| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://jocmr.elmerjournals.com |
Original Article
Volume 17, Number 7, July 2025, pages 386-397
Risk Factors in the Formation of Congenital Malformations of the Ear: Microtia and Atresia of the External Auditory Canal
Assel Imangaliyevaa, d , Rimma Suatbayevaa
, Islam Kamalovb
, Nurbol Kazybayevb
, Askar Imangaliyevc
aDepartment of Otorhinolaryngology, Kazakh National Medical University Named After S.D. Asfendizarov, Almaty, Kazakhstan
bDepartment of Otorhinolaryngology, Almaty Multidisciplinary Clinical Hospital, Almaty, Kazakhstan
cDepartment of Biomedical Disciplines, Kaspian University, Almaty, Kazakhstan
dCorresponding Author: Assel Imangaliyeva, Department of Otorhinolaryngology, Kazakh National Medical University Named After S.D. Asfendizarov, Almaty, Kazakhstan
Manuscript submitted February 12, 2025, accepted July 4, 2025, published online July 31, 2025
Short title: Risk Factors for Congenital Ear Malformations
doi: https://doi.org/10.14740/jocmr6205
| Abstract | ▴Top |
Background: The main study aims are to determine the incidence of congenital ear abnormalities in children in Kazakhstan and their risk factors. This research examined the medical treatment given to children with congenital malformations and the medical and social aspects impacting them and their parents. It also evaluated congenital ear deformity children’s quality of life.
Methods: This retrospective, cross-sectional study was conducted in two public health maternity hospitals in Kazakhstan and aimed to investigate 975 consecutive children delivered therein. The study utilized hospital records to assess various factors related to neonatal health and outcomes in the sampled population.
Results: The study revealed significant associations between congenital ear malformation and various factors: parental consanguinity (P = 0.001), maternal alcohol consumption (P = 0.020), cesarean section (P = 0.000), stillbirth/prenatal mortality (P = 0.005), and maternal medication use (P = 0.002). Surgical interventions comprised 68% of treatments, with non-surgical methods covering all cases, emphasizing a comprehensive approach. Maternal alcohol consumption (P = 0.005) and drug use (P = 0.002) showed notable associations with congenital malformations. Cesarean section (P = 0.048) and lower gestational age (P = 0.001) were linked to prenatal complications. Maternal behaviors like smoking (P = 0.010) and vitamin intake (P = 0.009) also impacted neonatal health.
Conclusions: These findings stress the importance of targeted interventions to mitigate risks in at-risk populations. Congenital ear malformations, influenced by genetics and environment, require targeted interventions. Surgical and non-surgical treatments address physical challenges, emphasizing holistic care for improved quality of life and well-being.
Keywords: Congenital abnormalities; Ear canal; Microtia; Risk factors; External; Auditory canal
| Introduction | ▴Top |
Congenital malformations of the ear, including microtia and external auditory canal atresia, pose significant clinical and public health challenges. These conditions can impair hearing, communication, and psychological well-being, yet their causes remain poorly understood, limiting both prevention and treatment efforts [1]. Anatomically, ear anomalies may affect the outer, middle, or inner ear, involving structural as well as functional impairments.
Recent studies suggest a potential link between the oxalate-degrading activity of the gut microbiota and increased risk for both cardiovascular disease and congenital ear malformation (CEM) such as microtia and atresia [2]. External ear malformations affect approximately 5% of the population, with congenital aural atresia, which often involves both the external and middle ear, being the most common. Microtia refers to an underdeveloped pinna, whereas anotia denotes complete absence of the pinna [3].
These anomalies are typically classified as malformations (e.g., microtia, anotia, preauricular skin tags, or sinuses) and deformations (e.g., cryptotia, conchal crus, lop ear, Spock ear, and prominent ear) [4]. The prevalence of congenital aural atresia in Argentina varies significantly by geographic region and ethnicity, with incidence rates ranging from 1.9 to 20.9 per 10,000 live births. Higher rates among Amerindian populations suggest a possible genetic predisposition [5].
A 12-month clinical evaluation of the Adhesive Bone Conduction Hearing Device (ADHEAR)™ system in children with congenital aural atresia demonstrated consistent improvements in hearing thresholds, speech recognition, and user satisfaction. The study also reported high device acceptance and no observed complications [6]. In addition, the use of bone conduction hearing aids in a cohort of 42 children under the age of 2 showed significant progress in auditory perception and speech development in both unilateral and bilateral cases [7].
During the first trimester, the embryo is highly vulnerable to factors that can lead to congenital anomalies - birth defects affecting about 3% of infants and causing up to 30% of pediatric hospitalizations by age 5. Causes include genetics, environmental exposures, maternal health, substance use, and nutrition, though many cases remain unexplained [8]. Mental and behavioral disorders associated with substance use have been identified as significant contributors to CEMs [9]. The ADHEAR device provides noninvasive, pressure-free hearing support with aesthetic comfort, ideal for conductive hearing loss even during sleep or bathing [10].
Recent studies show that ADHEAR offers comparable hearing outcomes to implant and softband systems, validating it as a noninvasive option [11]. A study of 14 children with aural atresia found that adhesive bone conduction device (aBCD) and passive transcutaneous bone conduction implant (ptBCI) offered similar hearing gains and user satisfaction levels [12].
Artificial intelligence (AI), radiomics, and telemedicine are revolutionizing the care for congenital ear anomalies by improving diagnosis, treatment, and global accessibility [13].
Studies support the effectiveness of implantable hearing systems. The Baha Attract system showed clear benefits over unaided hearing, with high patient satisfaction despite minor discomfort [14]. An ongoing trial of a new osseointegrated steady-state implant (OSI) implant has confirmed its safety and effectiveness, with marked improvements in speech recognition even in noisy settings [15]. Additionally, another ongoing trial on a new OSI implant has confirmed its safety and efficacy, with marked improvements in speech recognition even in noisy settings [16].
Another study using the Baha Attract system in four male subjects (mean age: 13.25 years) reported a mean air-bone gap of 48 dB after 1 year. Successful outcomes were observed within 6 to 12 months, indicating the system’s potential for patients with microtia-anotia and conductive or mixed hearing loss [17]. Despite technological and surgical progress, children with CEMs still face care barriers due to limited awareness, financial issues, and fragmented systems. Coordinated, multidisciplinary care spanning otolaryngology, plastic surgery, audiology, speech therapy, and psychosocial support is essential [18]. Scientific research in genetics, embryology, and clinical outcomes enhances diagnosis and treatment. Innovations like three-dimensional (3D) printing, tissue engineering, and advanced auditory implants support personalized interventions [19].
Progress in treatment is increasingly supported by innovative models of care, including multidisciplinary clinics, centralized referral systems, and collaborative care pathways. These models enhance access, reduce treatment delays, and improve patient satisfaction. Additional resources such as telemedicine, educational platforms, and support groups assist families in navigating care and fostering community support [20].
Nonetheless, several challenges persist, including variability in treatment outcomes, the psychosocial effects of congenital ear anomalies, and inequities in access to specialized care. These issues underscore the importance of long-term outcome studies, policy reform, and initiatives aimed at promoting health equity [21]. Early identification remains essential, as timely surgical correction is the primary reconstructive option for older infants and young children [22].
In conclusion, scientific-based approaches hold immense promise for advancing the medical and organizational care of children with CEMs. By leveraging interdisciplinary expertise, technological innovations, and collaborative partnerships, healthcare providers can deliver personalized interventions, optimize treatment outcomes, and enhance the overall well-being of affected individuals and their families. This research topic serves as a call to action for prioritizing evidence-based practices, fostering innovation, and promoting inclusivity in the management of CEMs. Purpose of the study is to improve the provision of medical and organizational care to children with congenital ear problems.
Research objectives
This study aims to: 1) study the incidence of congenital ear anomalies in children in the regions of Kazakhstan; 2) identify risk factors in the formation of CEM; 3) conduct an analysis and determine the level of medical care provided to children with congenital ear problems; 4) identify medical and social determinants of children and their parents with CEM; 5) evaluate the quality of life of children with CEM; and 6) develop evidence-based recommendations for organizing medical and organizational care for children with congenital ear problems.
| Materials and Methods | ▴Top |
Study design
This research, which is a hospital-based records study, was designed to examine the relationship between maternal factors and CEMs among children through a secondary analysis of hospital records. We used consecutive sampling of the children delivered within these hospitals. Also, as part of this sub study, we analyzed the data that relayed quality of life concerns which was a case series with purposes of data collection as planned and a review of the content. In order to standardize the text, a specific incidence period for new cases of CEMs was provided within this time frame to distinguish incidence from prevalence in all figures.
Study population
The study population consists of 975 neonates, all of whom were delivered in two public health maternity hospitals in Kazakhstan. The study timeframe spanned from January 1, 2020, to December 31, 2022, for a total study duration of 3 years. These neonates were part of a consecutive sampling of children born within the hospitals. In this study, data were available on the clinical characteristics of the participants, including age, weight at birth, and presence of any comorbidities. These characteristics were collected from the Medical Birth Registry, which provided essential information on the neonates’ health status at the time of birth.
Sampling technique
A total of 975 neonates were included in the survey through consecutive sampling of children, who had been delivered in these hospitals.
Exclusion criteria
To ensure the study’s consistency and validity, specific exclusion criteria were applied. Children with acquired ear malformations due to trauma or infection were excluded, as were those with incomplete medical records, including missing maternal health history or prenatal care details. Only children born at the two designated public health maternity hospitals in Kazakhstan were included, excluding those born outside these hospitals or transferred immediately after birth. Additionally, children with other severe genetic conditions or syndromes that could confound the study were excluded, ensuring a focus on CEMs specifically. The exclusion criteria also included children with congenital malformations unrelated to ear anomalies, or any conditions that would obscure the results of the study
Data collection
All charts identified from the Medical Birth Registry of the deliveries at the hospital were reviewed for the presence of congenital ear anomalies. For this study, CEMs were defined based on the previously established criteria: microtia, anotia, preauricular skin tags, and sinuses. Additionally, congenital ear deformations included conchal crus, cryptotia, helical rim deformities, lidding/lop ear, Stahl’s/Spock ear, and prominent ear. Microtia was classified using the Marx classification system, and only patients with grade II microtia or higher were included in the study to ensure consistency in categorization.
All patients with congenital ear anomalies were defined through comprehensive examinations conducted by a board-certified plastic surgeon and an otolaryngologist, ensuring a standardized approach to diagnosis. This dual-examiner method was employed to reduce bias and enhance diagnostic accuracy, acknowledging that different specialties may vary in their assessments of congenital ear conditions.
Quantitative data concerning medical and social determinants and the quality of life of children with congenital malformations were gathered through a combination of medical record reviews and parental interviews. Variables collected from medical records included maternal health history, prenatal care records, family medical histories, and the incidence of congenital ear anomalies. Interviews with parents or guardians provided insights into additional medical and social determinants affecting the care and well-being of the children.
Parents were recruited for prospective interviews and quality of life assessments through hospital follow-up visits and referrals from pediatricians. A total of 975 neonates were surveyed, with consecutive sampling of children who had been delivered in these hospitals. Out of the contacted parents, 80% responded, resulting in a response rate of 80%. Among the responding parents, 65% completed the quality-of-life assessments for their children, while 35% filled out the assessments themselves.
Validated health-related quality of life (HRQoL) assessment tools specific to pediatric populations were administered to evaluate the physical, emotional, and social well-being of the children with CEMs and their parents.
Statistical analysis
Descriptive statistics were employed to summarize demographic and clinical characteristics, including the incidence rates of CEMs across different groups. Associations between maternal and social factors and CEMs were initially explored using univariate analysis with Chi-square tests for categorical variables. Continuous variables were analyzed using t-tests or analysis of variance (ANOVA) where applicable. For multivariate analysis, logistic regression was performed to identify independent risk factors and calculate odds ratios (ORs) with 95% confidence intervals (CIs). A significance threshold of P < 0.05 was applied throughout. Qualitative interview data were subjected to thematic analysis to uncover key themes and sub-themes reflecting the quality of life and care experiences of children with CEMs. All statistical analyses were conducted using the Statistical Package for the Social Sciences (SPSS) software (version 26). In the multivariate analysis, the factors considered (adjusted) included parental consanguinity, maternal alcohol consumption, medication during pregnancy, cesarean section, abortions, maternal smoking, vitamin and iron supplementation, and dysmorphia, where applicable.
Ethical considerations
Ethical approval for this study was obtained from the Institutional Review Boards of both participating maternity hospitals in Kazakhstan prior to data collection. The study adhered to the principles outlined in the Declaration of Helsinki. Confidentiality and privacy of patient data were strictly maintained by anonymizing all records and securely storing sensitive information. Parental informed consent was obtained for all interviews and quality of life assessments. Participants were informed of their right to withdraw at any time without any effect on their medical care. All procedures were conducted with respect for participants’ rights and well-being.
| Results | ▴Top |
Table 1 shows that out of 975 neonates, 25 cases (2.56%) were diagnosed with CEMs. The incidence was slightly higher in males (2.62%) than females (2.52%), with overall rates of 26.86 and 25.75 cases per 1,000 respectively. Neonates with CEM had a slightly higher mean age at assessment (1.3 ± 0.6 days) and a notably lower mean birth weight (2.8 ± 0.6 kg) compared to those without CEM (3.2 ± 0.4 kg). Additionally, 14 (56%) of the children with CEM presented with other comorbidities, highlighting the clinical complexity associated with these malformations. The comorbidities observed in neonates with CEM included congenital heart defects, renal anomalies, cleft lip/palate, limb deformities, and craniofacial syndromes, indicating that many cases occurred alongside other systemic malformations. The overall incidence rate was calculated at 26.30 per 1,000 neonates.
 Click to view | Table 1. Demographic and Clinical Profile With Incidence of CEM Among Neonates in Two Public Hospitals in Kazakhstan |
Table 2 presents the results of a Chi-square test of significance analyzing medical and social determinants associated with CEM. Several factors were examined including sex, parental consanguinity, maternal employment, dysmorphia, maternal smoking during pregnancy, maternal alcohol consumption, premature birth, cesarean section and its implications for birth, stillbirth and prenatal mortality, maternal iron supplementation, maternal calcium intake, maternal vitamin supplementation, and maternal medication use. The analysis reveals statistically significant associations between CEM and parental consanguinity (P = 0.001), maternal alcohol consumption (P = 0.020), cesarean section and its implications for birth (P = 0.000), and stillbirth and prenatal mortality (P = 0.005). Additionally, maternal medication use showed a significant association (P = 0.002). These findings suggest potential risk factors or correlations between these variables and the occurrence of CEM, highlighting the importance of further investigation and potentially targeted interventions or preventive measures in at-risk populations. Other variables did not demonstrate statistically significant associations with CEM in this analysis.
 Click to view | Table 2. Medical and Social Determinants of Congenital Ear Malformation |
Univariate analysis was chosen with Chi-squared testing to identify associations between each individual factor and CEM. This approach was preferred over logistic regression, as the primary objective was to examine the presence of relationships rather than to model the relationship quantitatively. Logistic regression assumes a linear relationship between the independent variables and the dependent variable, which may not hold true for all factors in this context.
Table 3 and Figure 1 illustrate the diverse array of medical care provided to children with CEM, categorizing treatments into surgical and non-surgical approaches.
 Click to view | Table 3. Level of Medical Care Provided to Children With CEM, Including Surgical and Non-Surgical Treatment Modalities and Their Frequencies and Percentages |
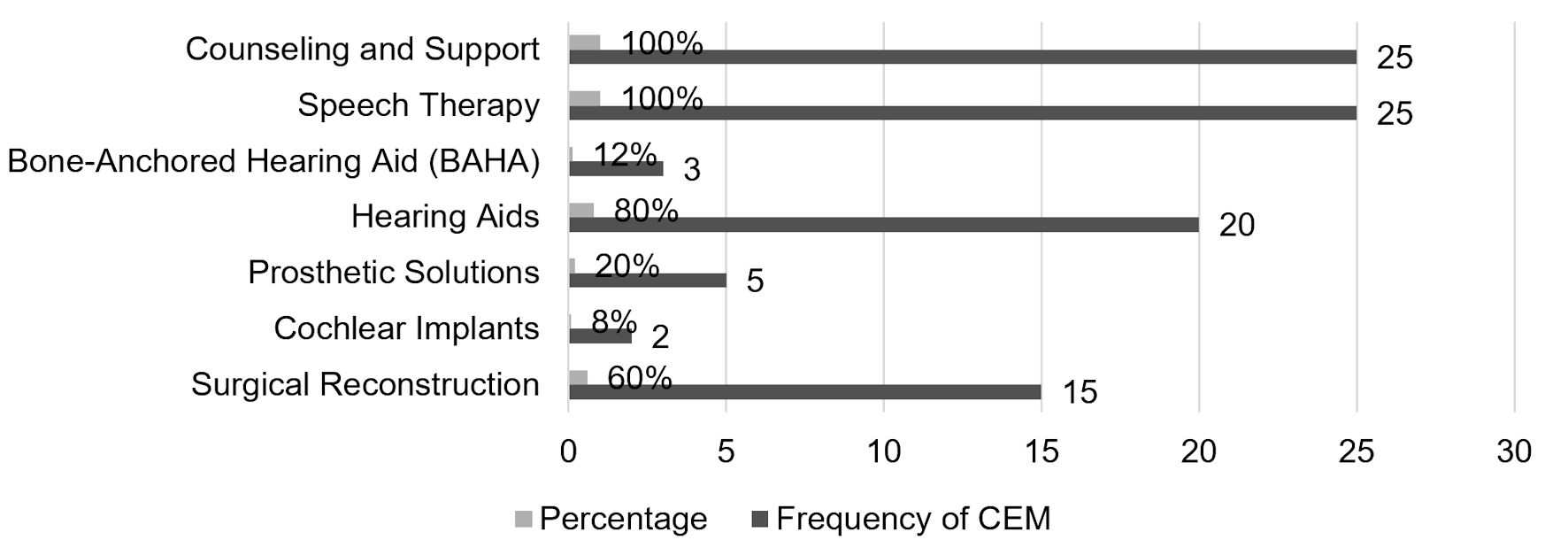 Click for large image | Figure 1. Graphical presentation of the level of medical care. CEM: congenital ear malformation. |
Surgical interventions, including surgical reconstruction and cochlear implants, accounted for 68% of cases, indicating a significant reliance on invasive procedures for addressing CEM. Surgical reconstruction primarily consists of microtia repair, which may involve techniques such as alloplastic implants or rib grafting. Patients in this study were followed for an average of 18 months, ensuring sufficient time to assess the outcomes of these procedures.
Conversely, non-surgical methods such as prosthetic solutions, hearing aids (including bone-anchored options like bone-anchored hearing aid (BAHA)), speech therapy, and counseling/support, collectively covered all cases, suggesting a multifaceted approach to managing CEM beyond surgical interventions alone. Notably, among children diagnosed with CEM, 80% received hearing aids and 100% underwent speech therapy, highlighting the critical role of auditory and communicative rehabilitation in managing CEM-related challenges. Regarding the third column “frequency of CEM”, this represents the N value for each treatment modality (Table 3). It should be clarified to avoid confusion. Additionally, bone-anchored hearing aid placement is indeed categorized as a surgical procedure and should be included in the surgical treatment statistics.
Table 4 presents the results of a multivariate analysis examining various risk factors associated with CEM. The analysis was adjusted for confounding variables including parental consanguinity, maternal alcohol consumption, medication during pregnancy, cesarean section, abortions, maternal smoking, vitamin and iron supplementation, and dysmorphia, where applicable. Variables were selected for inclusion based on prior literature and significance in univariate analysis (P < 0.20), and multicollinearity was assessed prior to model fitting. The table includes ORs for each independent variable along with their 95% CIs and P values. Notable findings include statistically significant associations between CEM and maternal alcohol consumption (OR = 12.73; 95% CI: 1.81 - 46.73; P = 0.005) and medication use during pregnancy (OR = 22.84; 95% CI: 1.19 - 10.42; P = 0.002). It is important to interpret wide CIs cautiously, as they reflect variability and potential sample size limitations. Common medications considered relevant include antinausea drugs (e.g., ondansetron), antibiotics (e.g., penicillins), and pain relievers (e.g., acetaminophen). Antidepressants and antihypertensives like methyldopa are also used, whereas some anticonvulsants such as valproic acid are contraindicated due to teratogenicity. Healthcare providers should be consulted for safe medication management during pregnancy. Furthermore, parental consanguinity and cesarean section showed significant associations with stillbirth outcomes. The model explains a modest proportion of variance (R2 values), indicating other unmeasured factors may also influence outcomes. These findings highlight important risk factors and the need for targeted interventions and further research.
 Click to view | Table 4. Risk Factors of Congenital Malformations and Multivariate Analyses |
Thematic analysis
Table 5 provides a clear representation of the main themes identified in the thematic analysis along with their corresponding sub-themes. The thematic analysis of responses from children with CEM revealed several key themes regarding their HRQoL. These themes included “physical challenges”, highlighting the discomfort and hearing difficulties experienced by many participants. “Emotional impact” emerged as another prominent theme, with children expressing feelings of self-consciousness, anxiety, and frustration related to their ear condition. “Social interactions” were also influenced, as indicated by variations in peer acceptance, participation in social activities, and friend support. Additionally, “functional limitations” were identified, with participants reporting difficulties in specific tasks and activity limitations.
 Click to view | Table 5. Theme and Sub-Themes of Quality of Life of Children With CEM |
Findings
Physical challenges
Participants frequently reported experiencing various physical challenges associated with their CEM. Discomfort in ears was a prevalent issue, with one respondent stating, “I often feel pain and discomfort in my ears, especially when it is windy.” Hearing difficulties were also commonly mentioned, with a participant remarking, “I struggle to hear clearly, especially in noisy environments like the playground.” Additionally, variations in energy levels were noted, as reflected in a response indicating, “I feel tired more quickly than my friends, which affects my ability to keep up with them during activities.”
Emotional impact
The emotional impact of CEM was evident among participants, with self-consciousness emerging as a significant concern. One respondent expressed, “I feel embarrassed about my ears’ appearance, and I try to hide them with my hair.” Anxiety was also prevalent, as articulated by a participant who said, “I worry that others will make fun of me because of my ears, so I often feel anxious in social situations.” Furthermore, frustration was a common emotion, with a participant stating, “It is frustrating when I cannot hear properly or when my ears hurt.”
Social interactions
Participants discussed various aspects of their social interactions affected by their CEM. Peer acceptance was highlighted as crucial, with some respondents expressing positive experiences such as, “My friends accept me for who I am, regardless of my ears.” However, others indicated challenges, with one participant stating, “Some kids tease me because of my ears, which makes me feel left out.” Participation in social activities varied, with some participants actively engaging despite their condition, while others reported hesitancy or avoidance. Friend support emerged as a significant source of comfort for many participants, as reflected in responses such as, “My friends understand my condition and support me, which helps me feel better about myself.”
Functional limitations
Functional limitations were commonly reported by participants, impacting various aspects of daily life. Difficulty with specific tasks was frequently mentioned, with a participant noting, “I struggle to hear instructions in class, which makes it hard to keep up with schoolwork.” Activity limitations were also prevalent, as indicated by responses such as, “I avoid participating in sports because my ears cannot handle the physical activity.”
| Discussion | ▴Top |
The current study shows that the incidence rate of 26.86 cases per 1,000 was among males as compared to an incidence rate of 25.75 cases per 1,000 among females. The overall incidence rate was 26.30 cases per 1,000 persons, indicating a slightly higher prevalence of CEM in males compared to females, with a slight variation in incidence rates between sex. Another study conducted in United States, discovered that males have a higher occurrence of CEMs compared to females. The incidence rates between sex vary slightly. Additionally, 10% of the cases involved congenital sensorineural hearing loss and inner ear malformations, with 58.33% being males and 41.67% being females among children with CEM [23]. Another study reported that CEM had a prevalence rate of 39.5%, with a higher occurrence in males compared to females [24]. Similar studies conducted in Kazakhstan and other geographic locations reported similar trends in the prevalence of CEM, with males being more affected. However, the exact rates can vary depending on environmental and socioeconomic factors. The results align with the greater occurrence of CEM in males than in females, as noted in the present investigation.
Recent genetic studies have further elucidated the hereditary factors influencing the pathogenesis of CEM, particularly in microtia. Key mutations in genes such as EYA1 and HMX1 have been identified as contributing factors to microtia and associated anomalies, reinforcing the genetic basis of these conditions. A 2024 study reported a novel de novo EYA1 frameshift mutation (c.1697_1698delinsT) in an 8-year-old patient with branchio-oto-renal syndrome (BORS), bilateral microtia, hearing loss, and vestibular hypofunction. This mutation results in a loss-of-function via premature termination (p.Lys566IlefsTer73) and was absent in the parental genomes, confirming its pathogenicity under the American College of Medical Genetics and Genomics (ACMG) guidelines [25]. Additionally, a 2023 study identified an EYA1 splicing mutation (c.1050+4 A>C) in a Chinese branchio-oto syndrome (BOS) family, which disrupted EYA1-SIX1 protein interactions and nuclear translocation, leading to reduced protein stability and impairing craniofacial development pathways [26]. These findings highlight the growing body of evidence supporting the genetic component in CEM. Moreover, isolated microtia, previously believed to follow a pattern of autosomal dominant inheritance, now demonstrates polygenic/multifactorial inheritance, revising prior assumptions [27]. This further supports the need for a comprehensive genetic approach in understanding congenital ear anomalies.
The current study analysis shows statistically significant associations between CEM and various risk factors, including parental consanguinity (P = 0.001), maternal alcohol consumption (P = 0.020), cesarean section implications (P = 0.000), stillbirth and prenatal mortality (P = 0.005), and maternal medication use (P = 0.002). These findings suggest that these factors may contribute to the risk of CEM, highlighting the importance of targeted interventions or preventive measures in populations at risk. In studies conducted in Kazakhstan, certain environmental factors, such as prenatal exposure to pollutants, were also identified as risk factors for CEM, adding another layer of complexity to the understanding of its etiology. Additional research on congenital ear abnormalities has also investigated several aspects linked to CEM. Research conducted at UT Southwestern Medical Center (USA) investigating the occurrence of inner ear abnormalities in infants with congenital sensorineural hearing loss, found a connection between inner ear malformations and a family history of hearing loss, indicating the possible hereditary impact on CEM [28]. Furthermore, research conducted in China on microtia, a congenital ear abnormality, documented the occurrence of congenital ear abnormalities throughout several generations of a family, suggesting the significant role of genetic inheritance in certain ear deformities [29]. The aforementioned research, in conjunction with the Chi-square test findings, substantially enhance our comprehension of the many elements linked to CEM, including genetic, environmental, and medical causes. The results emphasize the intricate characteristics of CEM and the need of taking into account various elements in studies and therapeutic treatments concerning this illness.
Multivariate analysis conducted on risk factors associated with CEMs revealed significant associations between maternal and prenatal factors and CEM. Notably, maternal alcohol consumption (P = 0.005) and drug use (P = 0.002) were found to be linked to CEMs. Additionally, cesarean section (P = 0.048) and lower gestational age (P = 0.001) were associated with prenatal complications. Maternal behaviors such as smoking during pregnancy (P = 0.010) and vitamin intake (P = 0.009) also demonstrated significant associations with Apgar scores. These findings highlight the intricate relationship between maternal behaviors and prenatal factors in determining neonatal health outcomes, emphasizing the importance of targeted interventions to mitigate associated risks. A comparison with studies from Kazakhstan reveals that although the trends are similar, the impact of maternal nutrition and health services availability appears to be more pronounced in countries with less access to healthcare resources. When considering these results in the context of CEM in another study conducted in east China, it is crucial to acknowledge that such malformations may have both genetic and acquired origins, with approximately 30% associated with syndromes [30]. A study conducted in population of Indonesia shows that non-genetic risk factors for specific types of CEMs, such as microtia/anotia, include maternal pregestational diabetes and the maternal use of isotretinoin [31]. Moreover, congenital ear deformities can arise from prenatal exposure to certain drugs, including alcohol as shown in another study conducted in Portugal [32]. Therefore, the significant associations identified in the multivariate analysis between maternal alcohol consumption, drug use, and neonatal health outcomes may have implications for the development of CEM. This complex interplay between maternal behaviors and prenatal factors, as revealed in the multivariate analysis, aligns with the understanding that CEM can be influenced by various maternal and prenatal factors, encompassing both genetic and non-genetic elements [33]. This underscores the necessity for comprehensive prenatal care and targeted interventions to mitigate associated risks and improve neonatal health outcomes, including the prevention of CEM.
The present research elucidates the treatment strategies for congenital ear deformity in children, emphasizing a substantial dependence on surgical procedures, which constituted 68% of cases, including surgical reconstruction and cochlear implants. Nevertheless, all instances were effectively addressed by noninvasive approaches, including prosthetic devices, hearing aids (including bone-anchored alternatives like BAHA), speech therapy, and counseling/support. Hearing aids were used in 80% of CEM cases, while speech therapy was applied in 100% of CEM cases. This highlights the significance of auditory and communicative rehabilitation in addressing problems associated with CEM. Furthermore, separate research conducted in Netherlands demonstrates that noninvasive ear molding treatment has quite favorable results overall. Furthermore, it suggests that with additional training and validation, machine learning methods such as Convolutional Neural Networks can effectively replicate provider assessment, eliminating the subjective nature of human evaluation. This makes it a reliable tool for identifying ear deformities and evaluating outcomes [34]. A separate study revealed that individuals with one-sided ear deformities experienced an increase in both the length and width of both their affected and healthy ears during the treatment period. This led to a balance between the two after 3 weeks. In individuals with deformities in both ears, there was a rapid increase in the length and width of both ears within the initial 3 weeks of treatment, followed by a gradual equalization of these measurements after the treatment. Ear molding is a crucial technique for addressing congenital auricular deformities, and it may enhance the length and breadth of the ear. Prompt identification and early commencement of therapy are essential in the treatment of congenital auricular deformity [35]. In addition, research on CEM has investigated alternative therapeutic methods, such as ear molding and splinting, to rectify ear abnormalities. These approaches have shown significant effectiveness, as documented in many publications [36]. These results are consistent with the comprehensive strategy to controlling CEM, which include non-surgical techniques to treat the illness. To summarize, the outcomes of the various medical treatments given to children with CEM emphasize the substantial dependence on surgical procedures, as well as the significance of non-surgical approaches like ear molding, hearing aids, and speech therapy in managing CEM-related difficulties. Additional research has also shown the efficacy of non-surgical methods in rectifying congenital ear problems, hence endorsing the comprehensive approach to addressing CEM.
This study also discusses the quality of life of children with CEM. The study participants in the thematic analysis frequently reported enduring physical challenges associated with their CEM, including discomfort, pain, and hearing difficulties, especially in noisy environments. Emotional ramifications were pronounced, with self-consciousness, anxiety, and frustration prevalent due to concerns about appearance and social acceptance. Social interactions were influenced by peer acceptance, teasing, and the varying degrees of participation in activities, with friend support serving as a significant source of comfort. Functional limitations, such as difficulty hearing instructions in class and avoiding sports due to physical constraints, were commonly mentioned, impacting daily life significantly. Overall, the current study analysis highlights the multifaceted impact of CEM on individuals’ physical, emotional, and social well-being, underscoring the importance of support and understanding in coping with these challenges.
Multiple studies have also emphasized the diverse obstacles encountered by people with congenital ear abnormalities. A study conducted on individuals diagnosed with microtia revealed that hearing impairment may have adverse emotional consequences, but reconstructive surgery notably enhanced their HRQoL [37]. Other research on notable ears in children highlighted the correlation between this deformity and reduced self-confidence, social seclusion, and worse academic achievement [38]. In addition, children with microtia may suffer from diminished auditory function as a result of underdeveloped or absent ear canals, which may significantly affect their everyday activities [39]. These results emphasize the need of assistance and comprehension in dealing with the physical, emotional, and social difficulties linked to congenital ear abnormalities. The creation and assessment of specialized quality of life measures for people with congenital external and middle ear abnormalities have also been emphasized as beneficial for therapeutic practice. Another study explored the hearing-related quality of life, developmental outcomes, and educational performance in children and young adults with unilateral conductive hearing loss due to aural atresia and showed lower hearing-related quality of life compared to normal-hearing peers, with many needing speech therapy and special educational support. Despite these challenges, most developmental and social-emotional outcomes were within normal ranges, highlighting the importance of close monitoring and support during education [40]. Overall, the current study highlights the need for providing extensive assistance and treatments to tackle the varied consequences of congenital ear abnormalities on afflicted persons, particularly those living in areas with limited access to healthcare.
Conclusions
In conclusion, the comprehensive review and analysis of studies pertaining to CEM underscores the multifaceted nature of this condition and its significant impact on affected individuals across physical, emotional, and social domains. The research elucidates various factors contributing to the incidence and development of CEM, including genetic predispositions, prenatal exposures, and maternal behaviors, highlighting the complex interplay between genetic and environmental influences. Importantly, the findings emphasize the critical role of targeted interventions and preventive measures in mitigating the associated risks of CEM, particularly in populations predisposed to certain risk factors such as parental consanguinity, maternal alcohol consumption, and cesarean section implications. The identification of these modifiable risk factors provides valuable insights for healthcare professionals to implement strategies aimed at reducing the prevalence of CEM and improving neonatal health outcomes. Furthermore, the study underscores the significance of both surgical and non-surgical treatment modalities in managing CEM-related difficulties, including surgical reconstruction, cochlear implants, ear molding, hearing aids, and speech therapy. The efficacy of these interventions in addressing the physical and functional challenges associated with CEM highlights the importance of comprehensive care approaches tailored to individual needs. Additionally, the research sheds light on the profound impact of CEM on the quality of life of affected individuals, emphasizing the need for holistic support and understanding to address the diverse obstacles faced in daily life. The emotional and social ramifications of CEM, including self-consciousness, social seclusion, and academic challenges, underscore the importance of psychological and social support services in promoting well-being and resilience among affected individuals.
Overall, the findings presented in the current study contribute to a deeper understanding of CEM and underscore the importance of multidisciplinary approaches in providing comprehensive care and support to individuals affected by this condition. Future research endeavors aimed at further elucidating the underlying mechanisms and refining therapeutic strategies are crucial in advancing the management and outcomes of congenital ear abnormalities.
Learning points
Based on the findings and conclusions of the study on CEM, the following are the recommendations: 1) Implementing comprehensive prenatal screening protocols to identify potential risk factors associated with CEM, such as parental consanguinity, maternal alcohol consumption, and maternal medication use, can help in early detection and intervention; 2) Launching public health education campaigns to raise awareness about the importance of maternal behaviors during pregnancy, including abstaining from alcohol consumption and avoiding certain medications known to be associated with congenital abnormalities; 3) Providing genetic counseling services to families with a history of CEM or other genetic syndromes to better understand the inheritance patterns and potential risks for future generations; 4) Establishing multi-disciplinary care teams consisting of otolaryngologists, pediatricians, geneticists, psychologists, and social workers to provide comprehensive care and support to individuals with CEM, addressing both medical and psychosocial needs; 5) Implementing early intervention programs that include access to surgical procedures, hearing aids, speech therapy, and psychosocial support services to optimize outcomes and improve the quality of life for children with CEM; 6) Supporting further research initiatives aimed at elucidating the underlying genetic and environmental factors contributing to CEM, as well as exploring novel therapeutic approaches, such as ear molding and splinting, to enhance treatment outcomes; 7) Incorporating specialized quality of life measures for individuals with congenital ear abnormalities into clinical practice to better assess and address the physical, emotional, and social impact of CEM on affected individuals; 8) Establishing systems for continued monitoring and evaluation of interventions and outcomes related to CEM to assess effectiveness, identify areas for improvement, and guide future research and healthcare policies.
By implementing these recommendations, healthcare systems can better address the complex challenges associated with CEM and improve outcomes for affected individuals and their families.
Acknowledgments
We would like to express our sincere gratitude to all participants and researchers whose contributions made this study possible. We also express our appreciation to the healthcare professionals and institutions involved in the care and support of people with congenital ear disease.
Financial Disclosure
None to declare.
Conflict of Interest
The authors declare that there are no conflict of interest.
Informed Consent
Parental informed consent was obtained.
Author Contributions
Assel Imangaliyeva: conception and design, data analysis and interpretation, manuscript writing, final approval of manuscript. Rimma Suatbayeva: administrative support, data analysis and interpretation, manuscript writing, final approval of manuscript. Islam Kamalov: provision of study materials, data analysis and interpretation, manuscript writing, final approval of manuscript. Nurbol Kazybayev: collection and assembly of data, data analysis and interpretation, manuscript writing, final approval of manuscript. Askar Imangaliyev: collection and assembly of data, data analysis and interpretation, manuscript writing, final approval of manuscript. All authors contributed equally to the conception and design of the study.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
ADHEAR: Adhesive Bone Conduction Hearing Device; aBCD: adhesive bone conduction device; BAHA: bone-anchored hearing aid; CEM: congenital ear malformation; CI: confidence interval; HRQoL: health-related quality of life; OR: odds ratio; OSI: osseointegrated steady-state implant; ptBCI: passive transcutaneous bone conduction implant; SPSS: Statistical Package for the Social Sciences
| References | ▴Top |
- Lim R, Abdullah A, Wan Hashim WF, Goh BS. Hearing rehabilitation in patients with congenital aural atresia: an observational study in a tertiary center. Egypt J Otolaryngol [Internet]. 2023;39(1):90.
doi - Stepanova N, Tolstanova G, Aleksandrova I, Korol L, Dovbynchuk T, Driianska V, Savchenko S. Gut Microbiota's Oxalate-Degrading activity and its implications on cardiovascular health in patients with kidney failure: a pilot prospective study. Medicina (Kaunas). 2023;59(12):2189.
doi pubmed - Georgakopoulos B, Zafar Gondal A. Embryology, ear congenital malformations. In: StatPearls. Treasure Island (FL) with ineligible companies. 2025.
pubmed - Feijen MMW, van Cruchten C, Payne PE, van der Hulst R. Non-surgical correction of congenital ear anomalies: a review of the literature. Plast Reconstr Surg Glob Open. 2020;8(11):e3250.
doi pubmed - Zernotti ME, Curet CA, Cortasa S, Chiaraviglio M, Di Gregorio MF. Congenital Aural Atresia prevalence in the Argentinian population. Acta Otorrinolaringol Esp (Engl Ed). 2019;70(1):32-35.
doi pubmed - Zernotti ME, Alvarado E, Zernotti M, Claveria N, Di Gregorio MF. One-year follow-up in children with conductive hearing loss using ADHEAR. Audiol Neurootol. 2021;26(6):435-444.
doi pubmed - Cywka KB, Krol B, Skarzynski PH. Effectiveness of bone conduction hearing aids in young children with congenital aural atresia and microtia. Med Sci Monit. 2021;27:e933915.
doi pubmed - Taye M, Afework M, Fantaye W, Diro E, Worku A. Congenital anomalies prevalence in Addis Ababa and the Amhara region, Ethiopia: a descriptive cross-sectional study. BMC Pediatr. 2019;19(1):234.
doi pubmed - Zhylin M, Mendelo V, Karpenko Y, Samara O, Kampi Y, Alexandru. Mental and behavioural disorders as a result of using alcohol and psychoactive substances. Revista de Cercetare si Interventie Sociala [Internet]. 2023;81:117-128. Available from: https://www.ceeol.com/search/article-detail?id=1136529.
- Westerkull P. An adhesive bone conduction system, Adhear, a new treatment option for conductive hearing losses. J Hear Sci [Internet]. 2018;8(2):35-43.
doi - Skarzynski PH, Ratuszniak A, Osinska K, Koziel M, Krol B, Cywka KB, Skarzynski H. A comparative study of a novel adhesive bone conduction device and conventional treatment options for conductive hearing loss. Otol Neurotol. 2019;40(7):858-864.
doi pubmed - Pedrero Escalas MF, Cavalle L, Perez Mora RM, De Paula Vernetta C, Lassaletta Atienza L, Gavilan J. Comparison of adhesive and passive transcutaneous bone conduction systems in atretic children. J Hear Sci [Internet]. 2022;12(4):47-54.
doi - Rakhimov T, Mukhamediev M. Implementation of digital technologies in the medicine of the future. Futurity Medicine [Internet]. 2022;1(2):12-23. Available from: https://www.futurity-medicine.com/index.php/fm/article/view/7.
- den Besten CA, Monksfield P, Bosman A, Skarzynski PH, Green K, Runge C, Wigren S, et al. Audiological and clinical outcomes of a transcutaneous bone conduction hearing implant: Six-month results from a multicentre study. Clin Otolaryngol. 2019;44(2):144-157.
doi pubmed - Cywka KB, Skarzynski PH, Krol B, Hatzopoulos S, Skarzynski H. Evaluation of the Bonebridge BCI 602 active bone conductive implant in adults: efficacy and stability of audiological, surgical, and functional outcomes. Eur Arch Otorhinolaryngol. 2022;279(7):3525-3534.
doi pubmed - Mylanus EAM, Hua H, Wigren S, Arndt S, Skarzynski PH, Telian SA, Briggs RJS. Multicenter clinical investigation of a new active osseointegrated steady-state implant system. Otol Neurotol. 2020;41(9):1249-1257.
doi pubmed - Marfatia H, Shah K, Shelke S, Krishnan K. Baha attract: our experience. Indian J Otolaryngol Head Neck Surg. 2017;69(4):544-548.
doi pubmed - Bush ML, Kaufman MR, McNulty BN. Disparities in access to pediatric hearing health care. Curr Opin Otolaryngol Head Neck Surg. 2017;25(5):359-364.
doi pubmed - Bhagat AC, Kumar J, Garg A, Prakash A, Meher R, Arya S. Imaging in congenital inner ear malformations-An algorithmic approach. Indian J Radiol Imaging. 2020;30(2):139-148.
doi pubmed - Kita SI, Miwa T, Kanai R, Morita Y, Lee S, Koike T, Kanemaru SI. Diagnosing middle ear malformation by pure-tone audiometry using a three-dimensional finite element model: a case-control study. J Clin Med. 2023;12(23):7493.
doi pubmed - Alqarawi N, Alhamidi SA, Alsadoun A, Alasqah I, Mahmud I. Challenges of having a child with congenital anomalies in Saudi Arabia: a qualitative exploration of mothers' experience. Front Public Health. 2023;11:1111171.
doi pubmed - Bhatti SL, Daly LT, Mejia M, Perlyn C. Ear abnormalities. Pediatr Rev. 2021;42(4):180-188.
doi pubmed - Ahmed J, Saqulain G, Khan MIJ, Kausar M. Prevalence & features of inner ear malformations among children with congenital sensorineural hearing loss: A Public Cochlear Implant Centre Experience. Pak J Med Sci. 2020;36(7):1511-1516.
doi pubmed - Zou Y. Congenital ear malformation (CEM). Acta Otolaryngol. 2023;143(sup1):S3-S16.
doi pubmed - He J, Mahmoudi A, Gu Y, Fu J, Yuan Q, Liu W. Case report: A novel mutation in the EYA1 gene in a child with branchiootic syndrome with secretory otitis media and bilateral vestibular hypofunction. Front Genet. 2023;14:1292085.
doi pubmed - Chen A, Ling J, Peng X, Liu X, Mao S, Chen Y, Qin M, et al. A novel EYA1 mutation causing alternative RNA splicing in a chinese family with Branchio-Oto syndrome: implications for molecular diagnosis and clinical application. Clin Exp Otorhinolaryngol. 2023;16(4):342-358.
doi pubmed - Chen X, Ma J, Zhang T. Genetics and epigenetics in the genesis and development of microtia. J Craniofac Surg. 2024;35(3):e261-266.
doi pubmed - D DD, Patil GC. Cross-sectional study to estimate the prevalence of inner-ear anomalies in children with congenital sensorineural hearing loss by high-resolution computed tomography (HRCT) temporal bone scan. Cureus. 2023;15(7):e42160.
doi pubmed - Zhang Y, Wang C, Yang M, Pan B. Inheritance analysis and family history for microtia: A hospital-based study in China. Int J Pediatr Otorhinolaryngol. 2023;171:111613.
doi pubmed - Paul A, Achard S, Simon F, Garcelon N, Garabedian EN, Couloigner V, Celerier C, et al. Congenital abnormalities associated with microtia: a 10-YEARS retrospective study. Int J Pediatr Otorhinolaryngol. 2021;146:110764.
doi pubmed - Ryan MA, Olshan AF, Canfield MA, Hoyt AT, Scheuerle AE, Carmichael SL, Shaw GM, et al. Sociodemographic, health behavioral, and clinical risk factors for anotia/microtia in a population-based case-control study. Int J Pediatr Otorhinolaryngol. 2019;122:18-26.
doi pubmed - Siebold B, Heike CL, Leroux BG, Speltz ML, Drake AF, Johns AL, Kapp-Simon KA, et al. Evaluation of prenatal diabetes mellitus and other risk factors for craniofacial microsomia. Birth Defects Res. 2019;111(11):649-658.
doi pubmed - Tsao PC, Lin HC, Chiu HY, Chang YC. Maternal, perinatal, and postnatal predisposing factors of hearing loss in full-term children: a matched case-control study. Neonatology. 2023;120(5):607-614.
doi pubmed - Hallac RR, Jackson SA, Grant J, Fisher K, Scheiwe S, Wetz E, Perez J, et al. Assessing outcomes of ear molding therapy by health care providers and convolutional neural network. Sci Rep. 2021;11(1):17875.
doi pubmed - Chen Y, Wang W, Wang Y, Mao X. Using ear molding to treat congenital auricular deformities. Front Pediatr. 2021;9:752981.
doi pubmed - Liu C, Wo P, Zhang J, Li J. Nonsurgical molding of congenital auricular deformities and analysis of the correction outcomes: A single-center, retrospective study in east China. Front Pediatr. 2022;10:1031575.
doi pubmed - Widodo DW, Mars R, Suwento R, Alviandi W, Oriza IID, Bardosono S. Satisfaction and health-related quality of life of patients with microtia following reconstructive surgery using the Nagata technique. PLoS One. 2021;16(9):e0256652.
doi pubmed - Carvalho C, Marinho AS, Barbosa-Sequeira J, Correia MR, Banquart-Leitao J, Carvalho F. Quality of life after otoplasty for prominent ears in children. Acta Otorrinolaringol Esp (Engl Ed). 2023;74(4):226-231.
doi pubmed - Truong MT, Liu YC, Kohn J, Chinnadurai S, Zopf DA, Tribble M, Tanner PB, et al. Integrated microtia and aural atresia management. Front Surg. 2022;9:944223.
doi pubmed - Smit AL, Burgers YRW, Swanenburg de Veye HFN, Stegeman I, Breugem CC. Hearing-related quality of life, developmental outcomes and performance in children and young adults with unilateral conductive hearing loss due to aural atresia. Int J Pediatr Otorhinolaryngol. 2021;142:110590.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.