| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://jocmr.elmerjournals.com |
Review
Volume 17, Number 7, July 2025, pages 365-374
Office-Based Middle Ear Surgery Under Local Anesthesia: A Contemporary Review
Naif Bawazeer
Department of Otolaryngology - Head and Neck Surgery and Ophthalmology, College of Medicine, Umm Al-Qura University, Makkah 21955, Saudi Arabia
Manuscript submitted May 23, 2025, accepted July 9, 2025, published online July 31, 2025
Short title: Office-Based Middle Ear Surgery Under LA
doi: https://doi.org/10.14740/jocmr6279
| Abstract | ▴Top |
Middle ear surgery is a daily routine procedure in otolaryngology. Pain control, along with a bloodless and non-moving operative field during the surgery, is crucial for achieving better surgical outcomes and can be achieved easily under general anesthesia (GA). Nevertheless, local anesthesia (LA), especially if done as office-based surgery, is an ideal alternative to GA in certain scenarios. Despite the well-established nature of LA for middle ear surgery, only a small percentage of otolaryngologists choose to use it, and few publications in the literature address this topic. This article reviews the literature for the feasibility of performing middle ear surgeries in an office base setting. A scoping review of the literature was conducted on middle ear surgery under LA in an office-based setting, focusing on feasibility, advantages, surgical techniques, limitations, and outcomes, to provide a concise guide for its implementation. LA will avoid the rare but serious complications of GA, and there are cost savings of approximately 50% in LA, which is crucial for the sustainability of healthcare systems. It is an ideal alternative to GA in certain scenarios, including decreased access to operative rooms, staff shortage or contraindications for GA. Also, surgeons can appreciate hearing improvement and the need for prosthesis adjustment with instant feedback during the surgery or prevent significant complications such as a dead ear under LA. Office-based surgery for middle ear under LA is feasible and the present work offers a brief guide for beginners with some tips and tricks to ensure optimal patient care and outcomes.
Keywords: Local anesthesia; Middle ear surgery; Office-based surgery; Sedation
| Introduction | ▴Top |
Middle ear surgery is a very frequent part of otolaryngology practice. This term accommodates a wide range of procedures from simple tubes insertion to complex cholesteatoma removal or cochlear implantation, and patients of all ages are affected. Perioperative pain control by anesthesia, along with a bloodless and non-moving operative field during the surgery, is crucial for achieving better surgical outcomes [1]. This can be achieved easily under general anesthesia (GA), and it is the preferred choice for most otologists to perform middle ear surgery, especially in their early career except for myringotomy and tubes insertion [2]. In addition, it is a favorable environment for junior staff to operate in a relaxed manner or to teach residents under supervision, with less stress of sudden patient’s reaction or time needed to finish the procedure [3].
On the other hand, local anesthesia (LA), especially if done as an office-based surgery, could be an ideal alternative for GA in certain scenarios, particularly when tolerance of GA is a concern. For instance, LA is valuable for individuals with significant comorbidities - whether age-related or not - that contraindicate GA, as well as in situations of limited access to operative room or staff shortage in the operating room (OR) from the anesthesiology department [4]. LA will expedite patient management and prevent the accumulation of long waiting lists for the OR. The occurrence of postoperative delirium (PD), as well as postoperative cognitive dysfunction (POCD), is particularly common in elderly individuals following GA, leading to a potential for adverse effects on the overall outcomes, irrespective of the surgical result. These can be also avoided under LA [5, 6].
Despite the well-established nature of LA in middle ear surgery, few publications in the literature address this topic, and only a small percentage of otolaryngologists choose to use it, as the utilization of GA during surgery provides surgeons with a sense of confidence when they perform procedures on crucial structures within the middle ear [7]. According to Yung et al, only 20% of UK otolaryngologists utilize LA for middle ear surgery [4]. Furthermore, the decision to use general anesthetics is largely affected by the patient’s cooperation and anxiety level, which is exacerbated by their hearing loss in ear diseases [7].
Office-based surgery is a growing field that encompasses a wide spectrum of procedures, from brief local anesthetic procedures lasting less than 5 min to complex operations conducted under GA in the presence of a post-anesthesia care unit and anesthesiologist [8]. The literature on office-based procedures primarily comes from the domains of dermatology and plastic surgery, and there is a shortage of precise data about otolaryngology results [9].
This article reviews the literature for the feasibility of performing middle ear surgeries in an office base setting and provides a brief guide for beginners with some tips and tricks to ensure optimal patient care. In this review, we focus on procedures performed under LA without sedation or with only level 1 sedation (anxiolysis), which can be conducted by an otolaryngologist without the involvement of a certified anesthesiologist or the need for advanced patient monitoring that is required when administering significant doses of sedation or GA.
| Methods | ▴Top |
Between January and February of 2025, a scoping review of the literature was conducted through PubMed, Google Scholar, Web of Science and the Cochrane Library. The goal was to identify all articles on middle ear surgery carried out under LA in an office-based setting regarding feasibility, advantages, surgical techniques, limitations, and outcomes. This review included articles that were written in English. The database searches generated a broad search using two combinations by the phrase AND. The terms were: “local anesthesia” OR “office-based” AND “middle ear surgery” OR “Tympanoplasty” OR “Stapedectomy” OR “mastoidectomy”. Articles on simple myringotomy and tube insertion, animal studies, articles published before 1990, articles that required injectable and deep sedation, articles that required non-ontological intervention in office-based surgery, and articles that lacked full-text availability were excluded. A total of 431 individual articles were identified, and a qualitative literature review was synthesized (Fig. 1). Results were reviewed, analyzed, then summarized to provide a concise guide for performing middle ear surgery under LA in an office-based setting.
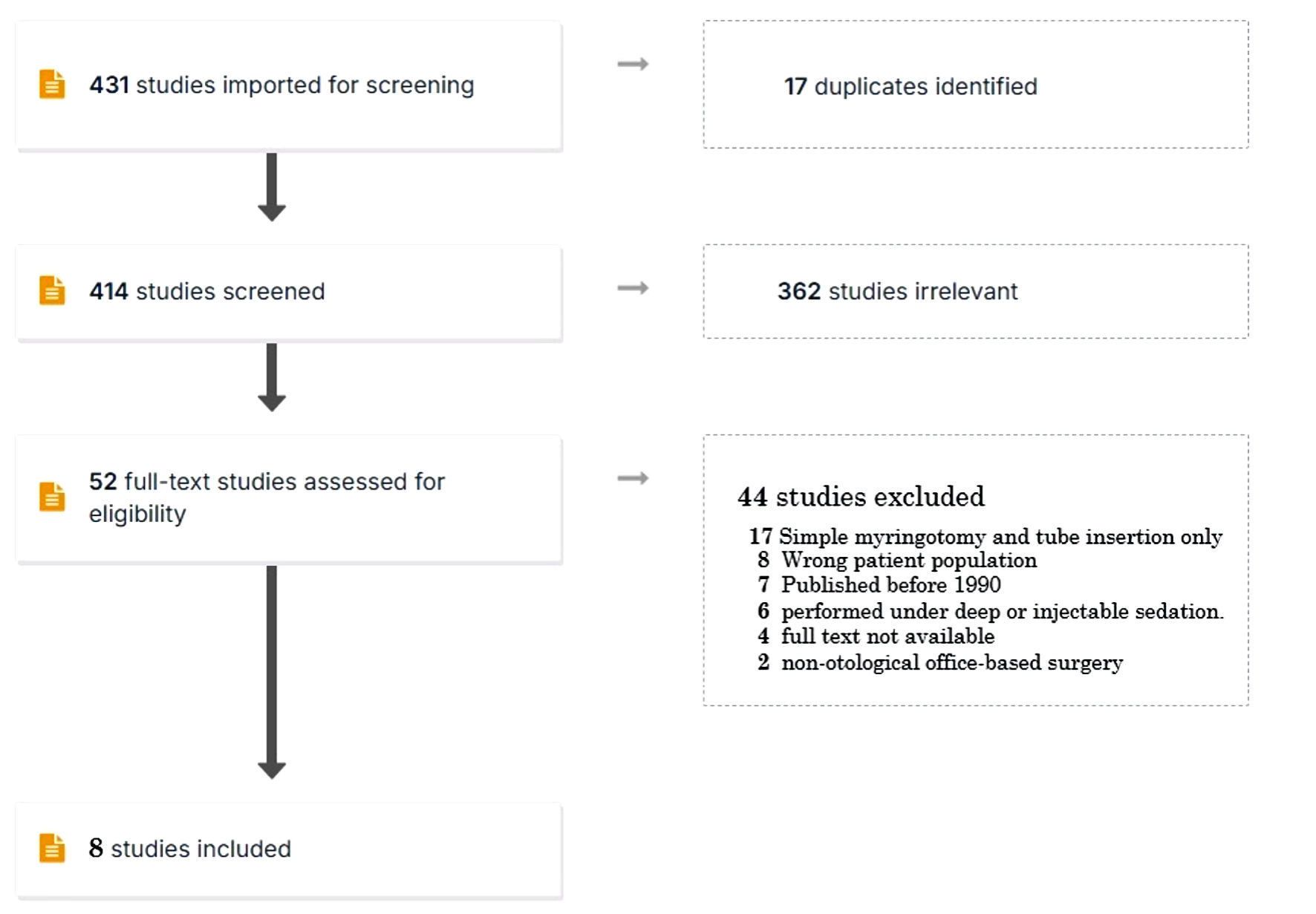 Click for large image | Figure 1. Literature review flow diagram. |
| Discussion | ▴Top |
Advantages of surgery under LA
As is well known by both patient and physician, LA will avoid rare but serious complications of GA, which include aspiration pneumonitis, malignant hyperthermia, respiratory depression, hypoxic brain injury and cardiovascular collapse [10]. Fortunately, it allows more patients to benefit from middle ear surgery that was contraindicated because of their general health, especially in those in need of cochlear implantation. As the population ages and life expectancy increases due to medical advancements, there is a growing indication of cochlear implantation among them [11]. Furthermore, surgeons can appreciate hearing improvement and the need for prosthesis adjustment with instant feedback during the surgery, which theoretically will lead to improved hearing outcomes of the surgery [3]. Similarly, in the case of stapes surgery, patients may experience sudden and intense vertigo, which suggests that the prosthesis is misplaced in the inner ear. The surgeon can take immediate action to prevent significant complications such as a dead ear [2]. Operative time will be surely reduced by eliminating the time of GA induction sequence, which could be sometime longer than expected depending on the patient’s airway. Also, postoperative recovery time and cost will be lower compared to GA, which is crucial for enhancing the sustainability of healthcare systems given the existing limitations on resources. Graff et al [12] reported in a systemic review that compared to GA, local anesthetics can result in cost savings of approximately 50% for surgical procedures. This is mostly due to reduced OR time and post-anesthesia recovery time [12]. Furthermore, unlike procedures performed under GA, most procedures require only one clinical staff member in addition to the surgeon. Long and laborious surgery, especially when associated with drilling and retro auricular approach, raises concerns that patients may not tolerate the noise and discomfort. Although a few articles demonstrate the feasibility of this type of surgery under LA, it is only done with moderate to deep sedation in the OR, with an anesthesiologist always easily reachable if necessary [7, 13].
Combining sedation with LA
Given that sedation - with or without analgesic properties - has an anxiolytic effect, its incorporation into LA during middle ear surgery will enhance patient and surgeon satisfaction [7, 14, 15]. It could be administered orally or by injection (intravenous (IV) or intramuscular (IM)) including midazolam (0.03 mg/kg), promethazine (50 mg IM), fentanyl (2 µg/kg) and pethidine 50 - 100 mg (IM). Injectable routes, particularly IV, are more effective but require advanced equipment and training to monitor patients for signs of toxication, especially respiratory depression, and also the presence of an anesthesiologist in the event of an adverse event. Furthermore, it is important to have easily accessible naloxone at the office for immediate reversal of acute effects [16].
Four levels (stages) of sedation are recognized by the American Society of Anesthesiologists (ASA): GA, deep sedation, moderate sedation (conscious sedation) and minimal sedation (anxiolysis). Level I procedures include minor surgical operations like skin lesion removal carried out under local or topical anesthetic; these procedures do not involve the use of drugs that cause altered consciousness beyond anxiolysis or minimal sedation. Patients under minimal sedation react appropriately to verbal orders when under the influence of drugs. While airway reflexes, cardiovascular and ventilatory systems remain unchanged, intellectual ability and motor coordination may be slightly compromised. Patients undergoing moderate sedation (level II), also known as conscious sedation, consciously respond to verbal commands or gentle tactile stimulation while under the influence of medication. Generally, cardiovascular function remains intact, and no actions are necessary to maintain a patent airway; spontaneous breathing is sufficient [16].
Deep sedation (level III) refers to a state where a patient’s consciousness is significantly reduced because of drugs. In this state, people are not easily awakened but can still respond properly when exposed to painful or repetitive stimulation. There may be a loss of the ability to sustain respiratory function autonomously. Cardiovascular function is often preserved. Patients may need help in keeping their airway patent, and their ability to ventilate spontaneously may not be enough. GA (level IV) is a state of unconsciousness induced by medication, in which patients cannot be stimulated, not even with excruciating stimuli, and the capacity to sustain ventilatory function autonomously is compromised. Patients usually require support in preserving patent airway, and ventilatory support is mandatory due to drug-induced neuromuscular depression. Impairment of cardiovascular function is at risk [16].
Dexmedetomidine is an alpha-2 agonist and one of the sedative medications that has received attention in the literature. It is distinctive in that its effects are not mediated by the gamma aminobutyric (GABA) system; thus, it does not induce respiratory depression [14, 17]. Despite the fact that it induces controlled hypotension, which is advantageous for maintaining a bloodless surgical field, monitoring is necessary to ensure its safe use. When administering sedation to patients with obstructive sleep apnea, extreme caution is required especially with conscious or deep sedation. Patients in this category are particularly sensitive to central nervous system depressant medications, which can induce upper airway obstruction or apnea at low concentrations and elevate the likelihood of perioperative complications [18]. This article primarily discusses procedures that can be performed without the use of sedation or with only minor level 1 sedation, without requiring the presence of an anesthesiologist or advanced equipment. However, conscious and deep sedation are particularly vital for retro-tympanic incision and dissection, along with extensive drilling of the mastoid, such as in tympanomastoidectomy and cochlear implantation [7, 13].
Challenges of surgery under LA
In our opinion, effective communication and coordination between the surgeon and the other clinic staff are critical to the surgery’s success and contribute to the overall patient experience. This coordination is particularly difficult to achieve at the start of the surgery implementation under LA and necessitates time and practice to establish. An uncoordinated team that performs the procedure in front of the patient will amplify the patient’s anxiety and pain threshold while also making the intervention more difficult for the surgeon. Moreover, it can be difficult sometimes to maintain the head and body in the appropriate position for ear surgery in awake patients, particularly in patients who are elderly or have cervical issues.
Noise and vibration are significant concerns that arise during surgical procedures which can trigger anxiety and increase pain threshold of the patient, particularly during drilling [7, 13]. The patients who reported these issues in the aforementioned articles had moderate to profound hearing loss and underwent cochlear implantation. Consequently, patients with mild to moderate hearing loss (chronic otitis media with preserved inner ear hearing) will therefore be more significantly affected by drilling. Thus, in our experience, we recommend avoiding drilling or using large size suction throughout the procedure to increase patient tolerance and avoid unpleasant experiences, especially in the absence of conscious or deep sedation. The potential for sudden rotatory vertigo to occur in the patient is another frustrating side effect of LA. This can occur when the anesthetic diffuses in the middle ear and contacts the inner ear, particularly in the case of a tympanic membrane rupture, and can last for several minutes to hours [19]. Also, middle ear surgery is associated with a high incidence of postoperative nausea and vomiting (PONV). Prophylactic administration of antiemetic medication is necessary to reduce the incidence of PONV, as 62% to 80% of patients will be affected in the absence of antiemetic treatment [20]. Furthermore, when there is bleeding in the operating field during middle ear surgery, anatomical landmark identification may be difficult, and the likelihood of cholesteatoma recurrence is increased. Vessel tone, arterial pressure, and venous pressure significantly influence the extent of bleeding that obscures the surgical field, because the microvasculature is the primary cause of bleeding in the middle ear. This is easily controlled when the patient undergoes surgery under GA [21].
One of the feared adverse effects associated with sedatives is oversedation, which can result in respiratory depression due to a diminished response of ventilation to hypercarbia. Complex challenges are presented by this condition under LA, including rapid desaturation, mask ventilation difficulties, the need of an anesthesiologist and orotracheal intubation struggles [22]. Also, surgeon must keep in mind that particular groups of patients, including African Americans and individuals with red hair, appear to be more pain-sensitive and require greater doses of anesthetics to obtain comparable levels of anesthesia. However, this comes with an increased risk of adverse effects related to LA [23].
In their systematic study, Wegner et al found no significant difference in postoperative hearing outcomes between patients who underwent stapedectomy under LA and those who underwent it under GA, despite the potential advantages of adjusting prostheses based on the patient’s subjective perception of hearing during the surgery. Although there was a considerable risk of bias in this article [3].
In the pediatric population, LA is primarily employed in middle ear surgery for simple myringotomy with ventilation tube insertion, given children’s intolerance to noise, pressure fluctuations in the middle ear, prolonged positioning, and anxiety. Consequently, complex or multi-step procedures involving the elevation of the tympanomeatal flap are rarely done among this age group [24, 25].
Points of interest in LA
Infiltrative LA is safe and commonly used in many specialties, including ear, nose, and throat (ENT), dentistry, plastic surgery, ophthalmology, and especially in office-based dermatologic surgery [26]. Some examples of amide anesthetics are lidocaine, which has an onset of action of less than 1 min and a duration of action of 30 to 120 min without epinephrine, or 60 to 400 min with epinephrine, as well as bupivacaine and mepivacaine. Procaine and tetracaine are examples of ester anesthetics [27]. The highest suggested doses of lidocaine with epinephrine and lidocaine without epinephrine for local infiltration in adults are 7 mg/kg and 4.5 mg/kg, respectively, as stated by the manufacturer. While in pediatric patients, the administration of lidocaine with epinephrine at a dosage of 3.0 to 4.5 mg/kg and lidocaine without epinephrine at a dosage of 1.5 to 2.0 mg/kg is considered safe [26]. Pain during infiltration appears to be reduced when a warm (40 °C) solution is utilized in conjunction with slow-paced infiltration, according to Scarfone et al [28]. The incidence of lidocaine allergy is uncommon, with a real immunologic response accounting for only 1% of adverse reactions cases [29]. In that scenario, a possible alternative is to change to an ester-based local anesthetic, considering that the occurrence of cross-reaction between the two types is rare. A different option is utilizing bacteriostatic saline, which consists of 0.9% benzyl alcohol in normal saline. This solution has demonstrated effectiveness in dermatological treatments. However, there is currently no documented evidence about its efficacy in otological procedures [26, 30]. The iontophoresis system is a distinctive technique for anesthetizing the external auditory canal and tympanic membrane, by employing a low electrical current to facilitate the transdermal delivery of an ionized mixture of lidocaine and epinephrine into the tissues. This technique provides better LA within 10 min with a particular earplug that eliminates the need for needle injection [25].
Lidocaine is classified as a pregnancy category B medication by the Food and Drug Administration (FDA). This classification, along with other supporting evidence, establishes its safety for local injection in small quantities throughout pregnancy. However, it is crucial to avoid it during the initial 10 weeks of pregnancy due to the heightened teratogenic risk [31]. Furthermore, the American Academy of Pediatrics has determined that lidocaine is acceptable with lactation. However, some preservatives, which are required to be added to local anesthetics containing epinephrine, may induce adverse reactions in neonates [32].
Epinephrine used in conjunction with infiltrative local anesthetic has been proven to extend anesthesia duration and decrease bleeding during the course of surgery. Several randomized controlled trials and systematic reviews have concluded that adding epinephrine to local infiltrative anesthetic is a safe practice for ear surgery [7, 33]. This addition does not pose any risk of necrosis for the ear or even dermatological procedure on the penis, as previously believed, even if the skin area involved is supplied by terminal blood vessels [34]. In dental surgery, the safety of administering epinephrine with local infiltrative anesthesia in modest volumes (1.8 to 3.6 mL) has been established for patients with stable cardiac disease. Conditions considered to represent stable cardiac disease include arrhythmia, ischemic heart disease, chronic coronary disease, and hypertension. Nevertheless, in cases where patients with unstable cardiac conditions require higher doses of LA (with epinephrine) for surgery, it is imperative to consult with their cardiologist prior to the procedure [35]. Although epinephrine is categorized as a pregnancy category C substance by the FDA, it appears to be safe for administration in small doses to pregnant women when combined with local infiltrative anesthesia. Still, clinicians should delay non-emergency procedures that necessitate local infiltration anesthesia until after delivery to prevent potential complications. Delaying urgent surgery till at least the beginning of the second trimester is advised, if feasible [36].
Local anesthetic systemic toxicity (LAST) is an uncommon incident, yet it can have severe and catastrophic consequences. The symptoms and signs of LAST are gradual and consist of tingling sensations in the face, numbness around the mouth, a metallic taste in the mouth, difficulty speaking clearly, audio-visual disturbances and an increased heart rate or high blood pressure. As the situation progresses, there is an increased risk of triggering central nervous system depression, seizures or cardiac rhythm disturbance occurring, and cardiopulmonary failure or arrest may result from severe cases [37]. Following the cessation of LA injection, immediate management involves performing resuscitation steps to ensure the maintenance of the airway, breathing, and circulation, in accordance with the Basic Life Support algorithms. Benzodiazepines are the recommended initial treatment for seizure activity due to their cardiostable properties. Administration of 20% IV lipid emulsion therapy can effectively transport any LA drug from organs with high blood flow such the heart to organs responsible for storage such as muscles. This process ultimately enhances the overall outcomes [38]. To minimize the risk of LAST, aspiration prior to injection is recommended to prevent intravascular injection; accurate positioning of the needle and dosage restriction to safe levels are recommended.
Key points of office-based surgery
Office-based surgery, as per its definition, refers to non-emergent or not a life-threatening procedure conducted in a setting other than a hospital or ambulatory surgery center. These surgeries should not cause a patient to lose more than 10% of their estimated blood volume, assuming their hemoglobin levels are normal. Additionally, the duration of the surgery should be less than 6 h and should exclude significant intracranial, intrathoracic, or intra-abdominal operations [8]. A mortality rate of 1 in 57,000 patients was established in 1997 by Morello et al among more than 400,000 office-based plastic surgery operations, which was documented in their series. GA administration and surgical participation by unqualified personnel further contribute to the exacerbation of this rate [9]. Other factors that affected the outcomes in case of complications during the office-based surgery include improper airway supplies and drugs for resuscitation, absence of established emergency protocols to follow (or they are not implemented correctly), and insufficient availability of transfer agreements for emergency care with nearby hospitals [8].
In order to optimize outcomes in the event of complications such as allergic reactions, toxicity, cardiac arrest, electrical failures, or fire emergencies, it is critical to have a concise written manual that outlines the necessary actions to be taken by the medical staff. For example, in Florida, all surgeons performing level II and III office-based surgery are obligated to complete Advanced Cardiovascular Life Support (ACLS) training, and another assistant staff member certified in Basic Life Support. According to the ASA, it is essential for all facilities to provide a dependable supply of oxygen, resuscitation supplies, suction, and emergency medications as a bare minimum requirement [39, 40]. Furthermore, offices that perform LA are advised by the American Society of Regional Anesthesia and Pain Management to keep a rescue kit for LAST on hand. A printed checklist for LAST, 1 L (total) of 20% lipid emulsion, IV tubes, and multiple catheters and syringes for rapid infusion should be included in this kit. Establishing a precise protocol for evaluation and management of LA toxicity is critical for all medical offices that perform office-based procedures [16].
The practice of office-based surgery has expanded due to its advantages, which include decreased expenses of medical care compared to regular hospital, more control over surgical planning and access by the surgeon, and more patient privacy. An estimated 10-15% of all surgeries are conducted as an office-based surgery nowadays [8, 40]. The majority of the literature that demonstrates feasibility, safety and outcomes is from plastic and dermatological specialties, and there are limited reports on the efficacy and safety of office-based surgery in otolaryngology. These reports indicate that office-based surgery in otolaryngology is feasible with acceptable risks and complications. However, further study is required to draw an accurate conclusion [41, 42]. It is important to bear in mind that in middle ear office-based surgery, the use of a small amount of LA with or without minimal oral sedatives, eliminates a significant portion of the negative outcomes associated with office-based surgery complications and emergencies discussed in the literature, as well as improving its safety profile, in contrast to risks related to the use of GA and strong sedatives during elaborative surgery in other surgery.
How the surgery will go under LA
The successful outcome of local anesthetic operations depends on several factors, including effective preoperative counseling, careful patient selection, and optimal sedation administration [13]. Patients who are naturally anxious are not suitable candidates for LA intervention, as they frequently exaggerate their perception of noise and pressure sensations as painful sensations, regardless of the effectiveness of LA. We offer each patient a minimal oral sedation of 1 mg of lorazepam 1 h prior to the surgery, particularly if the patient reveals signs of anxiety upon admission. Stronger sedation can be administered through a higher dose or by an IV route to improve patient pain control, but it comes at the cost of requiring advanced equipment and expertise to monitor patients for signs of toxication.
Turnover between cases will be accelerated, and efficacy improved by preparing the surgical instruments and materials for the entire patient list either early in the morning or one night before the day of surgery. To optimize time, it is recommended that the otolaryngologist be accompanied by one nurse and one clinic personnel. Upon admission and prior to discharge, the clinic personnel will verify the patient’s file, discharge papers, and appointment following the surgery. The nurse is responsible for the following tasks: preparing the surgical table, installing the patient in the OR, recording vital signs through intermittent monitoring (heart rate (HR), blood pressure (BP), and peripheral capillary oxygen saturation (SO2)), and assisting the surgeon during the surgery if the patient requires repositioning or an additional surgical instrument.
Upon the patient’s arrival, it is mandatory for a member of the clinic staff to conduct a quick review of his identification, diagnosis, and the surgical procedure that has been planned for him, including the operative side. Additionally, this individual is responsible for verifying the completeness of the patient’s medical dossiers, which includes medical records, images, an audiogram, and consent for the surgery. It is essential to offer a clear overview of the experiences that a patient will encounter and address any concerns they may have in order to reduce their anxiety. Following this, the patient must change into a surgical gown and remove any accessories, particularly metallic objects or hearing aids, to prevent any potential injuries if monopolar is used. Next, the nurse will accompany the patient to the OR and verify his identification, surgical details, and any allergies or contraindications. The patient will then lie down on the operating table or a manipulable medical stretcher. The nurse will take the first reading of the patient’s vital signs, and the monitor will remain connected to the patient to alert the team in case of any disruptions in vital signs. Figure 2 depicts an ergonomic configuration of an OR, designed to enable the surgeon to perform procedures in the ear independently. In order to enhance the visibility of the middle ear, the patient should lie flat without any elevation under their head, tilting their head to the opposite side and their chin to their chest as shown in Figure 3. Occasionally, support may be needed on the opposite side of the face to reduce postoperative pain from this position.
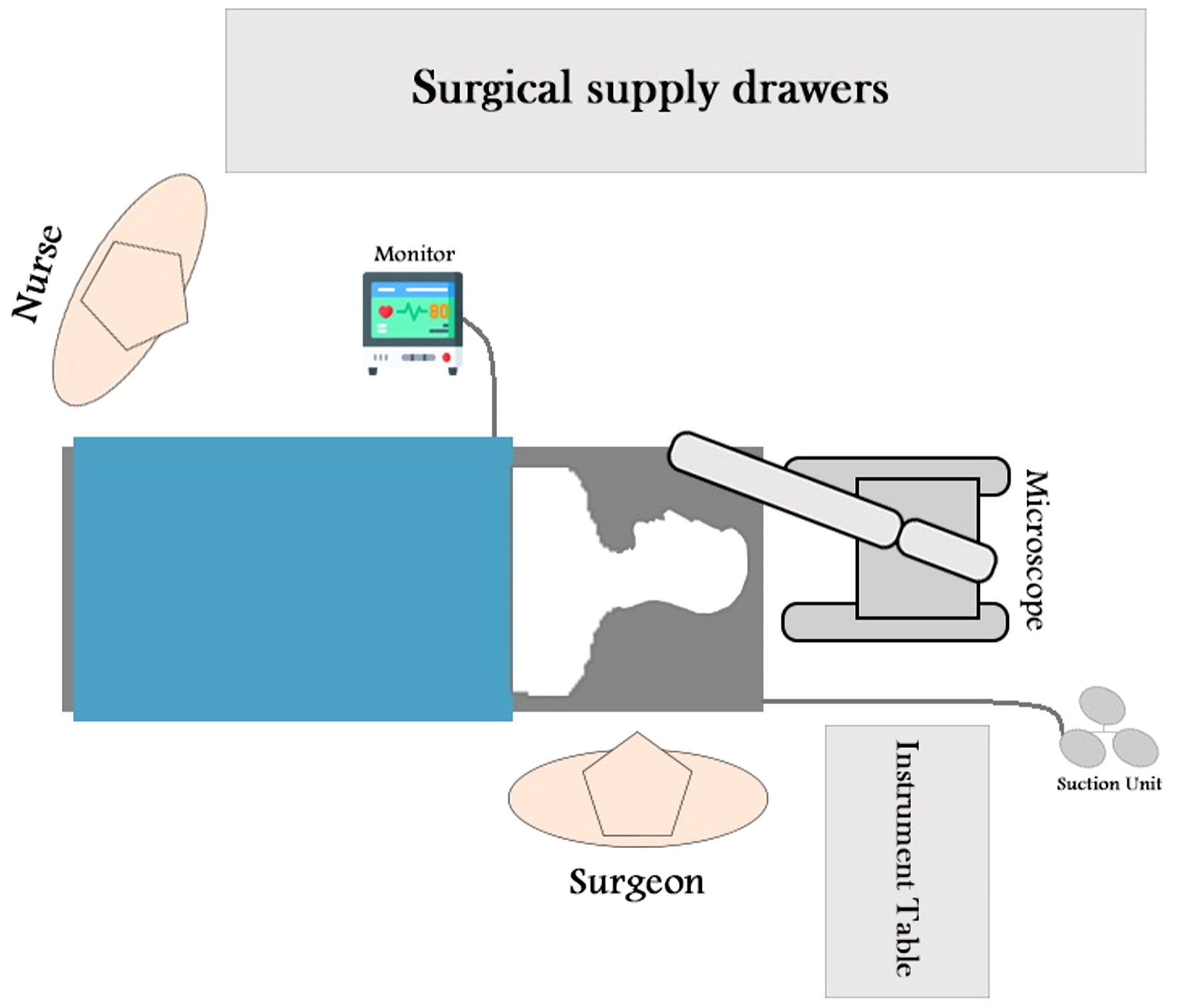 Click for large image | Figure 2. Ergonomic configuration of an operating room, designed to enable the surgeon to perform procedures in the ear independently. |
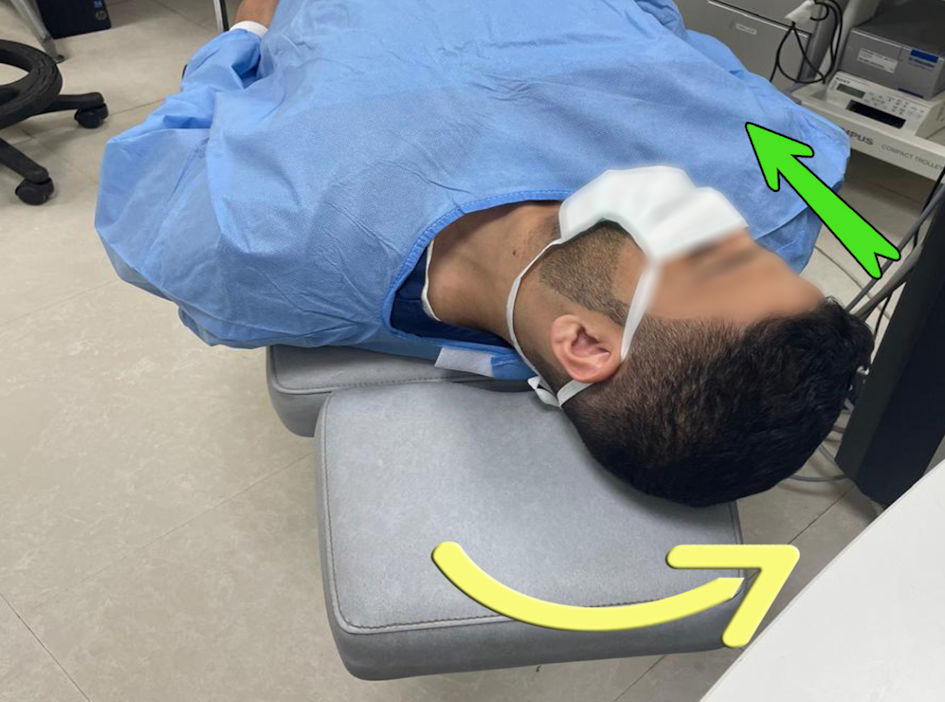 Click for large image | Figure 3. The patient is in a flat position with no elevation under the head, with the head tilted to the opposite side (yellow arrow) and the chin into their chest (green arrow) to improve the visibility of the middle ear. |
Once the surgical disinfectant has been applied to the ear, the surgeon can proceed with infiltrating the ear and the tragal cartilage’s front and back skin, if necessary, to get cartilage material or perichondrium, as depicted in Figure 4. The infiltration of the external auditory canal can be improved by bending the metallic segment of the needle laterally, as the created angle permits proper bone contact, as seen in the previous figure. The medical staff needs to remind the patient that local anesthetics provide analgesic effects but do not eradicate tactile sensations and noise in the infiltrated region. As a result, individuals may still experience feelings of tissue manipulation and noises from equipment, but without any feeling of pain. In addition, the surgeon must ensure that the innermost section of the outer ear and the eardrum are properly anesthetized before elevating the tympanomeatal flap. This is important because any additional anesthesia that is required after that can leak through the incision, making it challenging to re-anesthetize the deep part. This is likely to complicate the procedure due to the patient’s discomfort. Finally, when infiltrating the ear with tympanic membrane perforation, surgeons must ensure that the anesthetic remains within the subdermal layer with bone contact, and suction should be maintained in the other hand to aspirate any droplets that leak from the injection site before they reach the inner ear. This creates a passage for lidocaine to directly contact the inner ear, resulting in a strong episode of rotatory vertigo that can last from minutes to hours. Similarly, when infiltrating the external ear without tympanic perforation, the surgeon must observe the whitish discoloration of the skin and cease infiltration when it reaches the tympanic membrane. Excessive infiltration will result in the extravasation of anesthetic into the middle ear and, subsequently, the inner ear, causing rotatory vertigo. Furthermore, great analgesic effects can be obtained through the blocking of the great auricular nerve branches, notably through retroauricular infiltration, alongside the tympanic branch of the auriculotemporal nerve if needed. Mastoid bone and air cells lack sensory perception, except for the external periosteum and to some extent, the interior mucoperiosteum, which could clarify why the patient has a painless mastoid drilling experience [7].
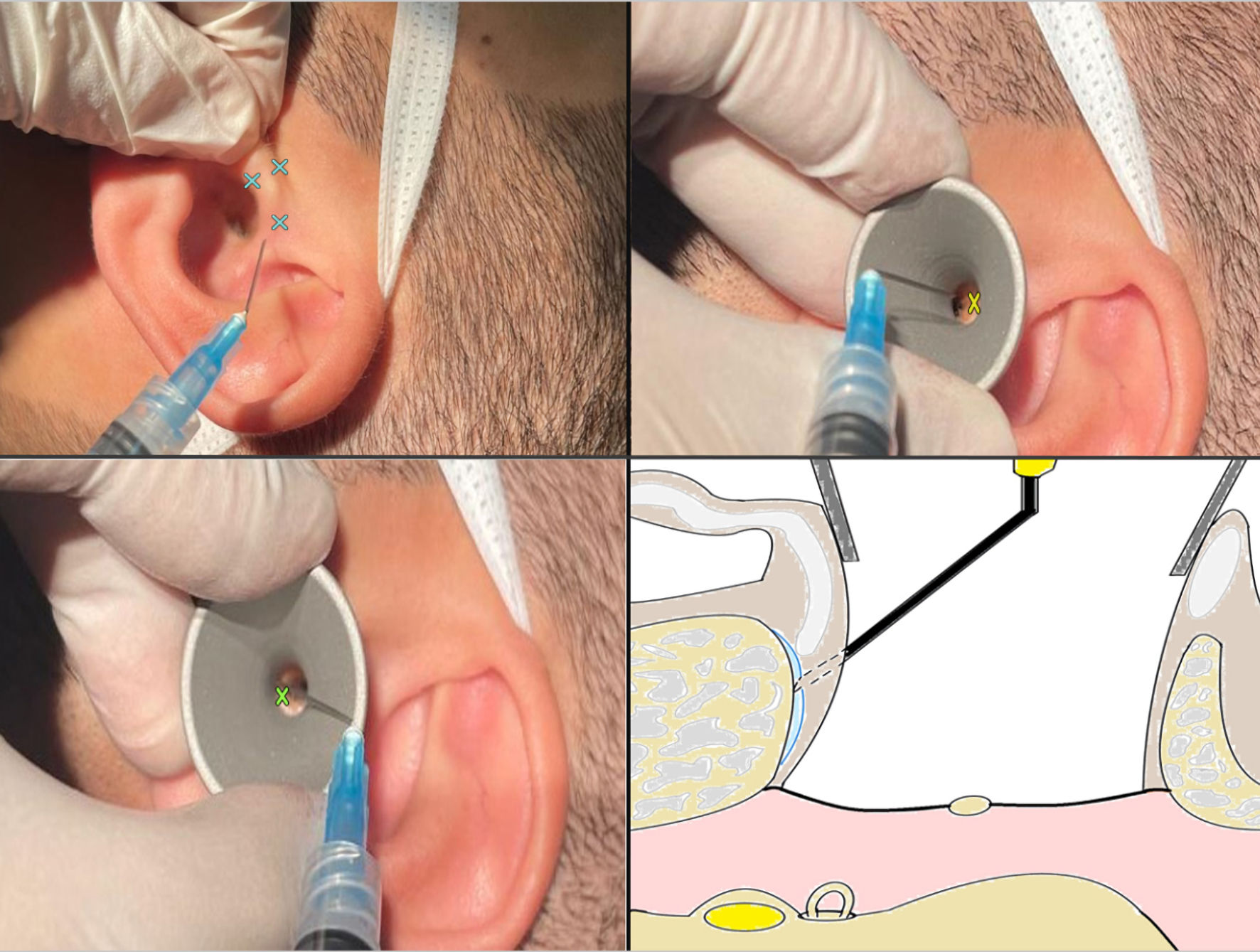 Click for large image | Figure 4. Tragal cartilage and the external auditory canal infiltration sites (cross marks). The metallic segment of the needle can be bent laterally to provide correct bone contact. Top left: tragal cartilage infiltration sites. Top right: superior part of the external auditory canal infiltration site. Bottom left: inferior part of the external auditory canal infiltration site. Bottom right: correct infiltration depth, the metallic segment of the needle should be bent laterally to ensure proper bone contact. |
It is advised to harvest the cartilage or perichondrium of the tragus first to allow the perichondrium to dry correctly on the table and be utilized effectively in the subsequent reconstruction. Following this, the surgeon can elevate the tympanomeatal flap to gain access to the middle ear and perform the intended procedure. Smaller diameter suction is recommended as the instruments approach the inner ear to prevent the patient from experiencing noise discomfort. It is critical that the patient be guided through each stage of the surgical procedure to prevent any unexpected surprises that could move abruptly the surgical fields, which could be problematic. As the final step of the surgery, the external auditory canal may be packed with Gelfoam or Otowick with antibiotic ointment, and a simple small square dressing is applied over the external auditory meatus, based upon the surgeon’s preferences.
Despite the mandatory disinfection of the office’s operating area between patients, it is less effective when compared to the hospital’s OR. Additionally, the ventilation system is different. For these reasons, we recommend administering prophylactic oral antibiotics, such as the first generation cephalosporins like cefadroxil, during the postoperative period. Although this practice is highly controversial, there is currently no available evidence in the literature to guide what should be decided. To prevent caloric reactions during surgical field washing or drilling if needed, it is critical to warm the irrigation fluid of the ear drill using an infusion warming system. Transient facial weakness related to anesthetic encountering dehiscence nerve is not an uncommon finding after the surgery and typically has no consequential adverse effects [43]. The surgeon must reassure the patient about this transit adverse effect. Physical and pharmacological techniques are employed to achieve a bloodless surgical field, such as a 15° - 20° head-up tilt, prevention of venous obstruction, normocapnia, and blood pressure reduction. A forced air device may be utilized to offer air room ventilation, while transparent plastic drapes may be utilized to alleviate claustrophobia sensation.
During the procedure, the author believes that engaging in simple conversation with the patient, whether it be by the assistant nurse, surgeon, or a family member, is extremely beneficial in providing the patient with a sense of reassurance. This is believed to unconsciously reduce the patient’s pain threshold and anxiety, resulting in better patient experience and tolerance. Mild and predictable movement of the surgical field may occur when the patient speaks, but it is easily manageable, unlike an anxious patient unable to tolerate the surgery.
The patient’s vital signs are recorded for the last two times after the surgery, with a 5-min interval between each reading. The patient is then discharged if he is asymptomatic after being kept under simple surveillance for 20 - 30 min without vital sign monitoring. Dimenhydrinate (Gravol) 50 mg suppository is administered in the event of vertigo, nausea and vomiting, and it may be administered again within 30 min. The duration of time required for symptom resolution depends on the amount of local anesthetic that reaches the inner ear, which can range from 1 h to 6 h. Even though it is uncommon, it is important to be prepared for prolonged observation in the office or even a transfer to a nearby health facility’s observation room, particularly with the last case of the operating list. In our opinion, it is advisable to start the operating list with tympanic membrane perforation cases, as rotatory vertigo is more frequent in these cases. It is crucial to allocate sufficient time to monitor and provide care for these patients until the vertigo attack has resolved. This can result in prolonged hours for the clinic staff if not properly planned, and it can pose a problem if it occurs by the end of the day, as vertigo attacks may persist for as much as 5 to 6 h. Medical office staff, particularly otolaryngologists, require the competence to identify and effectively manage any potential allergic reactions and local anesthetic toxicity. In case of any use of sedation, surgeons must be familiarized with practicing the Guidelines for Sedation and Analgesia by Non-Anesthesiologists, which was issued by the ASA in 2002 [44]. Saliba et al, Shoman et al, and Monfared et al published a remarkable series of tympanoplasties and ossiculoplasties carried under LA without sedation, proving the procedure’s feasibility and resulting in excellent patient outcomes [45-47]. Similarly, uncomplicated tympanoplasty operations under pure LA without tympanomeatal flap dissection have been documented in three studies in the literature with satisfactory outcomes [47-49]. Furthermore, Shoman et al described another small series of office-based ossiculoplasty with tympanomeatal flap and ossicles manipulation [50]. Lastly, Neumann et al reported a series of five patients who successfully underwent mastoidectomy under LA for chronic otitis media, despite having severe contraindications for GA and sedation [51].
| Conclusions | ▴Top |
Office-based surgery for middle ear under LA is feasible and presents an ideal alternative for GA in certain scenarios, including decreased access to operative room, staff shortage or contraindication for GA. Also, surgeons can appreciate hearing improvement and the need for prosthesis adjustment with instant feedback during the surgery. Furthermore, there are cost savings of approximately 50% in LA, which is crucial for the sustainability of healthcare systems. However, it is imperative that otologists be prepared for the rare but serious adverse effects of LA. According to the author’s experience and current trends in published literature, myringotomy and tympanoplasty without tympanomeatal flap elevation (as in butterfly tympanoplasty) represent ideal candidates for office-based surgery. However, as experience builds, tympanoplasty with tympanomeatal flap elevation (as in the underlay technique) and ossiculoplasty will be a more feasible and ideal indication. However, middle ear procedures involving drilling and extended dissection are not recommended unless deep sedation is provided in the main OR.
There is a scarcity of long-term outcome data and large-scale comparative studies. It is desirable to accumulate evidence through prospective research and multicenter collaborative investigations in the future. Moreover, it is essential to elucidate and standardize the surgical indications for office-based middle ear surgery, which remain ambiguous; hence, future research should concentrate on this domain. Indications should take into account factors such as patient cooperation, anxiety levels, and hearing levels. A brief guide for beginners with some tips and tricks to ensure optimal patient care and outcome was presented in this work.
Acknowledgments
The author is grateful to Prof. Issam Saliba MD, FRCSC (University of Montreal Hospital Centre), a pioneer in middle ear surgery under LA. Additionally, the author extends his appreciation to Dr. Faisal Swead for his participation as a model in the figures.
Financial Disclosure
The work was not supported or funded by any companies or third party.
Conflict of Interest
Author has no conflict of interest to declare.
Author Contributions
The author has contributed to, read, and approved this manuscript.
Data Availability
The author declares that data supporting the findings of this study are available within the article.
| References | ▴Top |
- Smith RL, Ward PA. Anaesthesia for ear surgery. Anaesthesia & Intensive Care Medicine. 2023;24(3):200-206.
- Liang S, Irwin MG. Review of anesthesia for middle ear surgery. Anesthesiol Clin. 2010;28(3):519-528.
doi pubmed - Wegner I, Bittermann AJ, Zinsmeester MM, van der Heijden GJ, Grolman W. Local versus general anesthesia in stapes surgery for otosclerosis: a systematic review of the evidence. Otolaryngol Head Neck Surg. 2013;149(3):360-365.
doi pubmed - Yung MW. Local anaesthesia in middle ear surgery: survey of patients and surgeons. Clin Otolaryngol Allied Sci. 1996;21(5):404-408.
doi pubmed - Strom C, Rasmussen LS, Sieber FE. Should general anaesthesia be avoided in the elderly? Anaesthesia. 2014;69(Suppl 1):35-44.
doi pubmed - Strom C, Rasmussen LS. Challenges in anaesthesia for elderly. Singapore Dent J. 2014;35C:23-29.
doi pubmed - Dietz A, Lenarz T. Cochlear implantation under local anesthesia in 117 cases: patients' subjective experience and outcomes. Eur Arch Otorhinolaryngol. 2022;279(7):3379-3385.
doi pubmed - Hector V, Desai MS, Miguel RV. Office-based anesthesia. Handbook of Ambulatory Anesthesia. 2008:283-324.
- Morello DC, Colon GA, Fredricks S, Iverson RE, Singer R. Patient safety in accredited office surgical facilities. Plast Reconstr Surg. 1997;99(6):1496-1500.
pubmed - Harris M, Chung F. Complications of general anesthesia. Clin Plast Surg. 2013;40(4):503-513.
doi pubmed - Yang Z, Cosetti M. Safety and outcomes of cochlear implantation in the elderly: A review of recent literature. J Otol. 2016;11(1):1-6.
doi pubmed - Graff V, Gabutti L, Treglia G, Pascale M, Anselmi L, Cafarotti S, La Regina D, et al. Perioperative costs of local or regional anesthesia versus general anesthesia in the outpatient setting: a systematic review of recent literature. Braz J Anesthesiol. 2023;73(3):316-339.
doi pubmed - Sarmento KM, Jr., Tomita S. Retroauricular tympanoplasty and tympanomastoidectomy under local anesthesia and sedation. Acta Otolaryngol. 2009;129(7):726-728.
doi pubmed - Kulkarni TM. A comparison of three drug combinations for sedation during middle ear surgeries under local Anesthesia: a multicentric randomized double blind study. Jr KIMSU. 2015;4(3):32-40.
- Dogan R, Erbek S, Gonencer HH, Erbek HS, Isbilen C, Arslan G. Comparison of local anaesthesia with dexmedetomidine sedation and general anaesthesia during septoplasty. Eur J Anaesthesiol. 2010;27(11):960-964.
doi pubmed - Schmalbach CE. Patient safety and anesthesia considerations for office-based otolaryngology procedures. Otolaryngol Clin North Am. 2019;52(3):379-390.
doi pubmed - Taghinia AH, Shapiro FE, Slavin SA. Dexmedetomidine in aesthetic facial surgery: improving anesthetic safety and efficacy. Plast Reconstr Surg. 2008;121(1):269-276.
doi pubmed - Hillman DR, Loadsman JA, Platt PR, Eastwood PR. Obstructive sleep apnoea and anaesthesia. Sleep Med Rev. 2004;8(6):459-471.
doi pubmed - Schmidt SH, Anniko M, Hellstrom S. Electrophysiological effects of the clinically used local anesthetics lidocaine, lidocaine-prilocaine and phenol on the rat's inner ear. Eur Arch Otorhinolaryngol. 1990;248(2):87-94.
doi pubmed - Usmani H, Quadir A, Siddiqui RA, Sharma SC. Ondansetron and dexamethasone in middle ear procedures. Indian J Otolaryngol Head Neck Surg. 2003;55(2):97-99.
doi pubmed - le Nobel GJ, Cushing SL, Papsin BC, James AL. Intraoperative bleeding and the risk of residual cholesteatoma: a multivariate analysis. Otol Neurotol. 2017;38(4):529-534.
doi pubmed - Bhananker SM, Posner KL, Cheney FW, Caplan RA, Lee LA, Domino KB. Injury and liability associated with monitored anesthesia care: a closed claims analysis. Anesthesiology. 2006;104(2):228-234.
doi pubmed - Liem EB, Joiner TV, Tsueda K, Sessler DI. Increased sensitivity to thermal pain and reduced subcutaneous lidocaine efficacy in redheads. Anesthesiology. 2005;102(3):509-514.
doi pubmed - Fournier I, Caron C, McMurtry CM, Lapointe A, Giguere C, Dore-Bergeron MJ, Bergeron M. Comparison of tympanostomy tubes under local anesthesia versus general anesthesia for children. Laryngoscope. 2024;134(5):2422-2429.
doi pubmed - Lustig LR, Ingram A, Vidrine DM, Gould AR, Zeiders JW, Ow RA, Thompson CR, et al. In-office tympanostomy tube placement in children using iontophoresis and automated tube delivery. Laryngoscope. 2020;130(Suppl 4):S1-S9.
doi pubmed - Kouba DJ, LoPiccolo MC, Alam M, Bordeaux JS, Cohen B, Hanke CW, Jellinek N, et al. Guidelines for the use of local anesthesia in office-based dermatologic surgery. J Am Acad Dermatol. 2016;74(6):1201-1219.
doi pubmed - Ogle OE, Mahjoubi G. Local anesthesia: agents, techniques, and complications. Dent Clin North Am. 2012;56(1):133-148.
doi pubmed - Scarfone RJ, Jasani M, Gracely EJ. Pain of local anesthetics: rate of administration and buffering. Ann Emerg Med. 1998;31(1):36-40.
doi pubmed - Bhole MV, Manson AL, Seneviratne SL, Misbah SA. IgE-mediated allergy to local anaesthetics: separating fact from perception: a UK perspective. Br J Anaesth. 2012;108(6):903-911.
doi pubmed - Bartfield JM, Jandreau SW, Raccio-Robak N. Randomized trial of diphenhydramine versus benzyl alcohol with epinephrine as an alternative to lidocaine local anesthesia. Ann Emerg Med. 1998;32(6):650-654.
doi pubmed - Richards KA, Stasko T. Dermatologic surgery and the pregnant patient. Dermatol Surg. 2002;28(3):248-256.
doi pubmed - Butler DC, Heller MM, Murase JE. Safety of dermatologic medications in pregnancy and lactation: Part II. Lactation. J Am Acad Dermatol. 2014;70(3):417.e411-410; quiz 427.
doi pubmed - Gessler EM, Hart AK, Dunlevy TM, Greinwald JH, Jr. Optimal concentration of epinephrine for vasoconstriction in ear surgery. Laryngoscope. 2001;111(10):1687-1690.
doi pubmed - Krunic AL, Wang LC, Soltani K, Weitzul S, Taylor RS. Digital anesthesia with epinephrine: an old myth revisited. J Am Acad Dermatol. 2004;51(5):755-759.
doi pubmed - Serrera Figallo MA, Velazquez Cayon RT, Torres Lagares D, Corcuera Flores JR, Machuca Portillo G. Use of anesthetics associated to vasoconstrictors for dentistry in patients with cardiopathies. Review of the literature published in the last decade. J Clin Exp Dent. 2012;4(2):e107-111.
doi pubmed - Gormley DE. Cutaneous surgery and the pregnant patient. J Am Acad Dermatol. 1990;23(2 Pt 1):269-279.
doi pubmed - Neal JM, Mulroy MF, Weinberg GL, American Society of Regional A, Pain M. American Society of Regional Anesthesia and Pain Medicine checklist for managing local anesthetic systemic toxicity: 2012 version. Reg Anesth Pain Med. 2012;37(1):16-18.
doi pubmed - El-Boghdadly K, Pawa A, Chin KJ. Local anesthetic systemic toxicity: current perspectives. Local Reg Anesth. 2018;11:35-44.
doi pubmed - Statement on Office Based Anesthesia. American Society of Anesthesiologists. 2019. Retrieved July 8, 2024, from https://www.asahq.org/standards-and-practice-parameters/statement-on-office-based-anesthesia.
- Hancox JG, Venkat AP, Hill A, Graham GF, Williford PM, Coldiron B, Feldman SR, et al. Why are there differences in the perceived safety of office-based surgery? Dermatol Surg. 2004;30(11):1377-1379.
doi pubmed - Junco R, Bernard A, Anderson LS. Report of the special committee on outpatient (office-based) surgery. Dallas, Texas: Federation of State Medical Boards. 2002.
- Bensoussan Y, Anderson J. In-office laryngeal procedures (IOLP) in Canada: current safety practices and procedural care. J Otolaryngol Head Neck Surg. 2018;47(1):23.
doi pubmed - Lancer JM, Fisch U. Local anaesthesia for middle ear surgery. Clin Otolaryngol Allied Sci. 1988;13(5):367-374.
doi pubmed - American Society of Anesthesiologists Task Force on S, Analgesia by N-A. Practice guidelines for sedation and analgesia by non-anesthesiologists. Anesthesiology. 2002;96(4):1004-1017.
doi pubmed - Saliba I, Woods O. Hyaluronic acid fat graft myringoplasty: a minimally invasive technique. Laryngoscope. 2011;121(2):375-380.
doi pubmed - Shoman NM. Clinical and audiometric outcomes of palisade cartilage myringoplasty under local anesthetic in an office setting. Am J Otolaryngol. 2019;40(4):482-486.
doi pubmed - Monfared A, Bergeron CM, Ortiz J, Lee H, Kamine K, Dray T, Gunsalus R. Bivalve cartilage inlay myringoplasty: an office-based procedure for closing small to medium-sized tympanic membrane perforations. Otolaryngol Head Neck Surg. 2008;139(5):630-634.
doi pubmed - Sakagami M, Yuasa R, Yuasa Y. Simple underlay myringoplasty. J Laryngol Otol. 2007;121(9):840-844.
doi pubmed - Wu M, Lou Z. Local anesthesia-based modified cartilage "Inlay" graft myringoplasty for repairing large perforation. Ear Nose Throat J. 2023.
doi pubmed - Shoman N. Pilot study assessing the feasibility and clinical outcomes of office-based ossiculoplasty. Ann Otol Rhinol Laryngol. 2019;128(1):50-55.
doi pubmed - Neumann C, Yung J, Carroll PH. Mastoid surgery under local anesthesia for medically unfit patients: techniques and outcome. Ann Otol Rhinol Laryngol. 2013;122(10):613-618.
pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.