):386-405.
doi pubmed - Richmond SB, Fling BW, Lee H, Peterson DS. The assessment of center of mass and center of pressure during quiet stance: Current applications and future directions. J Biomech. 2021;123:110485.
doi pubmed - Whitney SL, Roche JL, Marchetti GF, Lin CC, Steed DP, Furman GR, Musolino MC, et al. A comparison of accelerometry and center of pressure measures during computerized dynamic posturography: a measure of balance. Gait Posture. 2011;33(4):594-599.
doi pubmed - Allum JH, Carpenter MG. A speedy solution for balance and gait analysis: angular velocity measured at the centre of body mass. Curr Opin Neurol. 2005;18(1):15-21.
doi pubmed - Thiamwong L, Thamarpirat J, Maneesriwongul W, Jitapunkul S. Thai falls risk assessment test (Thai-FRAT) developed for community-dwelling Thai elderly. J Med Assoc Thai. 2008;91(12):1823-1831.
pubmed - Barry E, Galvin R, Keogh C, Horgan F, Fahey T. Is the timed up and go test a useful predictor of risk of falls in community dwelling older adults: a systematic review and meta-analysis. BMC Geriatr. 2014;14:14.
doi pubmed - Ghislieri M, Gastaldi L, Pastorelli S, Tadano S, Agostini V. Wearable inertial sensors to assess standing balance: a systematic review. Sensors (Basel). 2019;19(19):4075.
doi pubmed - Subramaniam S, Faisal AI, Deen MJ. Wearable sensor systems for fall risk assessment: a review. Front Digit Health. 2022;4:921506.
doi pubmed - Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155-163.
doi pubmed - Freitas SM, Wieczorek SA, Marchetti PH, Duarte M. Age-related changes in human postural control of prolonged standing. Gait Posture. 2005;22(4):322-330.
doi pubmed - van Wegen EE, van Emmerik RE, Riccio GE. Postural orientation: age-related changes in variability and time-to-boundary. Hum Mov Sci. 2002;21(1):61-84.
doi pubmed - O'Sullivan M, Blake C, Cunningham C, Boyle G, Finucane C. Correlation of accelerometry with clinical balance tests in older fallers and non-fallers. Age Ageing. 2009;38(3):308-313.
doi pubmed - Mancini M, Salarian A, Carlson-Kuhta P, Zampieri C, King L, Chiari L, Horak FB. ISway: a sensitive, valid and reliable measure of postural control. J Neuroeng Rehabil. 2012;9:59.
doi pubmed - Ali SM, Arjunan SP, Peter J, Perju-Dumbrava L, Ding C, Eller M, Raghav S, et al. Wearable accelerometer and gyroscope sensors for estimating the severity of essential tremor. IEEE J Transl Eng Health Med. 2024;12:194-203.
doi pubmed - Boonstra MC, van der Slikke RM, Keijsers NL, van Lummel RC, de Waal Malefijt MC, Verdonschot N. The accuracy of measuring the kinematics of rising from a chair with accelerometers and gyroscopes. J Biomech. 2006;39(2):354-358.
doi pubmed - Dejnabadi H, Jolles BM, Aminian K. A new approach to accurate measurement of uniaxial joint angles based on a combination of accelerometers and gyroscopes. IEEE Trans Biomed Eng. 2005;52(8):1478-1484.
doi pubmed - Wairagkar M, Villeneuve E, King R, Janko B, Burnett M, Agarwal V, Kunkel D, et al. A novel approach for modelling and classifying sit-to-stand kinematics using inertial sensors. PLoS One. 2022;17(10):e0264126.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.