| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://jocmr.elmerjournals.com |
Original Article
Volume 17, Number 6, June 2025, pages 309-319
Impact of Chronic Obstructive Pulmonary Disease Burden on Patients With Atrial Fibrillation: A Nationwide Study
Sherif Eltawansya, n, Faizan Ahmedb, Grishma Sharmac, Pawel Lajczakd, Ogechukwu Obie, Hardik A. Valandf, Bhavin Patelg, Dawood Shehzadh, Mohamed Abugrini, Anam Mubasherj, Asjad Salmank, Joseph Heatonl, Jesus Almendralm
aInternal Medicine Department, Jersey Shore University Medical Center, Neptune, NJ 08831, USA
bDivision of Cardiology, Duke University Hospital, Durham, NC, USA
cDepartment Internal Medicine, Kathmandu University School of Medical Sciences, Dhulikhel, Nepal
dMedical University of Silesia, 40-055 Katowice, Poland
eCollege of Osteopathic Medicine, New York Institute of Technology, Westbury, NY, USA
fDepartment of Internal Medicine, Allegheny General Hospital, Pittsburgh, PA, USA
gDepartment of Internal Medicine, Trinity Health Oakland/Wayne State University, Pontiac, MI, USA
hDepartment of Internal Medicine, University of South Dakota, Sioux Falls, SD, USA
iDepartment of Internal Medicine, Bassett Medical Center, Cooperstown, NY, USA
jDepartment of Internal Medicine, Texas Health Resources Bedford/Denton, TX, USA
kDepartment of Internal Medicine, Carle Health, Urbana-champaign, IL, USA
lDepartment of Internal Medicine, Jersey Shore University Medical Center, Neptune, NJ, USA
mCardiology Department, Jersey Shore University Medical Center, Neptune, NJ, USA
nCorresponding Author: Sherif Eltawansy, Internal Medicine Department, Jersey Shore University Medical Center, Neptune, NJ 08831, USA
Manuscript submitted March 23, 2025, accepted June 12, 2025, published online June 30, 2025
Short title: Impact of COPD on Patients With Afib
doi: https://doi.org/10.14740/jocmr6243
| Abstract | ▴Top |
Background: Chronic obstructive pulmonary disease (COPD) and atrial fibrillation (Afib) are frequently comorbid, with COPD patients exhibiting a higher risk of Afib-related hospitalizations. This study investigated the relationship between COPD and Afib, focusing on 30-day readmission rates and outcomes.
Methods: We conducted a retrospective cohort study using the Nationwide Readmissions Database (NRD) from 2016 to 2020. We included adult patients (≥ 18 years) with a primary diagnosis of Afib while excluding those with December discharges to ensure a complete 30-day follow-up. We compared patients with and without COPD, analyzing 30-day readmission rates, length of stay (LOS), hospital costs, in-hospital mortality, and associated factors using multivariable Cox and logistic regression models.
Results: A total of 1,064,982 patients admitted with Afib were included, of which 873,070 had no COPD, and 191,912 had it. COPD patients were older (73.19 vs. 70.82 years), had a shorter LOS (coefficient = -0.05, P = 0.002, 95% confidence interval (CI): -0.08 to -0.02), and had a higher comorbidity burden (Elixhauser comorbidity index: 5.13 vs. 3.43, P < 0.0001). The 30-day readmission rate was significantly higher in the COPD group (16.0% vs. 9.0%, P < 0.001). Logistic regression revealed that COPD increased the odds of readmission (odds ratio: 1.35, 95% CI: 1.32 to 1.39, P < 0.001).
Conclusion: COPD is a significant risk factor for 30-day readmission and in-hospital mortality among Afib patients, underscoring the need for integrated approaches targeting both diseases.
Keywords: Atrial fibrillation; Chronic obstructive pulmonary disease; Patient readmission; Hospital mortality; Risk factors
| Introduction | ▴Top |
Chronic obstructive pulmonary disease (COPD) is a prevalent respiratory condition characterized by persistent airflow limitation and is commonly comorbid with various cardiovascular diseases. Atrial fibrillation (Afib), a common cardiac arrhythmia, has been particularly interesting due to its association with COPD. Epidemiological studies indicate that patients with COPD have a higher risk of developing Afib and cardiovascular mortality compared to the general population [1-3]. The increased risk of AFib is partially attributable to structural and ventricular changes, such as left ventricular hypertrophy [4]. Moreover, reduced lung function, which is a hallmark of COPD, has been identified as a factor in the increased incidence of Afib [5].
The coexistence of COPD and Afib has been associated with an increased risk of Afib-related readmissions, highlighting the substantial impact of these comorbidities on healthcare utilization and patient outcomes [6, 7]. Patients with COPD are known to have a higher risk of 30-day readmission rates following hospital discharge, contributing to increased healthcare costs.
Understanding the interplay between COPD and Afib within the context of hospital readmission rates is crucial for developing clinical decision-making, improving patient care, and reducing the burden on healthcare systems. This study aimed to evaluate the impact of COPD diagnosis on the 30-day readmission rate, inpatient mortality, and length of stay among patients hospitalized for Afib from the Nationwide Readmissions Database (NRD).
| Materials and Methods | ▴Top |
Data source
This retrospective cohort study used the NRD from 2016 to 2020. The NRD is part of the Healthcare Cost and Utilization Project (HCUP) family of databases developed by the Agency for Healthcare Research and Quality. It contains approximately 18 million unweighted discharges from 2,048 hospitals in 22 states, representing approximately 35 million weighted discharges annually across the United States. All analyses were conducted on weighted data to produce nationally representative estimates. The Cleveland Clinic Institutional Review Board deemed the study exempt because it used de-identified data. This study follows the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines.
Study population
We included adult patients (≥ 18 years) hospitalized with a primary diagnosis of Afib, as defined by ICD-10 codes: I48, I48.0, I48.1, I48.2, I48.3, I48.4, I48.91, I48.92, and I48.9 (Supplementary Material 1, jocmr.elmerjournals.com). Patients discharged in December were excluded to ensure a complete 30-day follow-up period. Patients with COPD were identified using International Classification of Diseases, Tenth Revision (ICD-10) codes J44, J44.0, J44.1, and J44.9. Patients who died during the index hospitalization were excluded from the 30-day readmission analysis. The identification was based on the principal discharge diagnosis coded by hospital staff.
Patient and hospital characteristics
Demographics and hospital-level characteristics extracted from the NRD included age, sex, median household income for the patient’s ZIP code, primary expected payer, hospital size, teaching status, location, and ownership. Clinical variables included diabetes mellitus, hypertension, heart failure, and cor pulmonale. Comorbidities were identified using the Elixhauser Comorbidity Software for ICD-10-CM, which consists of 38 conditions such as hypertension, diabetes, hyperlipidemia, valvular disease, peripheral vascular disease, smoking, alcohol abuse, obesity, chronic pulmonary disease, renal failure, liver disease, cancer, coagulopathy, and anemia. Importantly, heart failure and cor pulmonale were explicitly included as comorbidities and adjusted for in multivariable models. Hospital Afib volume was calculated by summing all weighted Afib admissions at each hospital and stratifying them into quintiles.
Study outcomes
The primary outcome was 30-day all-cause readmission per 100 live discharges among patients hospitalized for Afib. Readmission was defined as any non-elective hospitalization within 30 days of discharge. Only the first readmission was counted. Due to NRD limitations, readmissions outside the index hospitalization state were not captured. Secondary outcomes included in-hospital mortality, length of stay (LOS) of the index hospitalization and readmission, hospitalization costs, Afib-related readmissions, and cause-specific 30-day readmission rates. Comparisons were made between patients with and without COPD.
More information on baseline characteristics, early readmission, and secondary endpoints are included in Supplementary Materials 2-4 (jocmr.elmerjournals.com).
Statistical analysis
Continuous variables were summarized as means and standard deviations or medians and interquartile ranges (IQRs), as appropriate. Categorical variables were presented as frequencies and percentages. To analyze the time to readmission, we used Cox proportional hazards models, with readmission as the event of interest and censoring patients at 30 days if no event occurred. Univariable Cox regression was initially performed to identify candidate variables with a P-value < 0.2, which were subsequently included in the multivariable Cox model, and clinically relevant variables such as heart failure. Linear regression was used for continuous outcomes, such as LOS and hospitalization cost, while logistic regression was used for binary outcomes, including mortality. These models were adjusted for age, sex, and Elixhauser comorbidities.
The Elixhauser Comorbidity Software, refined for ICD-10-CM, identifies 38 comorbid conditions based on secondary diagnoses on admission. These comorbidities are utilized in healthcare research due to their significant impact on clinical outcomes and healthcare utilization. Adjusted estimates with 95% confidence intervals (CIs) were derived using marginal effects, and the Hochberg method was used to adjust for multiple comparisons. All patients were included in the analysis of index hospitalization outcomes; however, patients who died during the index hospitalization were excluded from 30-day readmission analyses.
All statistical analyses accounted for the complex survey design of the NRD, including stratification, clustering, and weighting, in accordance with HCUP recommendations. Analyses were performed using the “svy” package in STATA version 16.1 (StataCorp, College Station, TX). A two-sided P-value of < 0.05 was considered statistically significant.
We used a combination of clinical rationale and univariate P-values (P < 0.1) for variable inclusion. We used sample weights for our NRD survey analysis and Cox regression for model building.
| Results | ▴Top |
Patient characteristics
In this retrospective cohort analysis, we examined the baseline characteristics of 1,064,982 patients admitted with Afib between 2016 and 2020. Among these, 873,070 patients had no COPD, while 191,912 had it. Among these, 865,444 patients with COPD and 188,603 patients without COPD were discharged alive (Table 1). COPD patients were older on average (73.19 vs. 70.82 years, P < 0.0001), had a more extended hospital stay (4.28 vs. 3.26 days, P < 0.0001), and exhibited a greater burden of comorbidities (Elixhauser comorbidity summary: 5.13 vs. 3.43, P < 0.0001).
 Click to view | Table 1. Baseline Characteristics |
The sex distribution between the COPD and the non-COPD group was not significantly different (P = 0.247). Medicare covered more COPD patients with Afib than non-COPD patients (82.30% vs. 70.13%, P < 0.001). Private insurance coverage was lower in the COPD group than in the non-COPD group (9.57% vs. 21.52%, P < 0.001). COPD patients with Afib were more likely to reside in ZIP codes within the 0-25th percentile of median household income than non-COPD patients (33.47% vs. 26.64%, P < 0.001), indicating socioeconomic disparities. Cor pulmonale was higher in the COPD group (0.80) than in the non-COPD group (0.16), with a P value of < 0.001. Additionally, congestive heart failure was also more prevalent in the COPD group (40%) compared to the non-COPD group (58.16%), with a P value of < 0.001.
Hospital characteristics showed that COPD patients with Afib were more frequently admitted to non-teaching metropolitan hospitals (27.18% vs. 25.77%, P < 0.001). The COPD with Afib group was more present in small metropolitan, micropolitan, and non-urban areas (P < 0.001). However, differences in hospital size (small versus medium versus large hospital based on bed size) were not statistically significant (P = 0.064). COPD patients with Afib had higher rates of cardiac arrhythmias (24.47% vs. 22.11%, P < 0.001), renal failure (24.51% vs. 17.87%, P < 0.001), and diabetes (32.88% vs. 26.62%, P < 0.001). COPD patients with Afib had a higher prevalence of do not resuscitate (DNR) orders (10.30% vs. 7.46%, P < 0.001), indicating greater disease severity or different care preferences.
We evaluated the top reasons for readmission in the overall group, the COPD subgroup, and the non-COPD subgroup (Table 2).
 Click to view | Table 2. Top 10 Causes of Atrial Fibrillation Readmission |
Readmission rates
The readmission rates were notably higher in the COPD group (n = 79,861) compared to the control group (n = 29,425). The overall readmission rate across all patients was 10.0%, with COPD patients exhibiting a higher rate than non-COPD patients (16.0±0.3% vs. 9.0±0.29%, P < 0.001, using an adjusted Wald test).
Factors influencing readmission
The logistic regression analysis identified factors associated with 30-day readmission among patients with Afib. COPD was significantly associated with higher odds of readmission (odds ratio (OR) = 1.35, P < 0.001, 95% CI: 1.32 - 1.39; hazard ratio (HR) from the Cox regression = 1.31, P < 0.001, 95% CI: 1.29 - 1.34), indicating that COPD is a substantial risk factor for hospital readmission in this cohort. Older age (OR = 1.01, P < 0.001, 95% CI: 1.01 - 1.01) and higher Elixhauser comorbidity scores were also strongly associated with increased odds of readmission (OR = 1.15, P < 0.001, 95% CI: 1.15 - 1.16).
Socioeconomic factors revealed that Medicaid coverage was associated with higher odds of readmission (OR = 1.28, P < 0.001, 95% CI: 1.23 - 1.33), while private insurance was protective (OR = 0.71, P < 0.001, 95% CI: 0.68 - 0.73). Higher median household income protected against readmission (OR = 0.83 to 0.92 across income quartiles, all P < 0.001).
Hospital characteristics such as teaching status (metropolitan teaching hospitals: OR = 0.97, P = 0.016, 95% CI: 0.95 - 0.99), location (micropolitan counties: OR = 0.87, P < 0.001, 95% CI: 0.82 - 0.92, non-metropolitan counties: OR = 0.82, P < 0.001, 95% CI: 0.77 - 0.87) were associated with lower odds of readmission compared to their respective counterparts.
Congestive heart failure increased the risk of readmission in the study population (HR = 1.26, P < 0.001, 95% CI: 1.24 - 1.29) using Cox regression. Meanwhile, cor pulmonale did not affect that risk (HR = 0.96, P < 0.508, 95% CI: 0.85 - 1.08).
Clinical conditions, such as cardiac arrhythmias (OR = 0.86, P < 0.001, 95% CI: 0.84 - 0.88), were protective against readmission, while renal failure (OR = 1.18, P < 0.001, 95% CI: 1.15 - 1.21) increased the odds of readmission (Table 3).
 Click to view | Table 3. Predictors of Readmission and Mortality |
In-hospital mortality
The in-hospital mortality rate was significantly higher in the COPD group (0.02 ± 0.13 vs. 0.01 ± 0.09, P < 0.001). COPD patients also had a more extended average initial hospital stay (4.28 ± 4.27 vs. 3.26 days ± 3.62, P < 0.001) compared to non-COPD patients.
LOS
The analysis of factors influencing hospital LOS among patients with Afib revealed that patients with COPD had a longer LOS compared to those without COPD (coefficient = -0.05, P = 0.002, 95% CI: -0.08 to -0.02). Older age (coefficient = 0.02, P < 0.001, 95% CI: 0.02 - 0.02) and a higher comorbidity burden (coefficient = 0.61, P < 0.001, 95% CI: 0.60 - 0.62) were associated with longer LOS. With using the adjusted Wald test (difference of means), the COPD group had a longer LOS (4.28 vs. 3.26, P < 0.001); on the other hand, using logistic regression that would allow controlling confounding factors, it demonstrated a slight decrease in LOS over time (coefficient = -0.05, P < 0.001, 95% CI: -0.06 to -0.03). Incorporating congestive heart failure and cor pulmonale led to a decrease in LOS in both factors (regression coefficient = 0.52, P < 0.001, 95% CI: 0.5 - 0.55; regression coefficient = 0.74, P < 0.001, 95% CI: 0.48 - 1.00).
Mortality risks
COPD was associated with a modestly increased hazard of mortality (HR = 1.11, P = 0.004, 95% CI: 1.03 - 1.18). Older age (HR = 1.01, P < 0.001, 95% CI: 1.01 - 1.02) and higher Elixhauser comorbidity scores were strongly linked to increased mortality hazard (HR = 1.13, P < 0.001, 95% CI: 1.11 - 1.15), underscoring the impact of multiple comorbidities on survival. Female sex was protective against mortality (HR = 0.80, P < 0.001, 95% CI: 0.75 - 0.85), as was private insurance (HR = 0.84, P = 0.009, 95% CI: 0.74 - 0.96) and higher median household income (HR = 0.83, P < 0.001, 95% CI: 0.75 - 0.92).
Conversely, having a DNR order significantly increased the hazard of mortality (HR = 8.02, P < 0.001, 95% CI: 7.45 - 8.63). Hospital characteristics, such as being located in smaller metropolitan areas (HR = 1.21, P = 0.033, 95% CI: 1.02 - 1.44) and non-urban areas (HR = 1.48, P = 0.005, 95% CI: 1.13 - 1.94), were also associated with an increased hazard.
Cor pulmonale and congestive heart failure did not alter mortality risk after applying Cox regression, with HRs of 0.91 (P = 0.506, 95% CI: 0.69 - 1.21) and 0.98 (P = 0.579, 95% CI: 0.93 - 1.04), respectively.
| Discussion | ▴Top |
COPD is a significant risk factor for 30-day readmission and in-hospital mortality among patients hospitalized with Afib. Our study analyzed data from 1,064,982 patients admitted with Afib between 2016 and 2020 from the NRD. The analysis revealed that Afib patients with COPD had significantly higher odds of 30-day readmissions compared to those without COPD (OR = 1.35, 95% CI: 1.32 - 1.39, P < 0.001) (Fig. 1). Additionally, COPD patients had higher in-hospital mortality rates (Fig. 2). LOS had conflicting results, showing a longer LOS in the COPD group, as indicated by a statistically significant difference in means. Still, after adjusting for confounders using linear regression, the COPD patients exhibited a shorter LOS.
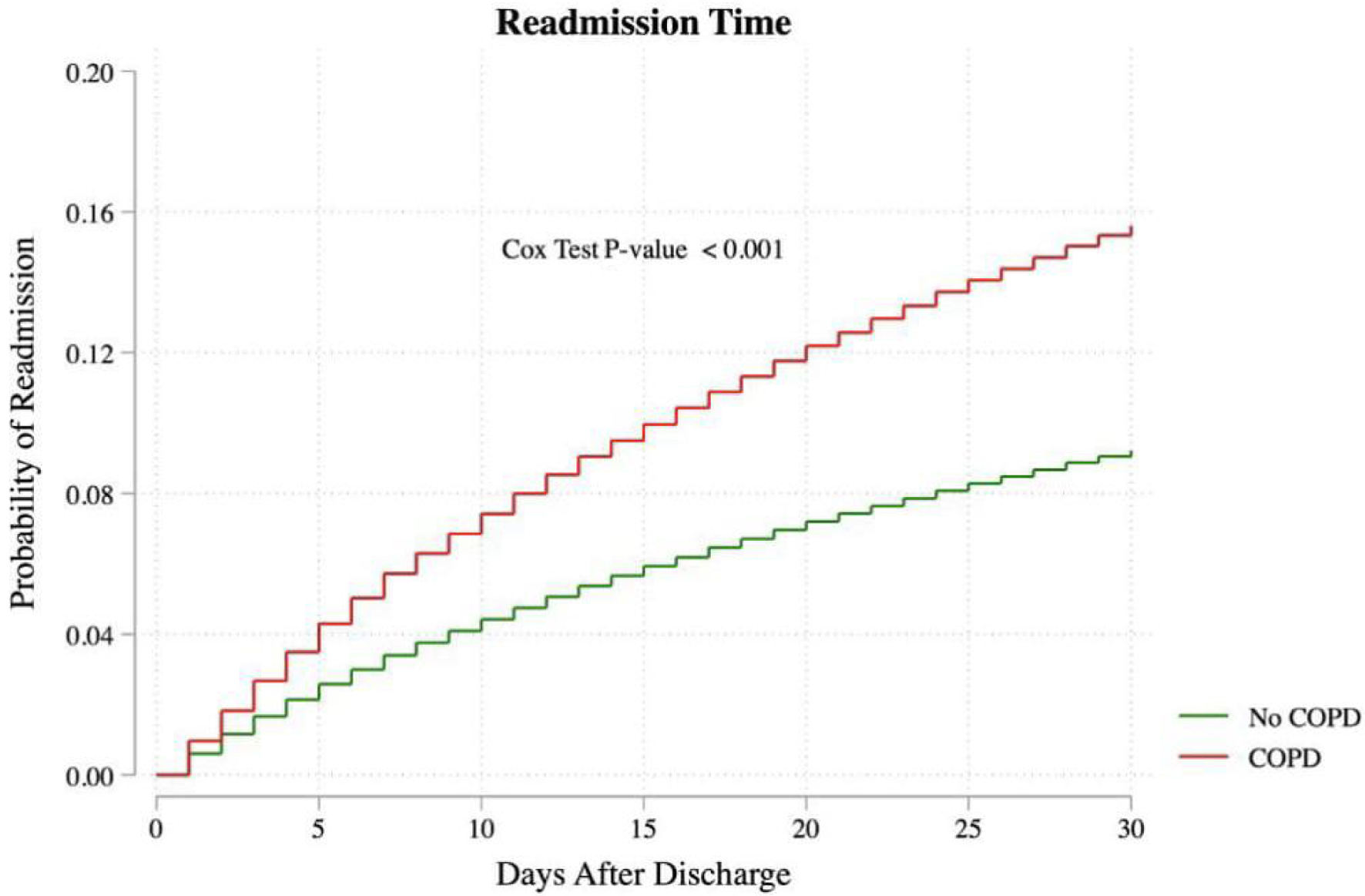 Click for large image | Figure 1. Readmission probability of atrial fibrillation patients based on the status of COPD presence or not. COPD: chronic obstructive pulmonary disease. |
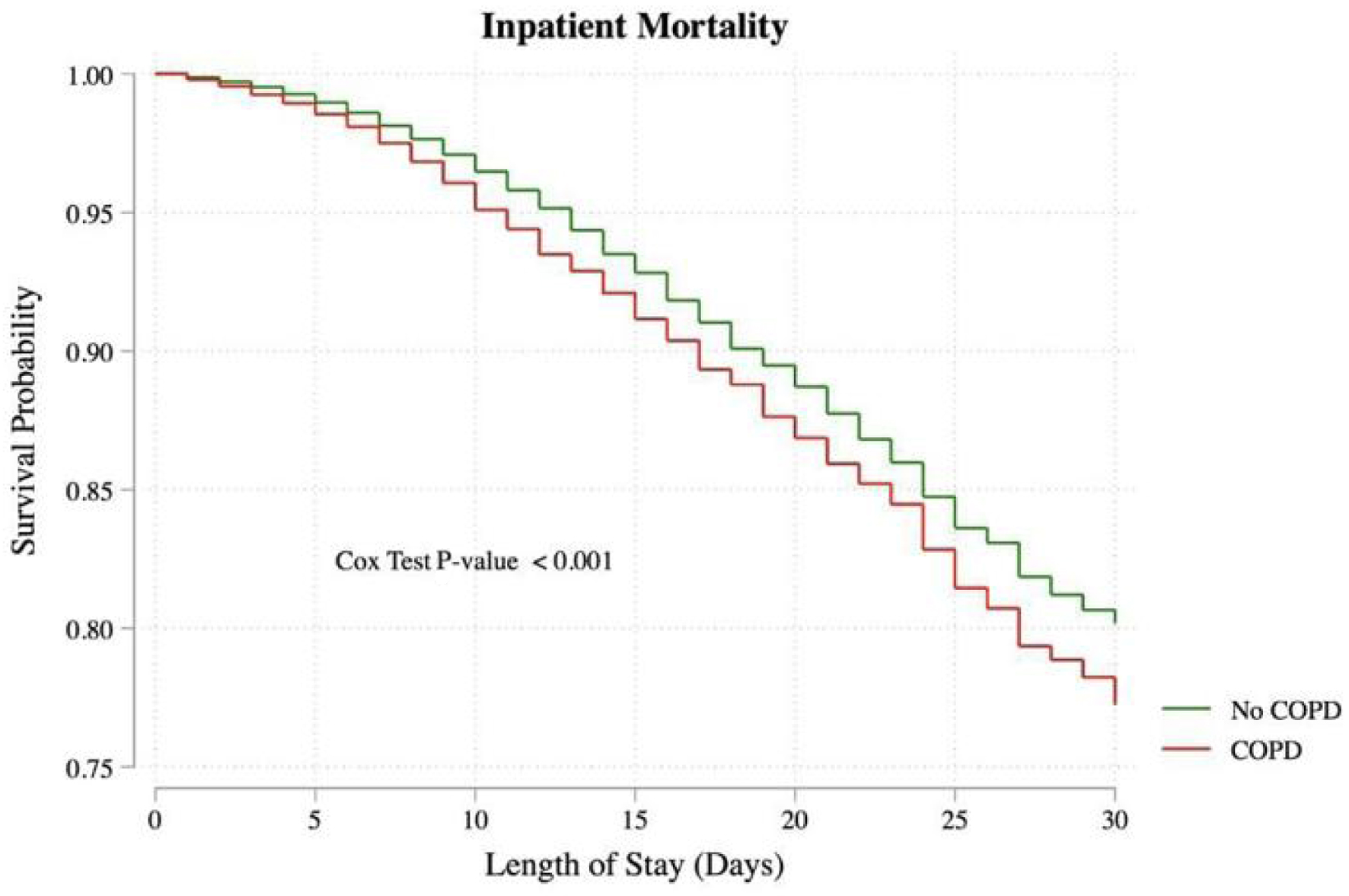 Click for large image | Figure 2. Survival probability of atrial fibrillation patients based on COPD presence. COPD: chronic obstructive pulmonary disease. |
According to Stevenson et al, acute hypercapnia causes structural remodeling and electrical dissociation between muscle bundles, as well as local conduction heterogeneities, which facilitate the onset and maintenance of Afib. This electro-anatomical substrate permits multiple small reentrant circuits that may cause the arrhythmia. They also found that acute hypercapnia alters atrial electrophysiology, not hypoxemia [8, 9]. Simon et al reported that COPD decreases the effectiveness of catheter-based antiarrhythmic therapy, accelerates the course of Afib, and increases the likelihood of Afib recurrence following cardioversion [10]. Our findings are consistent with previous studies that have identified COPD as a predictor of increased readmission rates and mortality in Afib patients. A study of admissions to the Veterans Administration Medical System hospital found that 10.4% of controls and 14.3% of patients with COPD had Afib, similar to our study [11]. Similarly, a retrospective analysis of the NRD for 2016 - 2018, including patients admitted with a diagnosis of Afib who underwent catheter ablation, found that patients with COPD are an independent predictor of readmission and that patients with COPD have a higher risk of readmission [1]. Desai et al stated, using a nationwide database, that arrhythmias were present in 30% of hospitalized COPD patients, with Afib being the most prevalent subtype (22.1%) [12]. The results of this analysis align with our previous findings, which showed a significantly higher risk of readmission in patients with COPD.
Remarkably, our results showed that patients with coexisting Afib and COPD had a shorter LOS than patients without COPD. On the contrary, Desai et al reported a more extended stay among COPD patients presenting with Afib [12]. This could be explained by the higher mortality rate in COPD patients, leading to shorter stays. This finding is noteworthy, considering the higher readmission rates in the COPD group. The need for these patients to continue their treatment at home, early discharge planning tailored for COPD patients, and possibly more aggressive in-hospital management protocols that aim to stabilize them for discharge quickly are some factors that could contribute to a decreased LOS. Westbroek et al stated that tailored discharge planning and home-based care can significantly reduce LO) in patients with COPD [13]. Furthermore, aggressive management strategies, such as the use of integrated care pathways and multidisciplinary team approaches, have been associated with shorter hospital stays and improved management of chronic conditions [14]. Further research is necessary to investigate the underlying reasons for this reduced LOS and to determine whether it has positive or negative implications for long-term patient outcomes. Comprehending these variables may lead to more effective post-discharge care plans and discharge planning, ultimately enhancing the standard of care for patients with Afib and COPD.
Our results are comparable to a study by Wang et al, conducted in 20 Chinese hospitals, which found a high mortality rate for COPD [15]. This emphasizes how severe the impact of COPD is on the prognosis of patients with Afib. The increased mortality rate may be attributed to the compounded stress on the cardiovascular and respiratory systems, which are already compromised in these patients. Moreover, the increased burden of inflammation, hypoxia, and the potential adverse effects of β-agonists and other treatments used for COPD may exacerbate cardiovascular complications. Previous studies have indicated that inflammation plays a critical role in the pathogenesis of both COPD and Afib, potentially leading to worse outcomes when both conditions are present [16, 17]. Furthermore, the presence of COPD can complicate the management of Afib, as certain medications used for rate and rhythm control may not be well tolerated by COPD patients [18]. The need to carefully balance treatments to manage both conditions effectively highlights the importance of integrated care approaches. Our results are summarized in Figure 3.
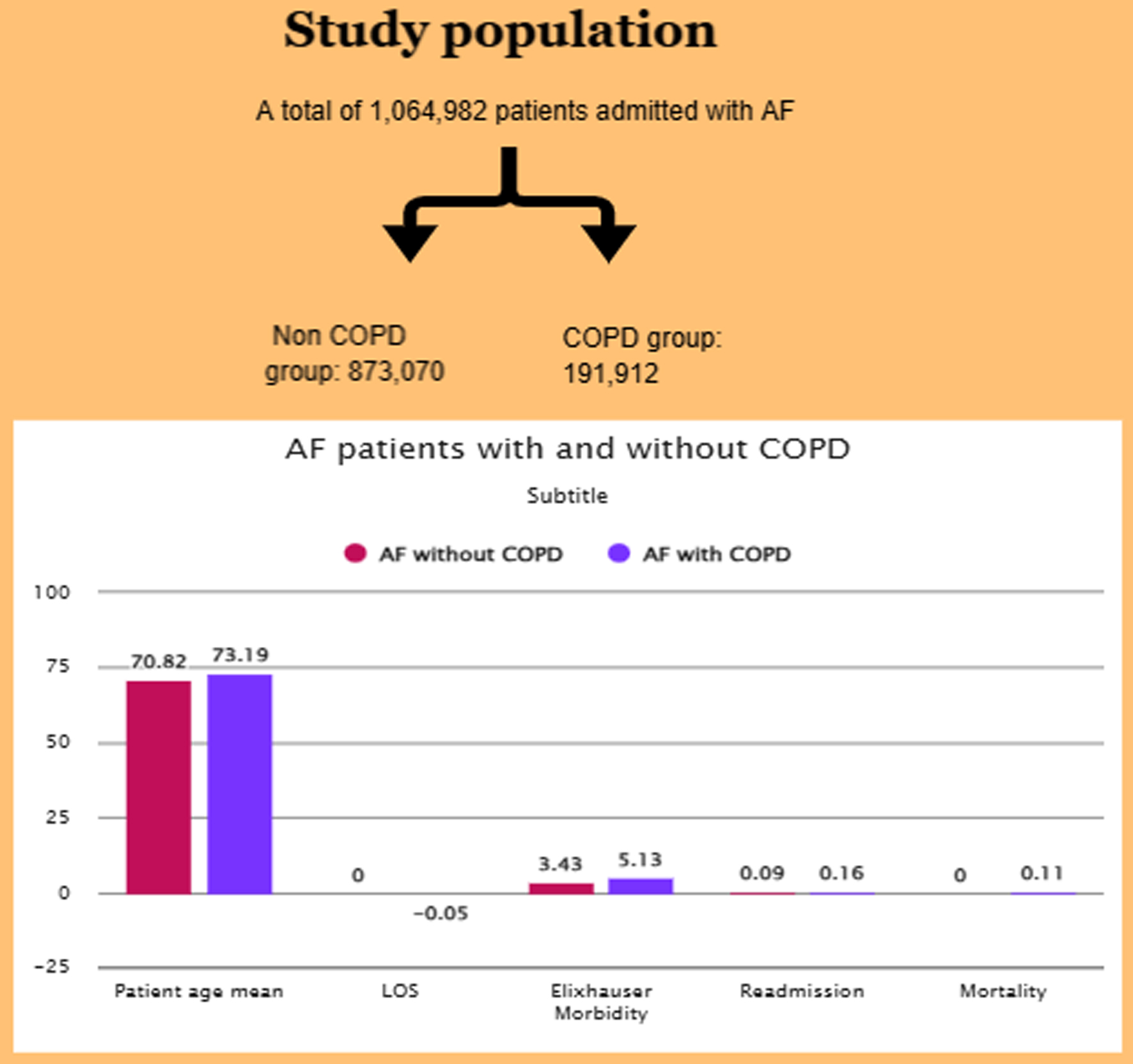 Click for large image | Figure 3. Study results comparing atrial fibrillation in the presence or absence of COPD, analyzing different factors. COPD: chronic obstructive pulmonary disease. |
Our study has several strengths. Including over one million patients enhances the statistical power and generalizability of our findings. Utilizing the NRD provides broad demographic and geographic representation, ensuring external validity. Finally, multivariable regression models accounted for numerous confounders, thereby strengthening the reliability of the observed associations.
Our findings indicate that Afib patients with coexisting COPD had an increased risk for 30-day readmission compared to those without COPD. Therefore, integrated care approaches targeting these two conditions are needed, as multidisciplinary teams that include pulmonologists and cardiologists can be involved in the concomitant management of both conditions. Aggressive management protocols, accompanied by proper follow-up after discharge, can thus be implemented to help reduce the risk of readmissions. Given the heightened 30-day readmission risk observed in patients with both Afib and COPD, targeted interventions may help reduce rehospitalization in this vulnerable population. Integrated disease management programs, particularly those involving multidisciplinary care teams that address cardiac and pulmonary conditions, have shown promise in improving outcomes. Early post-discharge follow-up, ideally within 7 days, can ensure medication reconciliation, symptom monitoring, and timely management of exacerbations. Telemonitoring and remote patient monitoring may offer additional benefits by allowing early detection of arrhythmia recurrence or COPD decompensation. Furthermore, optimizing pharmacologic therapy, such as rate or rhythm control tailored to pulmonary status and the appropriate use of anticoagulation, is essential. Finally, patient education on medication adherence, lifestyle modification, and recognizing warning signs may empower patients and reduce preventable readmissions [19-21].
Future studies should focus on clarifying the mechanisms underlying the dramatically increased rates of readmission and Afib-related mortality in patients with COPD. Furthermore, an area for further research may be the impact of individualized discharge planning and home-based care on long-term outcomes to optimize treatment strategies in this high-risk population.
Limitations
The retrospective design inherently introduces information and selection biases due to historical data, limiting our ability to control for all possible confounding variables. Misclassification or underreporting, particularly with the use of ICD-10 codes in identifying variables, is a limitation when ascertaining the accuracy of our findings. The database may lack key clinical details, such as the severity of COPD, treatment regimens for Afib, and other comorbid conditions, which would provide a better understanding of patient outcomes. The NRD lacks patient-level data on race and ethnicity, as well as medication data, including the use of anticoagulants and other pharmacotherapies relevant to the management of Afib. Administrative data, such as the one we implement here, relies on the healthcare provider’s decision to diagnose COPD or Afib. Therefore, no information is available about the tests used to confirm a disease diagnosis. The study does not account for disease duration, prior treatment, post-discharge management, and follow-up care, which are typically significant factors that impact readmission rates and patient outcomes. While this enhances relevance to the US healthcare system because the population under study is mainly US-based, it might reduce generalizability to other countries with different healthcare infrastructures and a diverse patient mix. These limitations underscore the need for future research to explore these areas in greater detail, thereby enhancing the contextualization of our findings.
Conclusion
Using an extensive national database, our study analyzed data from patients admitted with Afib between 2016 and 2020. We found that Afib patients with COPD had significantly higher odds of 30-day readmissions than those without COPD. However, LOS was shorter for the COPD group, with higher inpatient mortality in patients with COPD.
The findings underscore the substantial impact of COPD on Afib patients, necessitating integrated care approaches and tailored management strategies, including early discharge planning and more aggressive in-hospital management protocols. The increase in in-hospital mortality for Afib patients with COPD highlights the compounded stress on the cardiovascular and respiratory systems in these patients.
Future studies should elucidate the mechanisms underlying the increased readmission and mortality rates and substantiate our findings using administrative data.
| Supplementary Material | ▴Top |
Suppl 1. ICD-10 Codes With Corresponding Diagnoses.
Suppl 2. Basic Characteristics.
Suppl 3. Early Readmission.
Suppl 4. Secondary Endpoints.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
None obtained as the study content originated from a de-identified database.
Author Contributions
SE and FA contributed to methodology; FA and JH contributed to software; GS, PL, and OO contributed to validation; HV, BP, and DS contributed to formal analysis; MA and AM contributed to investigation; SE, FA, and AS contributed to data curation; SE, GS, and AP contributed to the writing of the original draft; SE, JA, JH, and AP contributed to draft editing and reviewing.
Data Availability
All data generated or analyzed during this study are included in this published article and its supplementary information files. Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.
Abbreviations
Afib: atrial fibrillation; COPD: chronic obstructive pulmonary disease; DNR: do not resuscitate; HR: hazard ratio; ICD-10: International Classification of Diseases, Tenth Revision; IQR: interquartile range; LOS: length of stay; NRD: Nationwide Readmissions Database; OR: odds ratio; POA: present on admission; STROBE: Strengthening the Reporting of Observational Studies in Epidemiology
| References | ▴Top |
- Abdullah AS, Eigbire G, Ali M, Awadalla M, Wahab A, Ibrahim H, Salama A, et al. Relationship of atrial fibrillation to outcomes in patients hospitalized for chronic obstructive pulmonary disease exacerbation. J Atr Fibrillation. 2019;12(2):2117.
doi pubmed - Angeli F, Reboldi G, Trapasso M, Aita A, Ambrosio G, Verdecchia P. Detrimental impact of chronic obstructive pulmonary disease in atrial fibrillation: new insights from umbria atrial fibrillation registry. Medicina (Kaunas). 2019;55(7):358.
doi pubmed - Groenewegen A, Zwartkruis VW, Smit LJ, de Boer RA, Rienstra M, Hoes AW, Hollander M, et al. Sex-specific and age-specific incidence of ischaemic heart disease, atrial fibrillation and heart failure in community patients with chronic obstructive pulmonary disease. BMJ Open Respir Res. 2022;9(1):e001307.
doi pubmed - Buch P, Friberg J, Scharling H, Lange P, Prescott E. Reduced lung function and risk of atrial fibrillation in the Copenhagen City Heart Study. Eur Respir J. 2003;21(6):1012-1016.
doi pubmed - Jain A, Arora S, Patel V, Raval M, Modi K, Arora N, Desai R, et al. Etiologies and predictors of 30-day readmission in heart failure: an updated analysis. Int J Heart Fail. 2023;5(3):159-168.
doi pubmed - Scholten M, Davidge J, Agvall B, Halling A. Comorbidities in heart failure patients that predict cardiovascular readmissions within 100 days-An observational study. PLoS One. 2024;19(1):e0296527.
doi pubmed - Li J, Liang L, Cao S, Rong H, Feng L, Zhang D, Chu S, et al. Secular trend and risk factors of 30-day COPD-related readmission in Beijing, China. Sci Rep. 2022;12(1):16589.
doi pubmed - Maraey AM, Maqsood MH, Khalil M, Hashim A, Elzanaty AM, Elsharnoby HR, Elsheikh E, et al. Impact of chronic obstructive pulmonary disease on atrial fibrillation ablation outcomes according to the national readmission database. J Innov Card Rhythm Manag. 2022;13(8):5112-5119.
doi pubmed - Stevenson IH, Roberts-Thomson KC, Kistler PM, Edwards GA, Spence S, Sanders P, Kalman JM. Atrial electrophysiology is altered by acute hypercapnia but not hypoxemia: implications for promotion of atrial fibrillation in pulmonary disease and sleep apnea. Heart Rhythm. 2010;7(9):1263-1270.
doi pubmed - Simons SO, Elliott A, Sastry M, Hendriks JM, Arzt M, Rienstra M, Kalman JM, et al. Chronic obstructive pulmonary disease and atrial fibrillation: an interdisciplinary perspective. Eur Heart J. 2021;42(5):532-540.
doi pubmed - Mapel DW, Dedrick D, Davis K. Trends and cardiovascular co-morbidities of COPD patients in the Veterans Administration Medical System, 1991-1999. COPD. 2005;2(1):35-41.
doi pubmed - Desai R, Patel U, Singh S, Bhuva R, Fong HK, Nunna P, Zalavadia D, et al. The burden and impact of arrhythmia in chronic obstructive pulmonary disease: Insights from the National Inpatient Sample. Int J Cardiol. 2019;281:49-55.
doi pubmed - Westbroek LF, Klijnsma M, Salome P, Sekhuis LM, Rolink E, Korsmit E, Kerstjens HAM, et al. Reducing the number of hospitalization days for COPD: setting up a transmural-care pathway. Int J Chron Obstruct Pulmon Dis. 2020;15:2367-2377.
doi pubmed - Smith SM, Soubhi H, Fortin M, Hudon C, O'Dowd T. Managing patients with multimorbidity: systematic review of interventions in primary care and community settings. BMJ. 2012;345:e5205.
doi pubmed - Wang J, Yang YM, Zhu J, Zhang H, Shao XH, Huang B, Tian L. [Analysis of risk factors for all cause-mortality in Chinese emergency atrial fibrillation patients]. Zhonghua Yi Xue Za Zhi. 2013;93(36):2871-2875.
pubmed - Alfaddagh A, Martin SS, Leucker TM, Michos ED, Blaha MJ, Lowenstein CJ, Jones SR, et al. Inflammation and cardiovascular disease: From mechanisms to therapeutics. Am J Prev Cardiol. 2020;4:100130.
doi pubmed - Barnes PJ. Inflammatory mechanisms in patients with chronic obstructive pulmonary disease. J Allergy Clin Immunol. 2016;138(1):16-27.
doi pubmed - Minor DS, Meyer AM, Long RC, Butler KR, Jr. beta-Blockers and chronic obstructive pulmonary disease: inappropriate avoidance? J Clin Hypertens (Greenwich). 2013;15(12):925-930.
doi pubmed - Press VG, Myers LC, Feemster LC. Preventing COPD readmissions under the hospital readmissions reduction program: How far have we come? Chest. 2021;159(3):996-1006.
doi pubmed - Thomas EE, Taylor ML, Banbury A, Snoswell CL, Haydon HM, Gallegos Rejas VM, Smith AC, et al. Factors influencing the effectiveness of remote patient monitoring interventions: a realist review. BMJ Open. 2021;11(8):e051844.
doi pubmed - Gallagher C, Rowett D, Nyfort-Hansen K, Simmons S, Brooks AG, Moss JR, Middeldorp ME, et al. Patient-centered educational resources for atrial fibrillation. JACC Clin Electrophysiol. 2019;5(10):1101-1114.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.