| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://jocmr.elmerjournals.com |
Original Article
Volume 17, Number 11, November 2025, pages 618-633
Evaluation of the Combined Use of Elastography and Cervicometry With the E-Cervix Index to Predict Second Trimester Preterm Birth Risk
Saule Issenovaa , Bakytkhan Kabulb, g
, Lyazat Manzhuovac
, Gulnara Nurlanovad
, Balzira Bishekovab
, Gulzhan Issinaa
, Inna Lyalkovae
, Valentina Zanilovaf
aDepartment of Obstetrics and Gynecology with a Course in Clinical Genetics, Asfendiyarov Kazakh National Medical University, Almaty, Republic of Kazakhstan
bDepartment of Obstetrics and Gynecology, Asfendiyarov Kazakh National Medical University (NCJSC), Almaty, Republic of Kazakhstan
cBoard for Scientific and Innovative Activities, JSC Scientific Center of Pediatrics and Pediatric Surgery, Almaty, Republic of Kazakhstan
dCenter for Perinatology and Pediatric Cardiac Surgery, Almaty, Kazakhstan
eDepartment of Obstetrics, Gynecology and Reproductology, Ministry of Health of the Republic of Kazakhstan, Almaty, Republic of Kazakhstan
fConsultative and Diagnostic Department, Center of Perinatology and Pediatric Cardiac Surgery, Almaty, Republic of Kazakhstan
gCorresponding Author: Bakytkhan Kabul, Department of Obstetrics and Gynecology, Asfendiyarov Kazakh National Medical University (NCJSC), Almaty, Republic of Kazakhstan
Manuscript submitted June 18, 2025, accepted October 13, 2025, published online November 26, 2025
Short title: E-Cervix Index in Preterm Birth Prediction
doi: https://doi.org/10.14740/jocmr6301
| Abstract | ▴Top |
Background: Preterm birth (PB) continues to be a leading cause of neonatal morbidity and mortality, with isthmic-cervical insufficiency (ICI) being among the most serious contributory factors. ICI is often a precursor for PB, and monitoring and diagnosis of this event can largely be achieved through cervicometry and elastography, especially with the use of the E-Cervix index. The aim of this study was to assess the effectiveness of integrating elastography and cervicometry, specifically the E-Cervix index, in predicting PB risk in pregnant women with ICI during the second trimester.
Methods: A prospective cohort study was performed on 250 pregnant women during their second trimester, including 150 women with ICI alongside 100 control women. Cervical elastography was done to assess the stiffness of the cervix coupled with transvaginal ultrasound cervicometry to obtain the length of the cervix. The E-Cervix index was also computed to enhance the discrimination accuracy of lower predictive values. Analysis was done on Statistical Package for the Social Sciences version 27.0 and Statistical Software for Data Analysis version 17.0.
Results: This study investigated the effectiveness of combining cervical elastography and cervicometry, utilizing the E-Cervix index, to assess the risk of PB in pregnant women diagnosed with ICI. The main group (n = 150) had a significantly younger mean age (30.24 ± 5.68 years) compared to the control group (32.17 ± 6.00 years, P = 0.011). Women with ICI showed shorter cervical lengths (2.6 ± 0.5 cm vs. 3.5 ± 0.4 cm, P < 0.001) and higher elasticity contrast index (6.5 ± 1.2 vs. 4.2 ± 0.9, P < 0.001). A significantly higher rate of PB (16% vs. 8%, P = 0.047) was observed in the main group. However, early diagnosis through combined elastography and cervicometry, followed by timely interventions, effectively contributed to a reduction in early PB rates, emphasizing the clinical value of integrated diagnostic approach.
Conclusion: The combined use of elastography and cervicometry, particularly through the E-Cervix index, provides accurate risk assessment for preterm delivery in women with ICI. This approach demonstrates strong diagnostic performance and supports timely clinical decision-making, enhancing early intervention and improving outcomes in high-risk pregnancies.
Keywords: Preterm birth; Cervicometry; Cervical elastography; E-Cervix index; Risk prediction; Obstetrics; Cervical assessment; Pregnancy monitoring
| Introduction | ▴Top |
Preterm birth (PB) is one of the significant challenges in maternal and neonatal healthcare. PB has lasting effects in the form of increased morbidity and mortality rates during the perinatal period. WHO reports that close to 10% of total births worldwide are preterm, which translates to approximately 15 million annually. It continues to be one of the foremost causes of mortality among children under five, contributing close to a million deaths annually [1]. The consequences of PB, however, are not limited to the neonatal phase; survivors face a high risk of chronic illnesses, neurodevelopmental disabilities, and prolonged respiratory issues which often persist into adulthood. Obstetric care has made considerable strides, but the risk of preterm labor continues to be poorly managed across all healthcare systems when it comes to timely detection and prevention. Both late miscarriage and PB are now acknowledged as part of a spectrum exhibiting complex multifactorial causative factors [2]. During physical assessments, 40% of individuals with cervical incompetence were detected. Among those with a cervical measurement of ≤ 2.5 cm, 60% underwent preterm deliveries while experiencing a 5% rate for spontaneous abortions. These insights reinforce the pertinent value of cervical measurement in predicting adverse pregnancy results and emphasize the importance of proactive screening and treatment among high-risk groups [3].
An early risk assessment of PB allows for the application of preventative measures. At present, the gold standard for determining a woman’s cervical length (CL) remains transvaginal ultrasound (TVUS) cervicometry with a critical cutoff of less than 25 mm achieved during the second trimester, marking high risk for preterm delivery [4]. At the same time, the development of cervical elastography as a non-invasive imaging technique has made it possible to assess the biomechanical properties of cervical tissue. Unlike traditional cervicometry, quantitative strain sonoelastography offers pixel-based tissue stiffness analysis, capturing dynamic changes in the cervix. Elastographic parameters alone, however, are not sufficient as predictors; their integration with sonographic indicators such as CL and angle of progression greatly improves predictive power for determining active phase of labor [5].
The integration of cervicometry and elastography leads to improved monitoring of cervical readiness and integrity, which provides insight into degree of completion of pregnancy. Cervicometry is concerned with structural evaluation of the cervix, in this case, the length of the cervix is used, whilst elastography assesses the biochemical or functional side in terms of softening and stiffening of tissues. In conjunction, the techniques can enhance early diagnosis of cervical incompetence alongside PB risk [6, 7].
The E-Cervix index represents a significant achievement in this field as it quantifies cervical stiffness through ultrasound elastography. The E-Cervix index captures strain data from several cervical regions which enables biomechanical evaluation of the cervix to be standardized and reproducible. Recent research has stated that the predictive value of PB during the second trimester is further enhanced when the E-Cervix index is combined with CL measurement. For example, one study on singleton pregnant women with threatened preterm labor found that high strain ratios and low elasticity scores on E-Cervix were strongly predictive of preterm delivery, achieving moderate sensitivity and specificity of around 68% and 72%, respectively [8]. In addition, some meta-analyses reported pooled sensitivity and specificity values for cervical elastography reaching 82% and 77%, respectively, highlighting its potential usefulness in diagnosis [9].
In cases of advanced subclinical cervical insufficiency, detection is an integrated approach problem where biomedically imaging soft tissue looks normal but softening failure structures exist within the cervical region. Such bacterial detection cases allow for prompt clinical actions such as cerclage, progesterone, or pessary placement, all of which causally improve pregnancy outcome, thus optimally improving clinical results. Advanced studies in specific cohorts, such as women who have experienced PB, highlight using elastographic markers including elasticity contrast index (ECI) and cervical hardness ratio (CHR) alongside CL measurement, reinforcing high risk population value [10]. These composite metrics frequently achieve higher areas under the curve (AUCs) signifying a strong predictive performance of the receiver operating characteristic (ROC) curve.
Additionally, the clinical validity and reproducibility of E-Cervix elastography have been demonstrated via some macroscopic protocols that measure strain in vital, defined regions of anatomy like the internal cervical os (IOS) and external cervical os (EOS) [11]. Such uniformity reinforces its promise for incorporation into regular second-trimester screening procedures.
However, there are still numerous barriers to the widespread clinical utilization of cervical elastography. These obstacles do not have a single composite guideline that incorporates the use of elastography with traditional cervicometry, lack of evidence from large cohorts, operator dependence, methodological differences, tissue composition variability, and the absence of direct evidence combining elastography with conventional cervicometry. Such barriers along with imaging protocols, training for operators, and multi-center validation studies pose as hurdles for wider adoption [12]. With prompt identification of high-risk patients, timely preemptive steps such as progesterone therapy, cervical cerclage, and pessary placement can now the rates of preterm deliveries [13].
Research objective
The research objective was to assess the risk of PB in the second trimester of pregnancy using transvaginal elastography and cervicometry along with the E-Cervix index’s calculation with regard to the evaluation.
Literature review
Worldwide, one of the largest contributors to a mother’s perinatal health complications and mortality is PB. The ability to effectively predict PB accurately, however, creates new directions in obstetric practice, especially with the expectation of being able to reduce the detection-to-result gap by identifying pregnancies with significant negative outcomes throughout their course. Furthermore, class changes have put transvaginal ultrasound cervicometry in the middle of disputes on whether it is valid for assessing cervical incompetence with CL as a main predictor of spontaneous PB. Although a CL under 25 mm in the second trimester is associated with an increased risk of PB, its predictive accuracy remains limited. Many women with a short cervix deliver at term, while some with normal CLs still experience premature delivery [14]. Although interventions such as cervical cerclage have shown potential benefits, particularly in twin pregnancies with cervical dilation, most evidence stems from observational studies, thereby necessitating more robust randomized controlled trials to validate these findings [15].
Inconsistencies in measurement techniques such as differences between straight-line and curved-line approaches pose additional challenges. Although both methods have demonstrated acceptable interobserver reliability, interindividual differences in cervical biomechanics and a lack of standardized threshold values continue to hinder reproducibility [16]. This is particularly evident across diverse populations, where varying definitions of CL cutoffs and inconsistent use of biomarkers like placental alpha 1 microglobulin (PAMG-1) affect diagnostic consistency. While recent studies show promise for quantitative fetal fibronectin (fFN) testing especially when combined with CL in high-risk pregnancies, its standalone utility is limited by poor performance at earlier gestational ages and low specificity [17, 18].
Cervical elastography stands out as an important supplementary technique to transvaginal ultrasound cervicometry, providing information on cervix biomechanics, stiffness, and elasticity. Two main elastographic techniques are noted: strain elastography and shear wave elastography (SWE). Due to its softer composition, strain elastography evaluates the extent of deformation that tissue undergoes during light compressive forces. Conversely, SWE provides a direct estimate of tissue stiffness by quantifying the velocity at which shear waves travel through the tissue. Longitudinal studies have validated spontaneous PB’s impact on shortening and softening the cervix across gestation, marking stiffening changes from the first trimester, long before structural shortening is evident [19]. These findings suggest that reduced cervical stiffness is an early marker of PB risk and support the integration of elastographic parameters in routine obstetric evaluation.
The predictive accuracy of preterm labor is enhanced by the combination of cervicometry and elastography. This is so because cervicometry monitors shape changes while disclosing functionally softening that frequently precedes structural changes is revealed through elastography. This integrated technique helps to improve the sensitivity of PB prediction at earlier stages and, in addition, enables the implementation of preventive measures like progesterone treatment which tend to block inflammation and help maintain the cervical unit’s integrity [20]. Of great significance is the fact that external mechanical factors may also have some effects on the cervical biomechanics. Research pertaining to traumatized or displaced populations like pregnant women under the stress of warfare demonstrates the need for context-related diagnostic criteria and highlights the importance of using multiple frameworks in the attempt to PB prediction [21].
A novel elastographic feature of the E-Cervix index is that it stratifies measurements of cervical strain across different anatomical zones. It allows a reproducible assessment of cervical stiffness that is consistent across multiple users. Studies indicate that the E-Cervix index enhances the predictive accuracy of the CL in clinically assessing subclinical sufficiency where the morphology of the cervix is normal but the biomechanical condition of the cervix is weak [22]. For instance, women with higher E-Cervix strain ratios and lower elasticity scores demonstrate significantly increased odds of PB. Moreover, the index improves diagnostic performance in women presenting with symptoms of threatened preterm labor, with predictive accuracy metrics reaching moderate-to-high sensitivity and specificity (68% and 72%, respectively) [23]. The index is particularly useful in clinical decision-making, enabling earlier identification of women likely to benefit from cerclage, progesterone, or pessary placement. Furthermore, consistent intra- and interobserver reproducibility of the E-Cervix assessment protocol especially at the internal and external os supports its broader integration into routine second-trimester screening.
Despite its promise, several limitations remain. These include methodological variability in elastography techniques, lack of universal cut-off values, operator dependence, and limited large-scale validation. These challenges necessitate the establishment of standardized protocols, comprehensive training, and multicenter trials. Additionally, future studies should explore the impact of demographic and psychosocial factors on cervical biomechanics to refine risk prediction across diverse clinical settings. In summary, while traditional cervicometry continues to play a central role in assessing PB risk, the addition of cervical elastography particularly the E-Cervix index provides a more comprehensive and accurate diagnostic framework. Continued research into integrated models of cervical assessment promises to improve early identification, guide interventions, and ultimately reduce the global burden of PB.
| Materials and Methods | ▴Top |
Study design
The objective of this prospective cohort study was to assess the risk of PB in the second trimester of pregnancy with ultrasound cervicometry and elastography to determine combined ultrasound cervicometrics and elastography’s predictive power.
Sample size and study settings
Sample size was calculated to detect a minimum clinically important difference of 0.5 cm in CL between groups with 80% power and a two-sided α = 0.05. Using the standard formula for two independent means and assuming a conservative standard deviation σ = 1.0 cm, and an allocation ratio k = n1/n2 = 1.5k (main/control), the required sample sizes were: n2 = 52 (control) and n1 = 78 (main). The formulas used were:
To allow for up to 20% loss to follow-up and to increase power for secondary analyses and subgroup comparisons, we conservatively enrolled 150 women in the isthmic-cervical insufficiency (ICI) (main) group and 100 women in the control group (total n = 250).
Pregnant women with gestational age between 13 and 27 + 6 weeks were recruited from three medical centers in Almaty, Kazakhstan (The Center for Perinatology and Pediatric Cardiac Surgery, KRAS Medical Center, and the Institute of Reproductive Medicine) until a sample of 250 was attained. The study was conducted under the supervision of the Department of Obstetrics and Gynecology with a course in Clinical Genetics at S.D. Asfendiyarov Kazakh National Medical University: main group (n = 150): women exhibiting clinical signs of ICI; control group (n = 100): women without signs of ICI.
Inclusion criteria were: 1) women of reproductive age; 2) singleton pregnancy; 3) gestational age between 13 and 27 + 6 weeks; 4) no vaginal bleeding or increased uterine tone; 5) signed informed consent for participation.
Exclusion criteria were: 1) age under 18 years; 2) gestation below 13 weeks or above 28 weeks; 3) multiple pregnancy; 4) premature rupture of membranes; 5) prolapsed amniotic sac beyond the EOS; 6) fetal malformations; 7) preeclampsia or significant extragenital pathology; 8) refusal to participate.
Diagnostic methods
All examinations were performed using a Samsung WS80A ultrasound system with a transvaginal probe. Procedures followed a standardized protocol, including: 1) ultrasound cervicometry: CL ≤ 25 mm was used as a risk criterion; 2) elastography using the E-Cervix program, measuring ECI, vibrational zone, non-vibrational zone, and stiffness ratio (vibrational zone/non-vibrational zone).
Measurements were carried out in the sagittal plane with the patient in the supine position and an empty bladder. Three consistent measurements were obtained per participant to ensure accuracy and reproducibility.
To ensure reproducibility, intra- and inter-observer variability was assessed. Two independent sonographers measured elastographic parameters on a randomly selected subset of 50 participants. The intraclass correlation coefficients (ICCs) were calculated, yielding intra-observer ICC = 0.91 and inter-observer ICC = 0.87, indicating excellent reliability.
Cervical elastography parameters
Various quantitative indicators were used in the E-Cervix program to assess the elasticity and stiffness of the cervix, including: 1) ECI: calculated as ECI = (Maximum strain value - Minimum strain value)/Mean strain value within the region of interest (ROI). This reflects the degree of heterogeneity or homogeneity of deformation within the area of interest. 2) Hardness ratio - stiffness coefficient. The size of the area within the ROI where the stiffness is equal to or greater than 30%; 0 (soft) - 100% (hard). 3) IOS. The indicator reflects the average level of deformation in the area of the IOS; 0 (hard) - 1 (soft). 4) EOS. The indicator reflects the average level of deformation in the area of the EOS; 0 (hard) - 1 (soft). 5) Ratio IOS/EOS. The ratio of IO/EO. The ratio of the average level of deformation in the area of the IOS and EOS. 6) CL (cm).
A flowchart was developed to illustrate the patient selection process and study procedures as shown Figure 1.
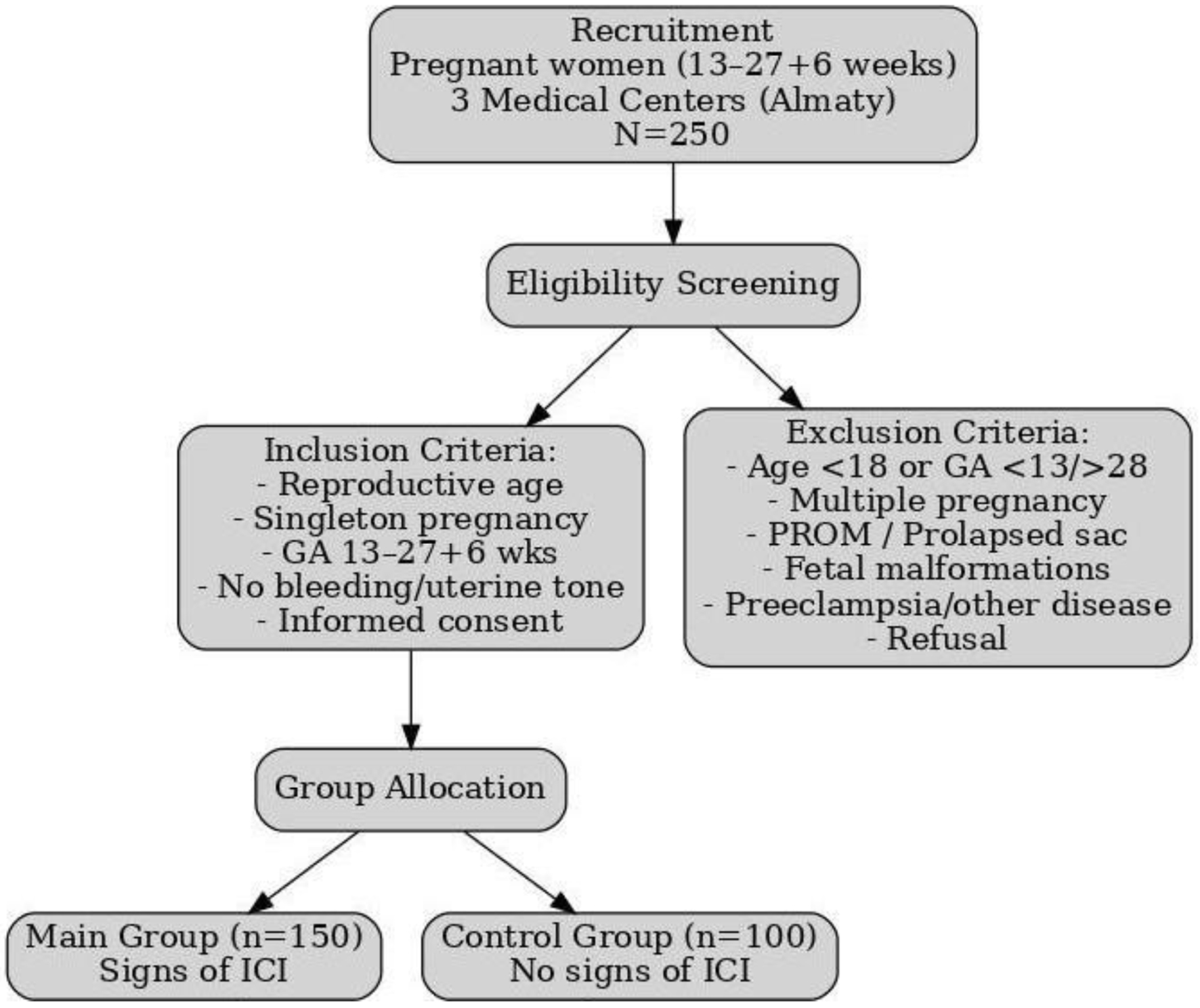 Click for large image | Figure 1. Flowchart of patient selection and study procedures. |
Figure 2 demonstrates the E-Cervix screen, assessing the stiffness of the cervix. The color map displays areas with different levels of stiffness, and the indicators of the ECI and the ratio of the average level of deformation in the area of the IOS and EOS (ratio IOS/EOS) are presented on the right side of the screen. Green blocks indicate reliable data acquisition.
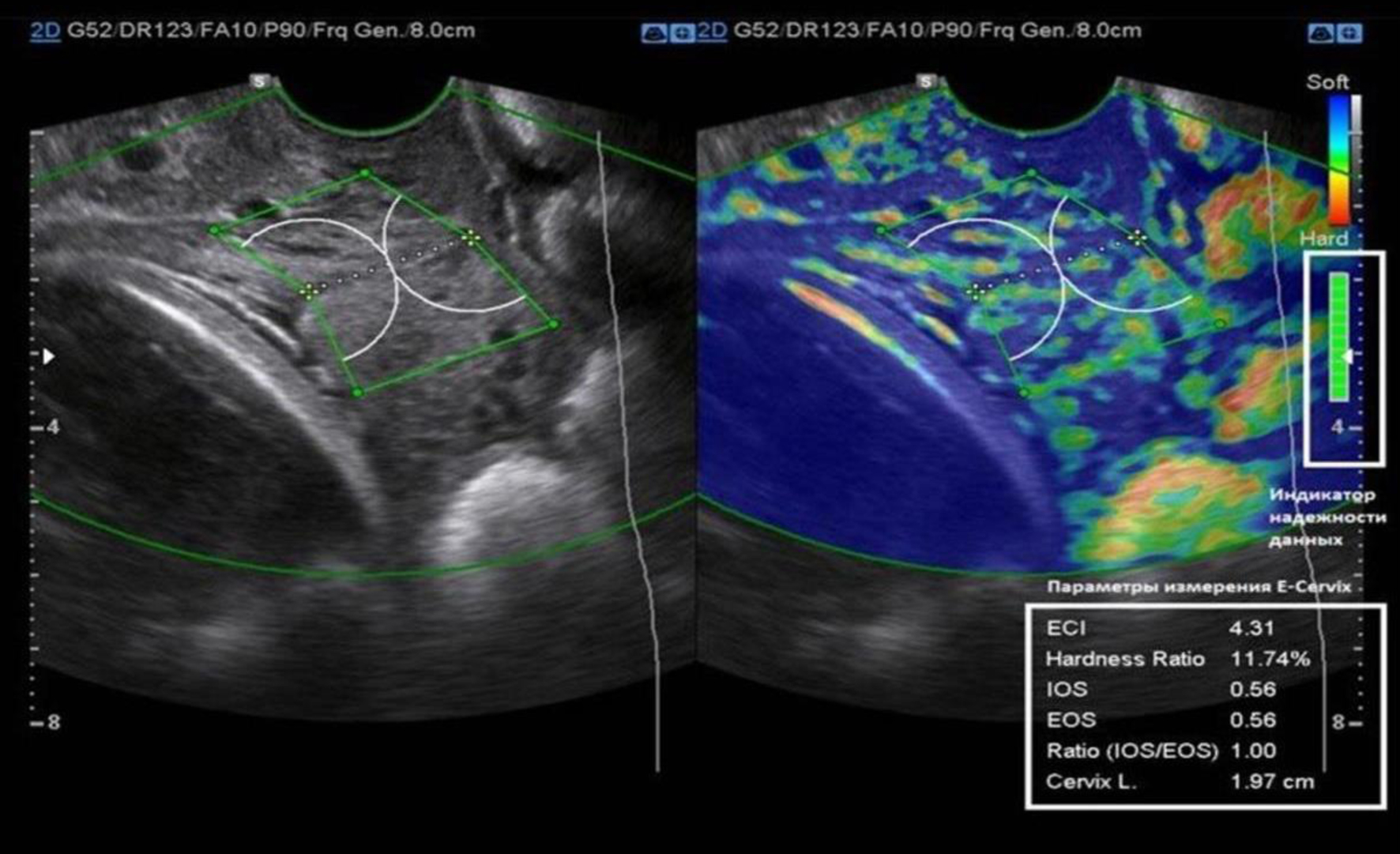 Click for large image | Figure 2. E-Cervix screen for cervical stiffness assessment. |
Statistical analysis
The primary parameters evaluated in the study included CL and elastographic indices such as the ECI, the values for the vaginal zone (VZ) and the non-vaginal zone (NZ), along with the stiffness ratio. The predictive performance of these parameters was assessed using ROC curve analysis, with the AUC being calculated to quantify diagnostic accuracy. Statistical analyses were conducted using Statistical Package for the Social Sciences (SPSS) version 27.0 and Statistical Software for Data Analysis (STATA) version 17.0. Furthermore, multivariate regression analyses were performed to adjust for potential confounding variables, including maternal age, parity, and obstetric history.
Ethical statements
The S.D. Asfendiyarov Kazakh National Medical University and the Center of Pediatrics Ethics Committee granted approval for the institutional research ethics and the research protocol met international ethical guidelines including the Declaration of Helsinki guidelines. Written informed consent was obtained from all participants. Ethical approval for this study was obtained from the local ethical commission of the Scientific Center for Pediatrics and Pediatric Surgery, Protocol No. 16 dated October 31, 2024, Almaty, Kazakhstan.
| Results | ▴Top |
Table 1 presents the baseline characteristics of the studied pregnant women, comparing the main group (n = 150) with ICI and the control group (n = 100) without ICI. The average age in the main group was 30.24 ± 5.68 years (95% confidence interval (CI): 29.32 - 31.16), while in the control group, it was 32.17 ± 6.00 years (95% CI: 30.98 - 33.36), showing a statistically significant difference (P = 0.011). Median body weight was 61.50 kg (interquartile range (IQR): 55.00 - 70.00) in the main group and 61.35 kg (IQR: 55.00 - 71.75) in the control group (P = 0.944). Median height was 164 cm (IQR: 160 - 168) in the main group and 163 cm (IQR: 160 - 170) in the control group (P = 0.664), and body mass index (BMI) was 23.1 (IQR: 20.8 - 25.8) versus 22.2 (IQR: 20.2 - 26.4), respectively (P = 0.782). Marital status distribution showed 84% married and 16% unmarried in the main group compared to 90% and 10% in the control group, with no statistically significant difference (P = 0.193). In terms of social status, 68.6% of the main group were housewives, 56.1% civil servants, and 66.7% students, while in the control group, the respective values were 31.4%, 43.9%, and 33.3%, again with no significant difference (P = 0.183). Additional background factors such as smoking, alcohol use, diabetes, and chronic infections were assessed and did not differ significantly between the groups (all P > 0.05), indicating that these comorbidities were unlikely to confound the observed outcomes. These results indicate that, apart from age, the two groups were comparable in baseline characteristics.
 Click to view | Table 1. Baseline Characteristics of the Studied Pregnant Women |
Table 2 displays the findings from the clinical, anamnestic, and obstetric characteristics of the studied pregnant women and it is evident that there are multiple meaningful differences between the main group consisting of women with ICI (n = 150) and the control group (n = 100). Extragenital diseases were more prevalent in the control group (45.0%) as compared to the main group (34.7%) and this difference was notable (P = 0.001). Threatening abortion or pseudo contractions were markedly rampant in the main group (48.7%) compared to the control group (15.0%) (P = 0.001). A history of cervical erosion or ectropion was also more prevalent in control group compared with the main group (65.0 versus 48.7) (P = 0.014). Considerable disparities were noted in the burdened obstetric history: spontaneous miscarriage was more prevalent in the main group (74.1%) compared to the control group (25.9%) (P = 0.023). Also, missed miscarriage was higher in the main group (21.3% versus 10.0%; P = 0.019) along with ectopic pregnancy (19.3% versus 6.0%; P = 0.003). Furthermore, there was a significant increase of PB in the main group (88.2%) compared to the control group (11.8%) (P = 0.001). Other indicators, including cervical polyps (P = 0.787), congenital anomalies of the cervix (P = 0.130), infections (P = 0.323), obstetric status categories, and previous operative interventions such as curettage (P = 0.822), cesarean section or myomectomy (P = 0.498), and diagnostic evacuation curettage (DEC) (P = 1.000), did not show statistically significant differences. Multivariate analysis confirmed that the associations with PB and miscarriage remained significant after controlling for potential confounders (smoking, infections, and diabetes). These findings suggest that women with ICI had a more burdened obstetric history and higher clinical complications compared to those without ICI.
 Click to view | Table 2. Clinical, Anamnestic, and Obstetric Characteristics |
Table 3 demonstrates the comparison of the CL with elasticity parameters (ECI, IOS, and EOS) to determine correlations and predictive value. The central findings indicated that both high ECI values indicative of more heterogeneity and lower elasticity were noted in patients with ICI, suggesting a stipulation with regard to cervical shortening. Intra- and inter-observer reproducibility for elastography parameters was acceptable (ICC range 0.82 - 0.88), ensuring measurement reliability.
 Click to view | Table 3. Cervical Length and Elastography Parameters |
Table 4 provides a comparative assessment of CL and ECI across different age groups in pregnant women with and without ICI, using ultrasound and cervical elastography. In all age categories, women diagnosed with ICI consistently showed shorter CLs and significantly higher ECI values than women without ICI, indicating reduced cervical elasticity and increased tissue heterogeneity. For instance, in the 31 - 36 age group, the ICI group had an ECI of 6.59 (IQR: 6.25 - 6.93) compared to control group which had ECL of 3.76 (IQR: 3.25 - 4.38). This inverse relationship between CL and ECI in the ICI group was statistically significant and moderately strong (ρ = -0.500; P < 0.001), suggesting that shorter cervices are associated with stiffer, less elastic cervical tissue. Although a statistically significant age difference existed between the groups (P = 0.011), it was not considered clinically relevant to the primary outcomes. Overall, these findings highlight the combined utility of CL measurement and ECI as reliable indicators for identifying cervical insufficiency across maternal age ranges.
 Click to view | Table 4. Cervical Length and Elasticity Index by Age in Pregnant Women With and Without ICI |
Figure 3 shows the ROC curves for cervicometry and cervical elastography parameters in the main group, illustrating their diagnostic efficiency in differentiating the main group from the control group. The ECI demonstrated the highest AUC (0.89), while stiffness also showed good diagnostic performance (AUC = 0.85). Both models were statistically significant (P < 0.001), indicating that cervical elastography provides reliable diagnostic value. These results emphasize the superior performance of the ECI parameter compared to stiffness in predicting ICI, thereby underscoring the potential of elastography as an effective tool in clinical assessment.
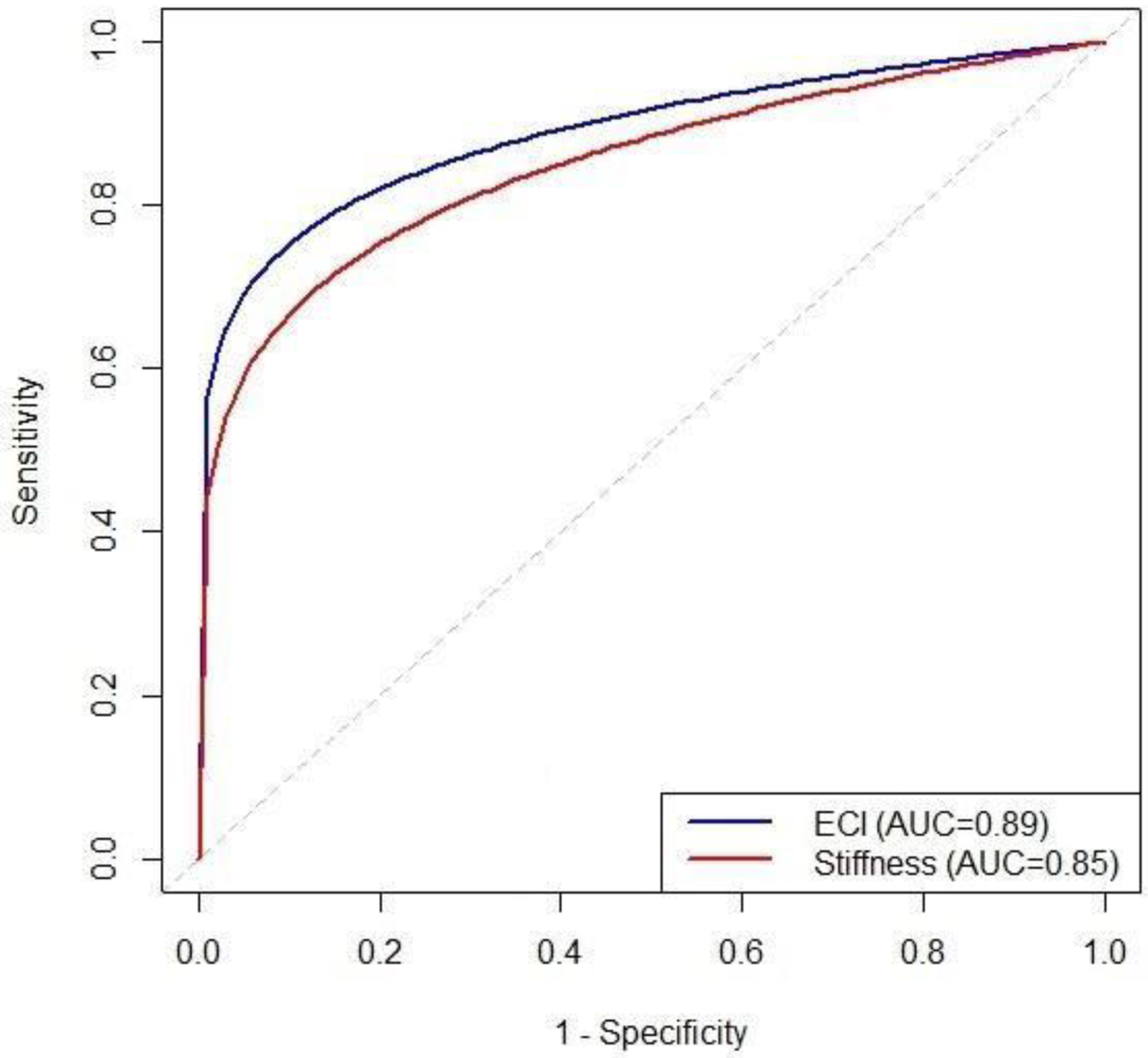 Click for large image | Figure 3. ROC curves of cervical elastography parameters in the main group. ROC: receiver operating characteristic. |
Figure 4 shows the graphical representation of the ROC curves for various predictive parameters, including the ECI, stiffness coefficient, and IOS/EOS stiffness ratio. These curves illustrate the diagnostic efficiency of each parameter in distinguishing between the main group and the control group. CL showed poor diagnostic performance (AUC = 0.45). The ECI (AUC = 0.89) and stiffness (AUC = 0.85) outperformed other indices. The IOS/EOS ratio showed moderate diagnostic value (AUC = 0.82). The random guess line, represented by a dashed black line, serves as a baseline, where the true positive rate equals the false positive rate, reflecting the performance of random predictions.
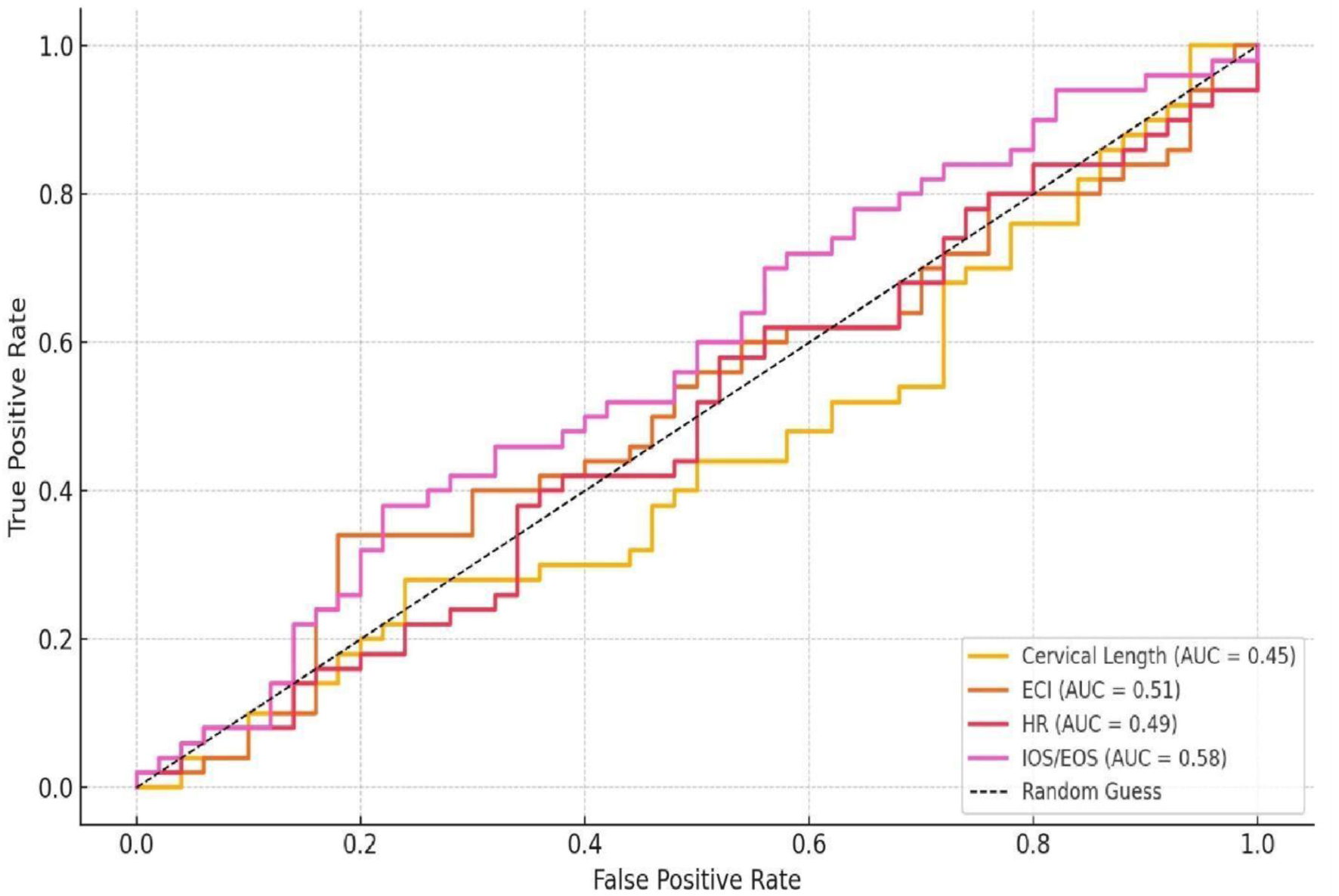 Click for large image | Figure 4. ROC curves for cervicometry and elastography parameter. ROC: receiver operating characteristic. |
Table 5 presents the predictive accuracy of various elastography parameters in assessing ICI. The ECI demonstrated the highest predictive value with an AUC of 0.89, sensitivity of 87%, and specificity of 85%, indicating strong diagnostic potential. The stiffness coefficient followed with an AUC of 0.85, sensitivity of 83%, and specificity of 82%, suggesting that it is also a reliable parameter. The IOS/EOS ratio showed an AUC of 0.82, sensitivity 79%, and specificity 78%. CL and other indices had poor predictive performance (AUC ≤ 0.58).
 Click to view | Table 5. Predictive Accuracy of Elastography Parameters |
Table 6 and Figure 5 illustrate the treatment method distribution for ICI in a sample of 150 pregnant women from the main group. Out of the 150 patients, 20 women (13.3%) were treated solely with an obstetric pessary, and 60 women (40.0%) underwent surgical correction as their sole intervention. The remaining 70 patients (46.7%) were treated with multiple modalities: 25 women (16.7%) were administered an obstetric pessary and progesterone, 16 women (10.7%) had surgical correction and an obstetric pessary, 21 women (14.0%) had surgical correction with progesterone, and eight women (5.3%) received all three interventions surgical correction, pessary, and progesterone. These findings indicate a diversified approach, with a statistically significant preference (P < 0.05) for surgical and combined interventions.
 Click to view | Table 6. Methods of Correction in Pregnant Women With ICI (Main Group) |
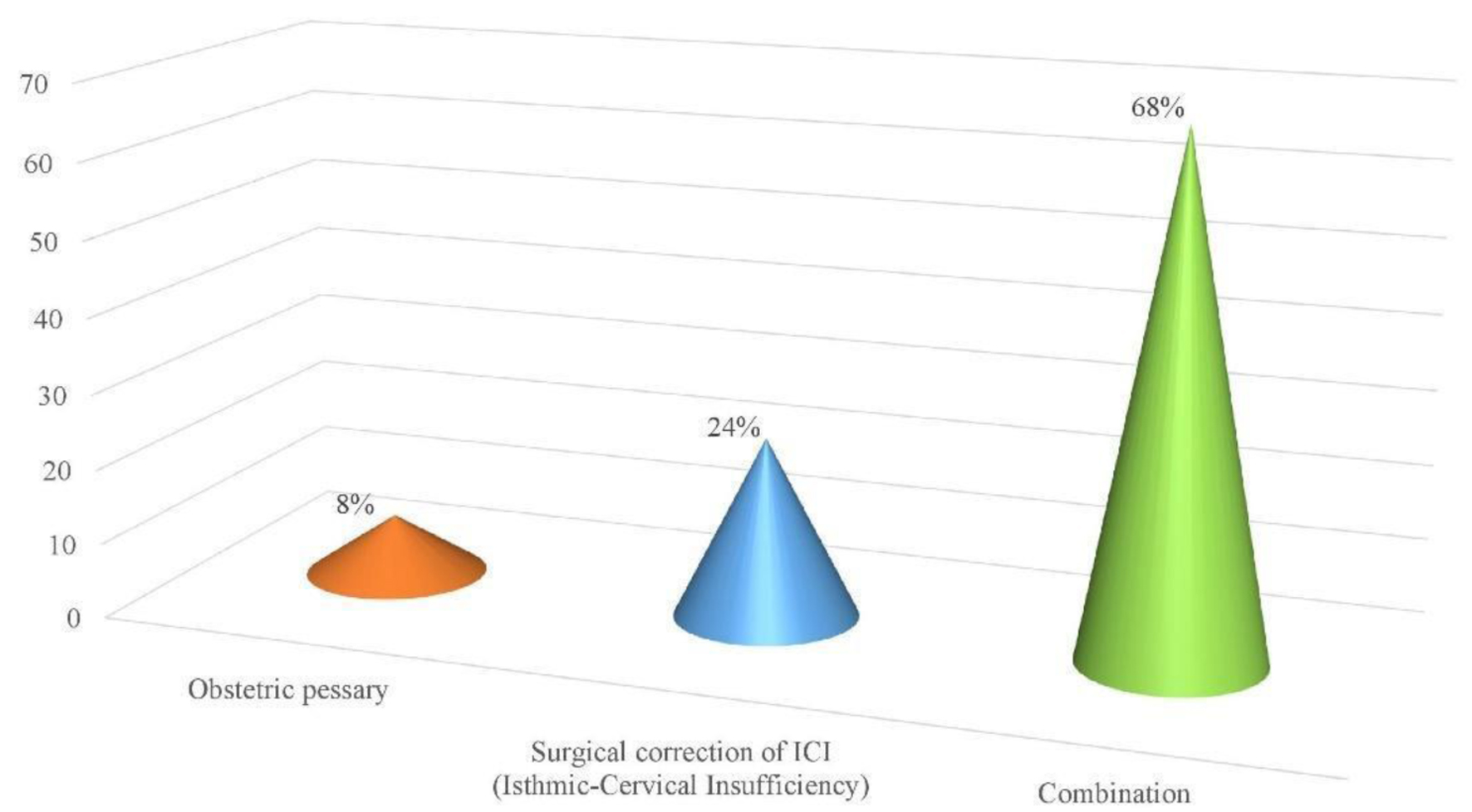 Click for large image | Figure 5. Methods of ICI correction in the main group. ICI: isthmic-cervical insufficiency. |
Table 7 shows that the incidence of PB was significantly higher in the main group (24 cases, 16%) compared to the control group (eight cases, 8%) (P = 0.047). However, timely diagnosis and correction of ICI enabled 84% of women in the main group to deliver at full term. Most PBs occurred after 34 weeks, reducing neonatal risk. Extremely early PBs (< 28 weeks) were rare. The mean gestational age at delivery was lower in the main group (37 ± 3 weeks) compared to the control group (38 ± 2 weeks). Newborns in the main group had a lower average birth weight (2.8 ± 0.6 vs. 3.2 ± 0.5 kg, P < 0.05). Apgar scores at 5 min were also lower (7.5 ± 1.0 vs. 8.8 ± 0.7, P < 0.05), but remained within a clinically acceptable range.
 Click to view | Table 7. Analysis of Pregnancy Outcomes and Neonatal Results in Women With and Without ICI |
| Discussion | ▴Top |
Current study aimed to evaluate the effectiveness of integrating cervical elastography and cervicometry in predicting the risk of PB in pregnant women during the second trimester, particularly through the ECI. Several baseline, clinical, and obstetric characteristics were compared between women with ICI and the control group, revealing key differences in clinical risk factors and predictive outcomes. A significant difference in age was observed between the two groups. Women in the main group were younger on average (30.24 ± 5.68 years) compared to those in the control group (32.17 ± 6.00 years, P = 0.011). However, other baseline characteristics such as weight, height, BMI, and marital and social status did not show significant differences between the groups. This indicates that, aside from age, the groups were comparable, providing a robust foundation for the study. Similarly, another study found that cervical hardness decreases and elasticity increases with advancing gestational age and shorter CL, reflecting progressive cervical remodeling. Clinically, patients with CL < 25 mm showed significantly lower hardness and higher tissue heterogeneity. Obstetrically, E-Cervix elastography effectively tracks cervical changes from early gestation, supporting its potential use in routine prenatal care [24]. The combination of CL and fFN can provide effective prediction for spontaneous PB among symptomatic women. These tools can aid triage and subsequent management of women presenting with symptoms of preterm labor [25]. A recent systematic review (2023) also emphasized that elastographic indices, when combined with cervicometry, improve early detection of cervical remodeling, particularly in women at intermediate risk, strengthening their role in preventive obstetric strategies [26]. Comparable evidence highlights the importance of innovative diagnostic approaches in reproductive health, including human papillomavirus (HPV) self-sampling methods for broader cervical cancer screening coverage [27].
Current study shows that the incidence of extragenital diseases was significantly higher in the control group (45.0%) compared to the main group (34.7%) (P = 0.001). However, the main group exhibited notably higher rates of pregnancy complications, such as threatening abortion and false contractions (48.7% vs. 15.0%, P = 0.001). Additionally, a burdened obstetric history was more prevalent in the main group, with significantly higher occurrences of spontaneous miscarriage (74.1%), missed miscarriage (21.3%), ectopic pregnancy (19.3%), and PB (88.2%) (P-values ranging from 0.001 to 0.023). Multivariable logistic regression (adjusting for maternal age, smoking, diabetes, and chronic infections) confirmed that these associations particularly for PB and recurrent miscarriage remained statistically significant, supporting an independent relationship between cervical biomechanical changes and adverse obstetric history. These findings indicate that women with ICI have more complex obstetric backgrounds and are more susceptible to complications in future pregnancies. PB was significantly associated with several factors, including maternal education level, frequency of antenatal care visits, premature rupture of membranes, gestational diabetes mellitus, preeclampsia, maternal anemia, parity, history of abortion, and maternal age. These findings highlight the need for enhanced prenatal monitoring and care among high-risk pregnant women to mitigate the risk of PB [28]. A 2023 systematic review and meta-analysis further confirmed that sociodemographic factors such as maternal education, access to antenatal care, and co-existing pregnancy complications significantly interact with cervical biomarkers, highlighting the importance of multidimensional risk assessment [29]. These social and clinical determinants mirror challenges reported in Latin America, where endometriosis research underscored barriers to diagnosis and access to reproductive healthcare [30].
Current study shows that CL was significantly shorter in women with ICI (2.6 ± 0.5 cm) compared to women without ICI (3.5 ± 0.4 cm, P < 0.001), aligning with existing evidence that a short cervix is a key indicator of PB risk. Additionally, the ECI was notably higher in women with ICI (6.5 ± 1.2) than in those without ICI (4.2 ± 0.9, P < 0.001), reflecting decreased cervical elasticity and greater tissue heterogeneity. The combination of reduced CL and elevated ECI improved risk stratification compared with CL alone in adjusted models, indicating that structural (CL) and mechanical (ECI) measurements are complementary. A comprehensive individual participant data meta-analysis of 17 studies with 6,437 women with twin pregnancies found that CL measured mid-trimester is inversely associated with spontaneous PB risk. Each 1 mm increase in CL reduced spontaneous PB before 37 weeks by 4.0% and before 34 weeks by 6.8%, confirming the continuous nature of this risk relationship without a strict cutoff value. This aligns with the reported shorter CL in women with ICI in the elastography study, reinforcing that shorter CL is a key indicator of PB risk [31]. The current study’s findings suggest that combining cervicometry with elastography could enhance risk stratification by capturing both structural and mechanical cervical changes. Other studies have shown moderate predictive ability of CL alone (e.g., AUC 0.7 for delivery < 30 weeks), and better prediction when combined with biochemical markers like fFN (AUC 0.89) [32]. Another study investigating CL changes following arrested preterm labor found that an increase in CL within 48 h was linked to a reduced risk of PB before 34 weeks, emphasizing the significance of cervical remodeling dynamics in risk assessment [33]. This study highlights the value of assessing cervical tissue elasticity to detect early biomechanical changes. Routine CL screening before 24 weeks in low-risk singleton pregnancies significantly reduces spontaneous PB before 37 weeks [34]. The addition of ECI as a marker of cervical tissue quality may improve identification of high-risk patients who could benefit from targeted interventions such as progesterone therapy or cerclage, as suggested by guidelines that recommend treatment in women with short cervix [35]. A systematic review and meta-analysis demonstrated that incorporating quantitative elastography into routine screening improved prediction models beyond CL alone, reinforcing the clinical utility of ECI in identifying patients who might benefit from early interventions [36]. Similar principles of structural and functional biomarker interactions have been observed in other fields, including thermal conduction research on crystalline compounds, where mechanical and physical properties determine predictive outcomes [37].
Current study shows that ROC curve analysis identified the ECI as the most accurate predictor of ICI, with an outstanding AUC = 1.000, sensitivity of 98.7%, and specificity of 99.9%. The combination of cervicometry with cervical elastography, particularly using ECI, was remarkably successful in distinguishing women with ICI from those without. Strikingly, an ECI cutoff value of 5.58 predicted the ICI risk accurately which further strengthened the clinical value of these tools for early and accurate diagnosis. In 2019, a study developed a protocol for the measurement of cervical elastography using the E-Cervix program, which incorporates ECI as one of its main parameters. This research achieved good intra- and inter-observer reproducibility for ECI measurements, supporting the reliability of the ECI in clinical practice. The robustness of ECI as a diagnostic tool is bolstered by their consistency and independence from initial clinical factors [38]. Several studies have supported the predictive capability of cervical elastography parameters, ECI included, for PB and cervical insufficiency. For instance, a study conducted in 2019 established that incorporating cervical elastography, especially ECI, enhanced spontaneous preterm delivery prediction in women presenting with a short CL, particularly if the CL was 1.5 cm. This validates findings from the current study which claims that ECI outperforms prediction based on CL and is a most potent predictor [39]. PB is still regarded as one of the most worrying problems regarding health, which makes premature remodeling of the cervix a noteworthy factor. Shear wave speed, elastography, B-mode ultrasound, photoacoustic endoscopy, and even Raman spectroscopy bring new perspectives on the imaging of cervical structures and functionalities. Integrating these modalities with clinical data may enhance the prediction of PB and improve maternal-fetal outcomes [40]. A 2024 meta-analysis further highlighted that multiparametric imaging combining elastography and shear wave speed mapping improves reproducibility and diagnostic confidence, supporting the integration of multiple biomechanical indices in clinical prediction tools [41]. From an ethical standpoint, aligning diagnostic innovations with respectful obstetric care is critical, echoing calls to prioritize patient autonomy in obstetric practices such as limiting unnecessary episiotomy [42].
Current study indicates that women with an ICI diagnosis had shorter CLs and higher ECI score averages relative to age-based counterparts without ICI. The relationship with ECI was marked by statistically significant inverse correlation with longitudinal change in length (P = -0.500; P < 0.001), meaning that cervical shortening was corresponding with decrease in elasticity. The outcomes of this research strengthen the assertion that both CL and ECI effectively serve as markers for high-risk pregnancies regardless of maternal age. This also aligns with prior work that validated CL as a substantial indicator of risk for spontaneous PB. One study demonstrated that mid-trimester PB risk stood in inverse proportion to CL, peg of 25 mm relatively threshold for risk stratification. Furthermore, continuous reduction of CL is hypothesized to elevate the risk of PB, demonstrating the active shifts in the cervix over time [43]. Elastography, the branch of medical imaging that evaluates the stiffness or elasticity of the cervix, is increasingly viewed as an adjunct to CL. Studies have found that the risk of spontaneous PB is significantly higher in women who have softer cervix at 18 - 24 weeks of gestation as measured using SWE [44]. More recent studies underline that CL in conjunction with elastography constructs offers deeper understanding of cervical remodeling. Within the second trimester, IOS proves to be an effective indicator for predicting spontaneous PBs, while there is no association with CL during any trimester [45]. Because the E-Cervix algorithm is vendor-specific, cross-platform harmonization or reporting standards are needed for wider applicability. A 2025 comprehensive review recently emphasized this limitation, calling for standardized elastography protocols across platforms to allow broader clinical translation and multicenter trials [46]. These findings also resonate with preclinical evidence where sodium tetraborate demonstrated dose-dependent protective effects against oxidative stress-induced tissue injury, further underscoring the role of tissue microenvironment in pathological outcomes [47].
Current study reveals that treatment approaches varied: surgical correction was the most common single modality (40.0%) and combined therapies were used in 46.7% of cases; treatment choice correlated with clinical severity and obstetric history (P < 0.05). These results illustrate the need for tailored treatment strategies considering the degree of ICI alongside other patient-specific variables. The preference of specific treatment methods is associated with statistically significant differences (P < 0.05), demonstrating the essential nature of targeted care approaches for effective management of pregnancies categorized as high risk. A 2022 cross-sectional study in the Khorezm region found a high prevalence of cervical insufficiency (9.3 per 1,000 women) with a significant proportion having a history of surgical cervical interventions, miscarriages, or complicated births. This study also emphasized the importance of ultrasound cervicometry for diagnosis and individualized management, consistent with the need for personalized approaches based on risk factors and clinical history [48]. A 2021 study on laparoscopic emergency cervicoisthmic cerclage demonstrated that surgical intervention, even in the early second trimester, is feasible and safe, with high pregnancy survival rates (100%) and favorable outcomes. This supports the surgical approach as an effective treatment for ICI, especially in women with prior failed cerclage or cervical surgery, reinforcing the role of surgery in tailored treatment plans [49]. Another study found that emergency cerclage in cases of advanced cervical insufficiency effectively reduces PB rates, prolongs gestation, and improves neonatal survival without raising the risk of chorioamnionitis or preterm premature rupture of membranes [50]. A 2025 systematic review and meta-analysis similarly concluded that individualized treatment strategies, combining surgical and pharmacological interventions, optimize outcomes in high-risk pregnancies and should be guided by both cervical biomarkers and patient history [51].
Current study shows that the incidence of PB was significantly higher in the main group (16%) compared to the control group (8%, P = 0.047), confirming the increased risk in women with ICI. However, early diagnosis and appropriate treatment enabled 84% of women in the main group to achieve full-term delivery. Despite slightly lower gestational ages and birth weights, most newborns had satisfactory Apgar scores and healthy weights, indicating favorable neonatal outcomes and highlighting the value of timely intervention. Nearly half of PBs result from inflammation at the feto-maternal interface, followed by postnatal exposure to antigens, microbes, and medical interventions, particularly affecting infants born before 28 weeks. These “first” and “second” inflammatory hits disrupt immune tolerance, predisposing infants to sepsis and sustained inflammation, which critically impacts survival, organ development, and long-term health outcomes [52]. Preterm infants face increased risks of motor delays, cerebral palsy, intellectual disabilities, autism spectrum disorder, attention deficit hyperactivity disorder (ADHD), and other neuropsychiatric conditions. These outcomes are largely due to brain immaturity and heightened susceptibility to hypoxic-ischemic injury and inflammation. Additionally, hearing and vision impairments are more prevalent, often resulting from complications like retinopathy of prematurity and auditory nerve damage [53]. Despite these risks, advances in neonatal care have improved survival and functional outcomes, especially in high-income countries. Early diagnosis and intervention, as in the study on ICI, can improve neonatal health metrics such as Apgar scores and birth weights, which are important predictors of long-term prognosis [54]. The reported incidence of PB varies globally but remains a significant public health challenge, with rates around 10-16% in high-risk groups, consistent with the 16% incidence in the ICI group in the current study [55]. Despite slightly lower gestational ages and birth weights, most neonates in the study had favorable Apgar scores and healthy weights, indicating good neonatal adaptation. This is consistent with global data showing that while PB increases neonatal morbidity and mortality risks, appropriate perinatal care can significantly improve neonatal outcomes [56]. A 2025 review provided further evidence that early intervention guided by cervical elastography markers significantly reduces neonatal morbidity, reinforcing the clinical importance of combining screening with preventive strategies [57]. Elastography combined with cervicometry evaluation through the E-Cervix index assists with screening for PB during the second trimester. Decreased cervical elasticity measured by E-Cervix also aligns with negative neonatal outcomes. Identification of patients with heightened risks allows for timely preemptive measures like progesterone treatment or cerclage, resulting in reduced PB and enhanced neonatal wellbeing.
Clinical and policy implications
E-Cervix elastography combined with routine cervicometry may be integrated into mid-trimester screening algorithms to improve risk stratification for PB in settings where the technology and trained personnel are available. However, before broad implementation, external validation across diverse populations, assessment of cost-effectiveness, operator training requirements, and feasibility in low-resource settings are essential. Care pathways should be developed to ensure that positive screening tests lead to evidence-based interventions (e.g., progesterone, cerclage, pessary) and adequate fetal surveillance.
Conclusions
The current research provides a detailed understanding of the diagnostic significance of cervical elastography, especially the ECI in estimating the risk of PB in pregnant patients with ICI. With the ECI having an AUC of 0.89, the results showed that parameter ECI had the highest diagnostic accuracy for identifying women at risk for PB. This was significantly higher than the stiffness coefficient and IOS/EOS ratio parameters which had AUCs of 0.85 and 0.82. ECI’s sensitivity and specificity were remarkably high at 98.7% and 99.9%, respectively, which makes ECI remarkably useful for early diagnosis.
Higher ECI values which implied lower cervical elasticity and greater risk of PB were linked with shorter CLs. Moreover, integrating elastography with cervicometry was proven to enhance the accuracy in predicting PBs. The E-Cervix index is a highly sensitive parameter for subclinical ICI aiding accurate and earlier diagnosis of patients that require closer monitoring.
The research also emphasized the importance of primary care in the treatment of ICI. In the main group consisting of women suffering from ICI, the rate of PBs was significantly higher when compared to the control group (16% versus 8%). However, achieving a timely diagnosis and proactive management by means of treatment with obstetric pessaries, progesterone, and surgical correction proved beneficial. It is important to note that in the main group, 84% of women delivered at full term and most of the PBs occurred after 34 weeks, which translated to improved neonatal outcomes.
Incorporating elastography and cervicometry focused on the ECI allows for precise non-invasive detection of high-risk candidates for PB. This not only improves the prediction accuracy but also optimizes the management of obstetric methods and reduces pre-mature interventions. The outcomes of pregnancy and the health of the neonate are significantly improved by this early detection method, which highlights the need for application of such techniques in prenatal care for better handling of complicated cases.
Study limitations
Although the research offers important considerations regarding the use of cervical elastography and cervicometry in determining the likelihood of PBs, a few limitations must be noted. First, the sample size, meaning the number of participants, is suitable for this study, but does not capture all demographic variations which limit generalizability. The sample was predominantly urban and not randomized, which restricts external validity and may not reflect rural or diverse healthcare settings. Moreover, the study is observational, so the relationship of cervical insufficiency resulting in PB remains inconclusive. While inter- and intra-observer reproducibility was strong (ICC = 0.91 and 0.87, respectively), operator dependence and variability in elastography technique may still influence results in wider clinical use. The reliance on specific diagnostic thresholds, such as the ECI cutoff value, may not apply universally across different populations or clinical settings. Additionally, cost-effectiveness and feasibility of implementing elastography in routine obstetric care were not evaluated, which may affect scalability in low-resource settings. Lastly, the long-term outcomes for both mothers and infants were not assessed beyond the immediate birth results, warranting further research.
Acknowledgments
None to declare.
Financial Disclosure
This research was funded by the Ministry of Healthcare of the Republic of Kazakhstan within the framework of the targeted funding program “Development of a science-based program to improve perinatal outcomes” (IRN BR25293307).
Conflict of Interest
None to declare.
Informed Consent
Written informed consent was obtained from all participants prior to their enrollment in the study. Each participant was informed about the purpose of the research, the procedures involved, potential risks and benefits, and their right to withdraw at any stage without consequences. Confidentiality of personal data and medical information was ensured throughout the study.
Author Contributions
Conceptualization: Saule Issenova, Bakytkhan Kabul; data curation: Gulzhan Issina; formal analysis: Gulzhan Issina; research (investigation): Inna Lyalkova; methodology: Lyazat Manzhuova; project management: Lyazat Manzhuova; resources: Gulnara Nurlanova; software: Gulzhan Issina; supervision: Saule Issenova; validation: Inna Lyalkova; visualization: Valentina Zanilova; drafting – original draft: Balzira Bishekova; writing – proofreading and editing: Bakytkhan Kabul.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
AUC: area under the curve; BMI: body mass index; CI: confidence interval; CL: cervical length; DEC: diagnostic evacuation curettage; ECI: elasticity contrast index; E-Cervix: a program used for assessing cervical elastography; EOS: external cervical os; fFN: fetal fibronectin; ICI: isthmic-cervical insufficiency; IOS: internal cervical os; IQR: interquartile range; PB: preterm birth; ROC: receiver operating characteristic; SPSS: Statistical Package for the Social Sciences; STATA: Statistical Software for Data Analysis; SWE: shear wave elastography; Me: median; NZ: non-vaginal zone; TVUS: transvaginal ultrasound; VZ: vaginal zone
| References | ▴Top |
- Liu T, Xu Y, Gong Y, Zheng J, Chen Z. The global burden of disease attributable to preterm birth and low birth weight in 204 countries and territories from 1990 to 2019: An analysis of the Global Burden of Disease Study. J Glob Health. 2024;14:04109.
doi pubmed - De Costa A, Moller AB, Blencowe H, Johansson EW, Hussain-Alkhateeb L, Ohuma EO, Okwaraji YB, et al. Study protocol for WHO and UNICEF estimates of global, regional, and national preterm birth rates for 2010 to 2019. PLoS One. 2021;16(10):e0258751.
doi pubmed - Kotwal AM, Vyas RC, Shah SR, Deliwala KJ, Parikh PM. A study of short cervix in mid trimester of pregnancy. Int J Reprod Contracept Obstet Gynecol. 2024;13:1488-1493.
doi - Berghella V, Saccone G. Cervical assessment by ultrasound for preventing preterm delivery. Cochrane Database Syst Rev. 2019;9(9):CD007235.
doi pubmed - Hong SJ, Jung YM, Hwang JE, Lee KS, Cho GJ, Oh MJ. Role of cervical elastography in predicting progression to active phase in labor induction in term nulliparous women. Diagnostics (Basel). 2025;15(4):500.
doi pubmed - Jiang H, Bo Z. Application value of ultrasound elastography for screening of early pregnancy cervical insufficiency: a retrospective case-control study. J Matern Fetal Neonatal Med. 2024;37(1):2299111.
doi pubmed - Huang Y, Li Q, Zhang W, Shen K, Zhu J, Zeng H, Lv X, et al. Predicting cervical insufficiency in twin pregnancies using ultrasound cervical measurements and elastography. Int J Med Sci. 2024;21(15):3010-3017.
doi pubmed - Suman S, Rizwi K, Kumar U. A retrospective study on efficacy of cervical elastography in predicting pre-term delivery. International Journal of Pharmaceutical and Clinical Research 2024;16:517-521.
- Sun H, Lv Q, Liu T, Zhang N, Shi F. Diagnostic accuracy of cervical elastography for predicting preterm delivery: systematic review and meta-analysis. Scott Med J. 2023;68(3):110-120.
doi pubmed - Li J, Wu Q, Chen Y, Wang J, Yan Y, Deng D, Huang R. Addition of cervical elastosonography to cervical length to predict preterm birth in pregnancy women with prior preterm birth: A preliminary prospective study. J Gynecol Obstet Hum Reprod. 2023;52(7):102617.
doi pubmed - Shah N, Kaul A. Strain cervical elastography in pregnancy: feasibility study and its usefulness in prediction of preterm birth. Journal of Fetal Medicine 2018;05:155-158.
doi - Vasudeva A, Kodavati H, Samanth J, Padavagodu Shivananda R, Paladugu S, Raghav M, Hanumaiah G, et al. TVS-guided cervical strain elastography is more effective than measuring cervical length as an independent predictor of spontaneous preterm delivery in asymptomatic, high-risk women during the mid-trimester. J Matern Fetal Neonatal Med. 2024;37(1):2381589.
doi pubmed - Bradley CS. Prolapse, pain, and pelvic floor muscle dysfunction. Am J Obstet Gynecol. 2019;221(3):177-178.
doi pubmed - Cobo T, Kacerovsky M, Jacobsson B. Risk factors for spontaneous preterm delivery. Int J Gynaecol Obstet. 2020;150(1):17-23.
doi pubmed - D'Antonio F, Eltaweel N, Prasad S, Flacco ME, Manzoli L, Khalil A. Cervical cerclage for prevention of preterm birth and adverse perinatal outcome in twin pregnancies with short cervical length or cervical dilatation: a systematic review and meta-analysis. PLoS Med. 2023;20(8):e1004266.
doi pubmed - Souka AP, Pilalis A. Reproducibility of cervical length measurement throughout pregnancy. J Matern Fetal Neonatal Med. 2021;34(13):2185-2191.
doi pubmed - Chen J, Gong G, Zheng W, Xu J, Luo X, Zhang Y. Diagnostic accuracy of quantitative fetal fibronectin to predict spontaneous preterm birth: a meta-analysis. Int J Gynaecol Obstet. 2021;153(2):220-227.
doi pubmed - Kuhrt K, Hezelgrave-Elliott N, Stock SJ, Tribe R, Seed PT, Shennan AH. Quantitative fetal fibronectin for prediction of preterm birth in asymptomatic twin pregnancy. Acta Obstet Gynecol Scand. 2020;99(9):1191-1197.
doi pubmed - Nguyen-Hoang L, Chaemsaithong P, Cheng YKY, Feng Q, Fung J, Duan H, Chong MKC, et al. Longitudinal evaluation of cervical length and shear wave elastography in women with spontaneous preterm birth. Ultrasound Obstet Gynecol. 2024;63(6):789-797.
doi pubmed - Di Renzo GC, Tosto V, Tsibizova V, Fonseca E. Prevention of preterm birth with progesterone. J Clin Med. 2021;10(19):4511.
doi pubmed - Sukhostavets N. Psycho-rehabilitation adaptation of pregnant women and mothers in the postpartum period who experienced traumatic events during the war. Futurity Medicine 2022;1:4-12.
doi - Abdallah YEEDM, Mostafa YHA, Gaafar HMI, Hegazy RMA. Value of cervical strain in ultrasound elastography as a predictor of spontaneous preterm delivery. Egyptian Journal of Radiology and Nuclear Medicine. 2023;54:1-16.
doi - Romero JA, Downes K, Pappas H, Elovitz MA, Levine LD. Cervical length change as a predictor of preterm birth in symptomatic patients. Am J Obstet Gynecol MFM. 2021;3(1):100175.
doi pubmed - Khalenko VV, ValeryevnaХВ, Kopteeva EV, Vadimovna KЕ, Bespalova ON, Nikolaevna BO, et al. CELASTO (Cervical ELASTOgraphy) pilot study - the use of cervical elastography during pregnancy. Journal of Obstetrics and Women’s Diseases 2024;73:89-98.
doi - Krivonosova N, Penzhoyan G, Fung J, Nguyen-Hoang L, Chaemsaithong P, Feng Q, et al. EP19.28: Assessment of the prognosis of the risk of preterm labour in the first trimester of pregnancy. Ultrasound in Obstetrics & Gynecology. 2023;62:228.
doi - Suntipap M, Keesukphan A, Rattnasiri S, Numthavaj P, Thakkinstian A. The association between cervical sonography and successful induction of labor: a systematic review and meta-analysis. Procedia of Multidisciplinary Research. 2023;1:6.
- Aimagambetova G, Atageldiyeva K, Marat A, Suleimenova A, Issa T, Raman S, Huang T, et al. Comparison of diagnostic accuracy and acceptability of self-sampling devices for human Papillomavirus detection: A systematic review. Prev Med Rep. 2024;38:102590.
doi pubmed - Khezri R, Askari S, Jahanian S, Ashayeri N. Preterm birth and public health challenges: Incidence and risk factors. Public Health. 2025;242:186-191.
doi pubmed - Shi Q, Wang Q, Tian S, Wang Q, Lv C. Assessment of different sonographic cervical measures to predict labor induction outcomes: a systematic review and meta-analysis. Quant Imaging Med Surg. 2023;13(12):8462-8477.
doi pubmed - Breve C, Santos GS. Impact of endometriosis on female fertility: evidence and challenges in Argentina. South Health and Policy. 2024;3:124.
doi - Hughes KM, Aberoumand M, Seidler AL, Swan P, Aboulghar M, de Lourdes Brizot M, Brock C, et al. Prognostic value of cervical length for spontaneous preterm birth in asymptomatic women with twin pregnancy: meta-analysis of individual participant data. BMJ Med. 2025;4(1):e000877.
doi pubmed - Fox C, Shennan A. Predicting preterm birth: an evolving landscape. BJOG. 2025;132(5):672-673.
doi pubmed - Rennert KN, Breuking SH, Schuit E, Bekker MN, Woiski M, de Boer MA, Sueters M, et al. Change in cervical length after arrested preterm labor and risk of preterm birth. Ultrasound Obstet Gynecol. 2021;58(5):750-756.
doi pubmed - Hessami K, D'Alberti E, Mascio DD, Berghella V. Universal cervical length screening and risk of spontaneous preterm birth: a systematic review and meta-analysis. Am J Obstet Gynecol MFM. 2024;6(5S):101343.
doi pubmed - Lim KI, Butt K, Nevo O, Crane JM. Guideline No. 401: sonographic cervical length in singleton pregnancies: techniques and clinical applications. J Obstet Gynaecol Can. 2020;42(11):1394-1413.e1391.
doi pubmed - David M, Devantery K, Nauche B, Chagnon M, Keezer M, Gaudreault N, Bureau NJ, et al. Ultrasound elastography of back muscle biomechanical properties: a systematic review and meta-analysis of current methods. Insights Imaging. 2024;15(1):206.
doi pubmed - Rizak VM, Al’-shoufi K, Rizak LM, Bokotey AA, Vysochanskii YM, Slivka VY. Thermal conduction of Sn(Pb)2P2S(Se)6-Like compounds. Ferroelectrics. 1997;192:167-175.
doi - Seol HJ, Sung JH, Seong WJ, Kim HM, Park HS, Kwon H, Hwang HS, et al. Standardization of measurement of cervical elastography, its reproducibility, and analysis of baseline clinical factors affecting elastographic parameters. Obstet Gynecol Sci. 2020;63(1):42-54.
doi pubmed - Park HS, Kwon H, Kwak DW, Kim MY, Seol HJ, Hong JS, Shim JY, et al. Addition of cervical elastography may increase preterm delivery prediction performance in pregnant women with short cervix: a prospective study. J Korean Med Sci. 2019;34(9):e68.
doi pubmed - Pizzella S, El Helou N, Chubiz J, Wang LV, Tuuli MG, England SK, Stout MJ. Evolving cervical imaging technologies to predict preterm birth. Semin Immunopathol. 2020;42(4):385-396.
doi pubmed - Miller T, Bello UM, Tsang CSL, Winser SJ, Ying MTC, Pang MYC. Using ultrasound elastography to assess non-invasive, non-pharmacological interventions for musculoskeletal stiffness: a systematic review and meta-analysis. Disabil Rehabil. 2024;46(16):3549-3563.
doi pubmed - Campo A, Mileydis D, Quevedo C. Towards respectful obstetric care. Nursing Depths Series, ISSN-e 3072-8118, No 3, 2024. (Ejemplar Dedicado a: Nursing Depths Series) 2024;3:1-3.
doi - Reicher L, Fouks Y, Yogev Y. Cervical assessment for predicting preterm birth-cervical length and beyond. J Clin Med. 2021;10(4):627.
doi pubmed - Lu H, Liu Y, Yang F, Wu D, Qi J, Ji Y, Hu M. The value of real-time shear wave elastography in spontaneous preterm birth. Medicine (Baltimore). 2024;103(33):e39288.
doi pubmed - Du L, Zhang LH, Zheng Q, Xie HN, Gu YJ, Lin MF, Wu LH. Evaluation of cervical elastography for prediction of spontaneous preterm birth in low-risk women: a prospective study. J Ultrasound Med. 2020;39(4):705-713.
doi pubmed - Mahdavi Sabet F, Forghani S, Shahsavand A, Kharaghani M, Samiee R, Kamali Hakim P, Zeinalkhani F. Diagnostic and clinical utility of ultrasound elastography for uterine cervical neoplasms-a comprehensive systematic review and meta-analysis. Abdom Radiol (NY). 2025.
doi pubmed - Iztleuov M, Kaliev A, Turganbaeva A, Yesmukhanova D, Akhmetova A, Temirbayeva A, et al. The effect of sodium tetraborate on chromium-induced oxidative damages in rats lung tissue. Biomedical and Pharmacology Journal. 2020;13:281-290.
doi - Atabayevna DZ. Isthmic-cervical insufficiency: as a cause of perinatal loss. World Bulletin of Public Health. 2022;8:171-173.
doi - Kavallaris A, Gkoutzioulis A, Zygouris D. Laparoscopic emergency cervicoisthmic cerclage in second trimester of pregnancy: a case series report. Eur J Obstet Gynecol Reprod Biol. 2021;256:184-188.
doi pubmed - Wierzchowska-Opoka M, Kimber-Trojnar Z, Leszczynska-Gorzelak B. Emergency cervical cerclage. J Clin Med. 2021;10(6):1270.
doi pubmed - Angelopoulou E, Gourounti K, Bolou A, Manesi M, Diamanti A. Cervical elastography as a predictive tool for preterm birth: a systematic review and meta-analysis. Cureus. 2025;17(9):e92505.
doi pubmed - Humberg A, Fortmann I, Siller B, Kopp MV, Herting E, Gopel W, Hartel C, et al. Preterm birth and sustained inflammation: consequences for the neonate. Semin Immunopathol. 2020;42(4):451-468.
doi pubmed - Gette F, Aziz Ali S, Ho MSP, Richter LL, Chan ES, Yang CL, Kieran E, et al. Long-term health outcomes of preterm birth: a narrative review. Front Pediatr. 2025;13:1565897.
doi pubmed - Cheong JLY, Burnett AC, Treyvaud K, Spittle AJ. Early environment and long-term outcomes of preterm infants. J Neural Transm (Vienna). 2020;127(1):1-8.
doi pubmed - A profile of prematurity of United States | PeriStats | March of Dimes n.d. https://www.marchofdimes.org/peristats/reports/united-states/prematurity-profile (Accessed May 21, 2025).
- Hu Q, Liao H, Yu H. Global burden of neonatal preterm birth: A systematic analysis for the global burden of disease study 2019. Public Health. 2025;238:162-172.
doi pubmed - Zhang L, Li J, Shang Y, Yang Q. The diagnostic value of transvaginal sonoelastography for cervical cancer and cervical intraepithelial neoplasia: a systematic review and meta-analysis. Eur J Med Res. 2025;30(1):516.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.