| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://jocmr.elmerjournals.com |
Original Article
Volume 17, Number 12, December 2025, pages 663-675
Prognostic Value of SIRS, SOFA, qSOFA, and LqSOFA in Emergency Department Sepsis Patients and Correlation of Cytokine Patterns With In-Hospital Mortality
Christos Davoulosa, Evangelos J. Giamarellos-Bourboulisb, Panagiotis Koufargyrisb, Charalambos Gogosa, Dimitrios Velissarisa, c
aUniversity of Patras, Patras, Greece
b4th Department of Internal Medicine, National and Kapodistrian University of Athens, Athens, Greece
cCorresponding Author: Dimitrios Velissaris, Department of Internal Medicine, University of Patras, Patras, Greece
Manuscript submitted July 30, 2025, accepted September 24, 2025, published online December 24, 2025
Short title: Clinical Scores and Cytokines Predict Mortality in Sepsis
doi: https://doi.org/10.14740/jocmr6340
| Abstract | ▴Top |
Background: Several prognostic scores and molecular patterns have been developed to predict increased in-hospital mortality in septic patients. This prospective study aimed to evaluate the prognostic value of systemic inflammatory response syndrome (SIRS), Sequential Organ Failure Assessment (SOFA), quick SOFA (qSOFA), lactate quick SOFA (LqSOFA) and cytokine production levels in emergency department sepsis patients to predict in-hospital mortality.
Methods: A total of 106 septic patients were enrolled. Baseline SOFA, SIRS, qSOFA and LqSOFA scores were calculated, and plasma levels of interleukin (IL)-6, IL-10, tumor necrosis factor-α (TNF-α) and interleukin-33 receptor (IL-33R) were measured on admission.
Results: SOFA, qSOFA, LqSOFA scores were significantly lower in sepsis survivors. IL-33R levels were significantly higher in non-survivors (P = 0.021). The best predictive score for sepsis based on the area under the receiver operating characteristic (ROC) curve was qSOFA (0.764, 95% confidence interval (CI) = 0.663 - 0.866), followed by LqSOFA (0.738, 95% CI = 0.63 - 0.845), SOFA (0.713, 95% CI = 0.604 - 0.822) and SIRS (0.603, 95% CI = 0.478 - 0.729). The addition of IL-33R levels (cut-off values > 55,393 pg/mL) to qSOFA and SOFA significantly increased the diagnostic accuracy of both scores with area under the curve (AUC) of 0.78 (95% CI = 0.695 - 0.85) and 0.740 (95% CI = 0.636 - 0.844), respectively. When evaluating early (within 72 h) in-hospital mortality, both IL-10 and IL-33R were significantly higher in non-survivors (124 pg/mL vs. 41 pg/mL in survivors, 195,610 pg/mL vs. 62,767 pg/mL in survivors, respectively). When added to qSOFA and SOFA scores (cut-off levels 74.5 pg/mL and 55,393 pg/mL for IL-10 and IL-33R, respectively), they significantly increased their diagnostic accuracy.
Conclusions: Sepsis prognostic scores were significantly lower in sepsis survivors. IL-10 levels had a significant impact in predicting early (within 72 h) in-hospital mortality and IL-33R levels in predicting both early and total in-hospital mortality, especially when combined with SOFA and qSOFA scores.
Keywords: Sepsis; Mortality; Cytokines; SOFA; qSOFA
| Introduction | ▴Top |
Sepsis is a preventable, life-threatening syndrome caused by an infection and is responsible for 11 million deaths worldwide, accounting for about 20% of all global deaths [1]. Furthermore, mortality rates for hospital-treated sepsis cases and intensive care unit (ICU)-treated sepsis cases are 24% and 42%, respectively, with significant disparities between low-, medium- and high- income countries [1, 2]. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) has readdressed sepsis definition as a life-threatening organ dysfunction caused by a dysregulated host response to an infection, abating older definitions that focused solely on inflammatory excess [3, 4]. The balance between pro and anti-inflammatory response is crucial for sepsis survival. This balance is influenced by host factors such as age, underlying comorbidities, and pathogen virulence, with cytokines contributing to the immune response [5, 6]. As our understanding of the complex molecular interactions between different pathways in sepsis grows, there is urgent need for earlier detection and targeted therapies based on cytokine profile. In the past few years, several clinical scores for sepsis identification and risk stratification have been investigated, with an emphasis on earlier sepsis detection and appropriate treatment. Some, such as quick Sequential Organ Failure Assessment (qSOFA), rely on clinical parameters aiding early detection in the emergency department, while others, such as SOFA score, lactate qSOFA (LqSOFA), systemic inflammatory response syndrome (SIRS) or National Early Warning Score (NEWS), incorporate both clinical and microbiological parameters [7-11]. The aim of this study is to evaluate the prognostic value of SIRS, SOFA, qSOFA and LqSOFA as prediction scores in emergency department sepsis patients and to investigate the immune-mediated response by measuring cytokine production patterns and their correlation with in-hospital mortality.
| Materials and Methods | ▴Top |
Study selection and inclusion criteria
In this prospective cohort study carried out between June 2019 and April 2020, we evaluated septic patients who presented to the emergency department unit of a tertiary hospital in Patras, Greece. All patients enrolled in the study fulfilled the international criteria for sepsis (Sepsis-3 definitions). Inclusion criteria were adults with radiological, microbiological or clinically documented infections and sepsis according to Sepsis-3 definition. Patients with missing clinical, microbiological data or missing blood samples were excluded. Out of 136 patients presenting to the emergency room (ER), 30 patients were excluded, leaving 106 patients for evaluation. Demographic characteristics, comorbidities, type of infection, clinical severity scores, and patients’ outcome were documented on admission. As for LqSOFA score, we developed binary (0 for a lactate point-of-care concentration < 2 mmol/L and 1 for a lactate concentration > 2 mmol/L) lactate scores to be added to qSOFA score. The aim of the study was to examine the potential role of both pro- and anti-inflammatory biomarkers in predicting in-hospital mortality and to assess their concentrations during the sepsis process. Interleukin (IL)-6, tumor necrosis factor-α (TNF-α), known pro-inflammatory cytokines, IL-10, an anti-inflammatory cytokine, and interleukin-33 receptor (IL-33R) with mixed actions depending on microenvironment, were studied. Furthermore, we combined IL-33R and IL-10 semiquantitative levels (using cutoff values derived from the Youden Index) with several scores by adding one point in each score if the IL’s level exceeded the cutoff. BacTAlert and Vitek 2 (bioMerieux) systems were used for performing the cultures, identifying the bacterial isolates and testing the antibiotic susceptibility. Plasma samples were collected upon admission, and cytokine levels were measured in pg/mL. Enzyme-linked immunosorbent assay (ELISA) kits from Diaclone (France) were used to measure IL-6, IL-10, and TNF-α levels, while soluble suppression of tumorigenicity 2 (sST2)/sIL-33R levels were measured using an ELISA kit from R&D Systems (USA).
Ethical statement
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by the Institutional Ethics Board of University Hospital of Patras (approval code: 457/11-7-2019).
Data analysis
Data analysis was performed using descriptive statistic tools. Categorical data were presented as frequencies and group percentages whereas continuous data with normal and skewed distributions as mean ± standard error (SE) and medians, respectively. Chi-square test was used for comparison of categorical data whereas Mann-Whitney U test was used for comparison of skewed continuous data, and data normality was assessed using the Kolmogorov-Smirnov and Shapiro-Wilk tests using a P value of 0.05. Furthermore, Spearman’s rank correlation coefficient was used to assess monotonic relationships between continuous and discrete ordinal variables, while receiver operating characteristic (ROC) analysis was used to evaluate the performance of various scoring systems and biomarkers in discriminating those with largest probability to die from sepsis. In order to compare the respective powers of prediction for several scores and biomarkers, the area under the curve (AUC) was compared for each ROC curve. The best cutoff point for each index was determined by the Youden Index, which maximizes sensitivity and specificity for a continuous variable to create a dichotomous value by taking the sensitivity + the specificity - 1 and choosing the maximum value. All tests were two-tailed, and statistical significance was considered for P values < 0.05. Analyses were performed by using Statistical Package for the Social Sciences software (SPSS for Windows-version 28.0 SPSS Inc., Chicago, IL, USA) and GraphPad Prism 8 software.
| Results | ▴Top |
A total of 106 patients suffering from sepsis according to Sepsis-3 definitions were included in the study. Among them, 46 patients suffered from lower respiratory tract infection, 24 suffered from urinary tract infection, eight from biliary tract infection, five from intestinal infection, three from central nervous system (CNS) infection while the rest suffered from mixed (18 patients: urinary/respiratory tract infections etc.). Additionally, 18 patients had concurrent bacteremia. Of the 106 patients, 80 patients survived while the rest 26 patients died. The two groups (survivors, non-survivors) did not differ in age, comorbidities, white blood cell (WBC), lactate, C-reactive protein (CRP) values on admission (Table 1). All patients were treated according to the newest sepsis guidelines with broad spectrum antibiotics, crystalloids and inotropes if needed. No patient underwent parenteral nutrition.
 Click to view | Table 1. Study Population Demographics and Baseline Characteristics |
We assessed the prognostic value of several scoring systems calculated on patients’ admission in predicting hospital sepsis mortality. Survivors had significantly lower SOFA, qSOFA, and LqSOFA scores than non-survivors, while both groups did not differ in SIRS scores. Moreover, there was a statistically higher in-hospital mortality in female patients (P = 0.023).
We also evaluated systemic inflammatory response in sepsis patients by measuring several pro- and anti-inflammatory cytokines and their association with in-hospital mortality. Levels of pro-inflammatory cytokines IL-6 and TNF-α, anti-inflammatory mediator IL-10 and the IL-6/IL-10 ratio did not differ significantly between survivors and non-survivors. In contrast, IL-33R levels were significantly higher in the group of non-survivors (P = 0. 021) (Fig. 1). Moreover, we evaluated the role of these biomarkers in predicting early (within 72 h) in-hospital mortality. Both IL-10 and IL-33R levels were higher in non-survivors (124 pg/mL vs. 41 pg/mL in survivors, 195,610 pg/mL vs. 62,767 pg/mL in survivors, respectively), whereas IL-6 and TNF-α levels were not statistically different (Fig. 2). We also performed correlation assays between prognostic scores and molecular inflammatory patterns on admission. Although significant positive correlations were observed between most prognostic scores and cytokines, only SOFA and qSOFA with IL-33R correlation indicated a moderate effect size (r = 0.46, (P < 0.001, 95% CI = 0.28 - 0.61), r = 0.4, (P < 0.001, 95% CI = 0.23 - 0.56), respectively).
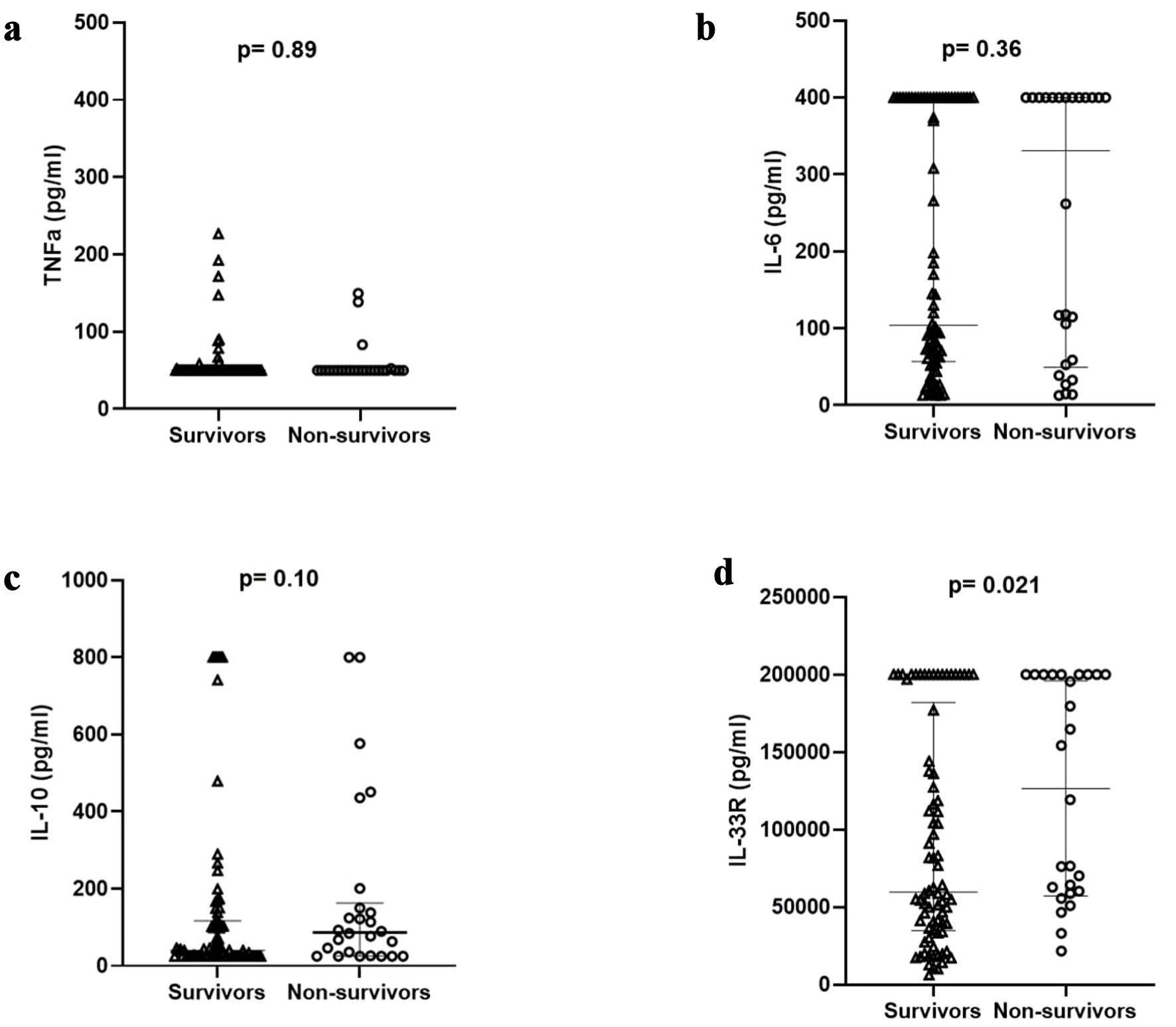 Click for large image | Figure 1. Cytokine differences regarding outcome in study population. TNF: tumor necrosis factor; IL: interleukin; IL-33R: interleukin-33 receptor. |
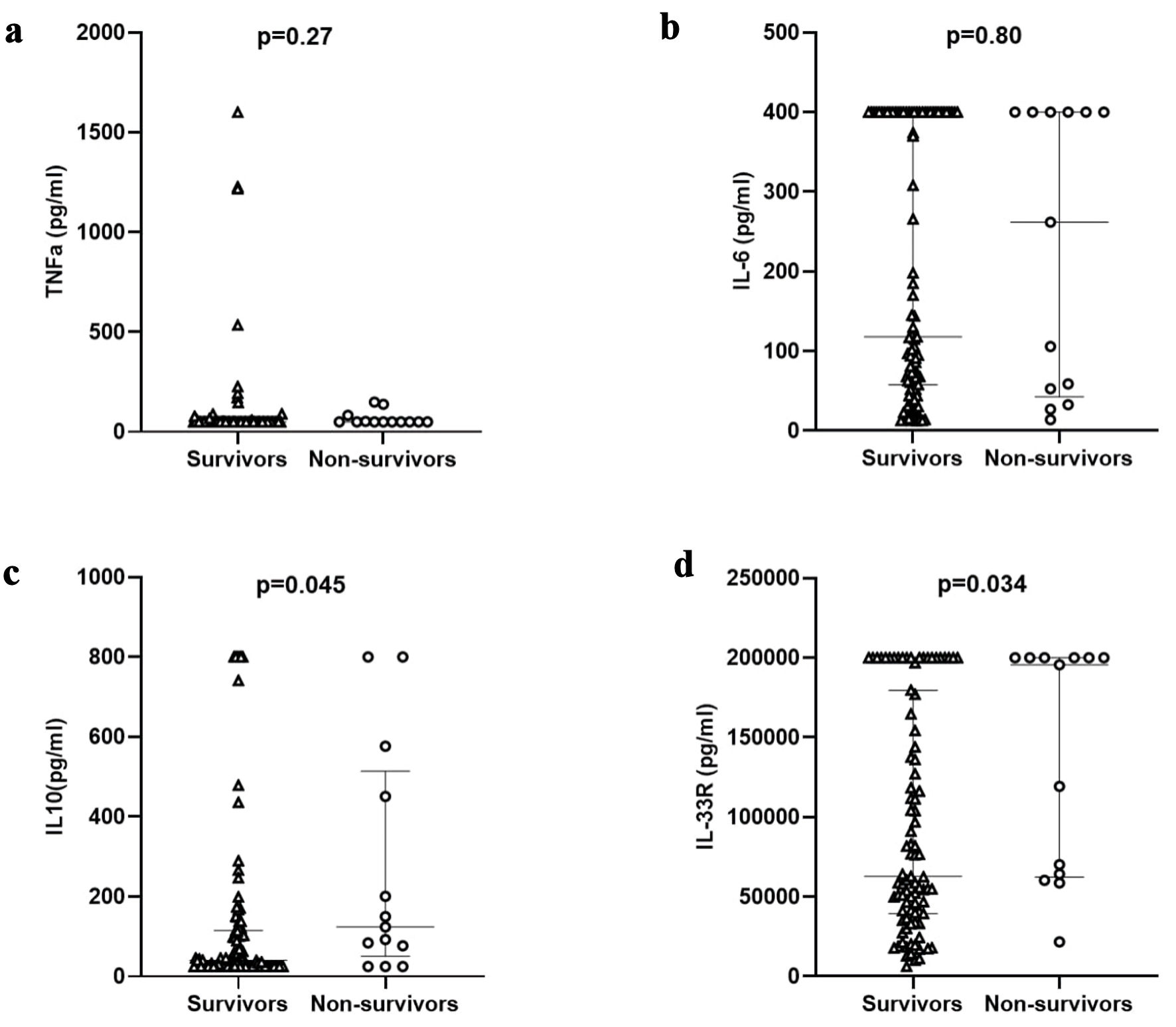 Click for large image | Figure 2. Cytokine differences regarding early outcome (in 72 h) in study population. TNF: tumor necrosis factor; IL: interleukin; IL-33R: interleukin-33 receptor. |
Prognostic value of severity scores and molecular mediators for in-hospital mortality
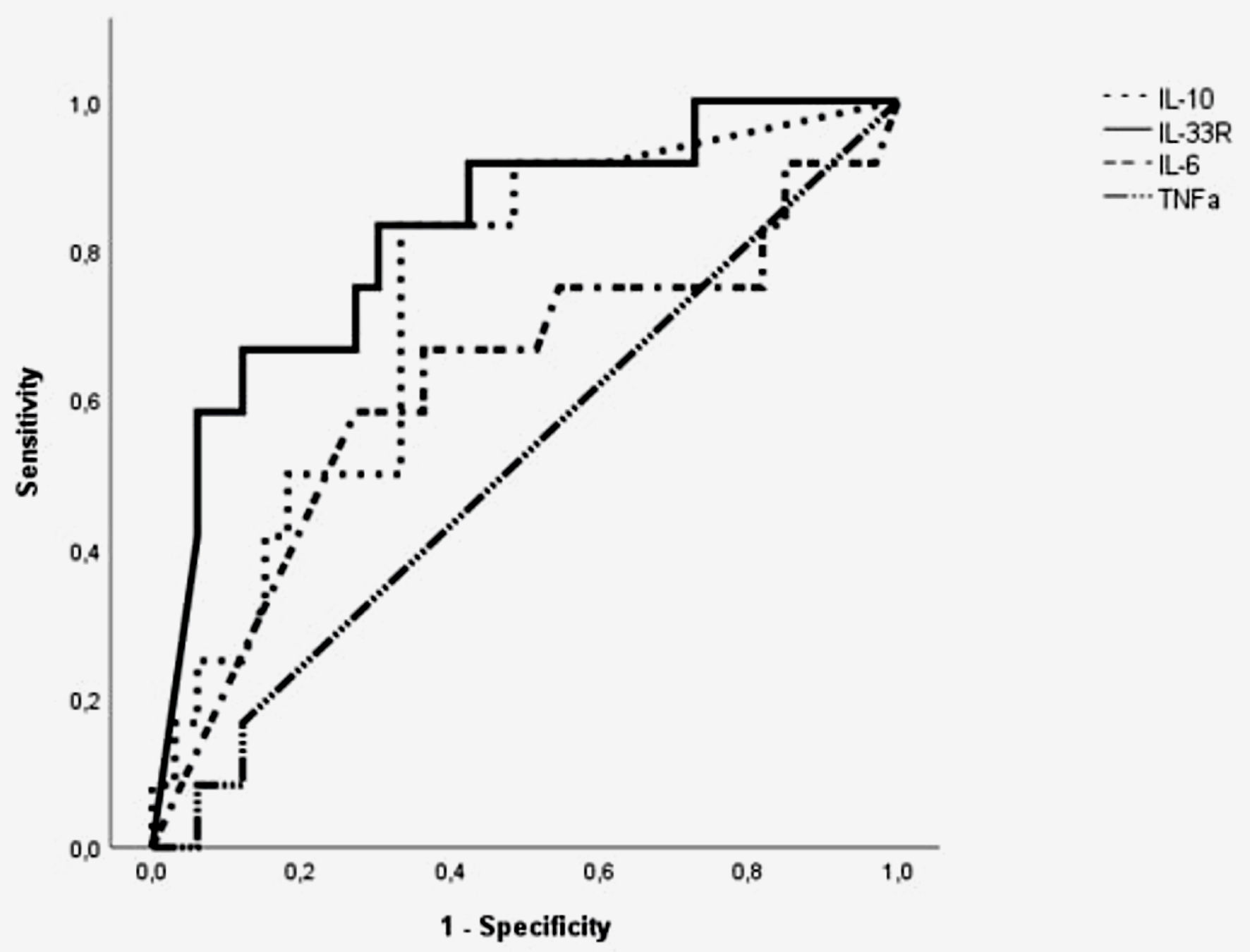
To further assess the value of several prognostic scores and molecular patterns on admission as predictors for in-hospital mortality, ROC were analysed. Figure 3 presents AUCs, sensitivity and specificity in predicting in-hospital mortality for various molecular mediators and prognostic scores. The best predictive score based on the area under the receiver operating curve was qSOFA (0.764, 95% CI = 0.663 - 0.866), followed by LqSOFA (0.738, 95% CI = 0.63 - 0.845), SOFA (0.713, 95% CI = 0.604 - 0.822) and SIRS (0.603, 95% CI = 0.478 - 0.729). Using the Youden index, the optimal cutoff values of SIRS, SOFA, qSOFA, and LqSOFA were > 2, > 3, > 1 and > 2, respectively, in which specificity was 63.7%, 57.5%, 63.7%, and 77.5%, while sensitivity was 57.7%, 81%, 84.6% and 65.4%, respectively, although for SIRS as a prognostic score the P value was not significant (P = 0.1). To assess the diagnostic performance of IL-6, IL-10, TNF-α and IL-33R levels on admission in identifying mortality risk for patients with sepsis, ROC curves were also built. Between all mediators studied, only IL-33R had a moderate although significant prognostic value for in-hospital mortality with a cutoff level of 55,393 pg/mL (sensitivity 84.6%, specificity 46.2%) and an AUC of 0.65 (95% CI = 0.538 - 0.762). Furthermore, the addition of IL-33R levels (cutoff values > 55,393 pg/mL) to qSOFA and SOFA scores (added 1 point in each score with IL’s levels above cutoff) significantly increased the diagnostic accuracy of both individual tests with AUC of 0.781 (95% CI = 0.679 - 0.88) and 0.740 (95% CI = 0.636 - 0.844), respectively (Fig. 3). Moreover, when adjusting for early (72 h) in-hospital mortality, only IL-10 and IL-33R had a moderate although significant prognostic value in predicting early in-hospital mortality with cutoff levels of 74.5 pg/mL (sensitivity 77%, specificity 65%) and AUC 0.67 (95% CI = 0.5 - 0.84) for IL-10 and cutoff levels of 55,393 pg/mL (sensitivity 92.3%, specificity 43%) and AUC 0.68 (95% CI = 0.54 - 0.82) for IL-33R. Interestingly, the addition of both IL-10 (cutoff levels 74.5 pg/mL) and IL-33R (cutoff levels 55,393 pg/mL) increased the diagnostic accuracy of both SOFA and qSOFA tests in predicting early in-hospital mortality. More precisely, the addition of IL-10 to SOFA and qSOFA increased the models’ AUC from 0.83 (95% CI = 0.714 - 0.94) to 0.85 (95% CI = 0.73 - 0.96), and from 0.79 (95% CI = 0.67 - 0.9) to 0.83 (95% CI = 0.7 - 0.95), respectively. Similarly, the addition of IL-33R to SOFA and qSOFA further increased the models’ AUC from 0.83 to 0.85 (95% CI = 0.75 - 0.94) and from 0.79 to 0.81 (95% CI = 0.7 - 0.92), respectively (Fig. 4). Furthermore, due to the conflict around the poor sensitivity of qSOFA in predicting early sepsis mortality, we evaluated the possible role of IL-33R as an adjunctive tool, especially in patients having qSOFA scores of 0 or 1. In this group of patients, IL-33R levels were similar between survivors and non-survivors (median values of 54,124 pg/mL in the former and 51,091 pg/mL in the latter).
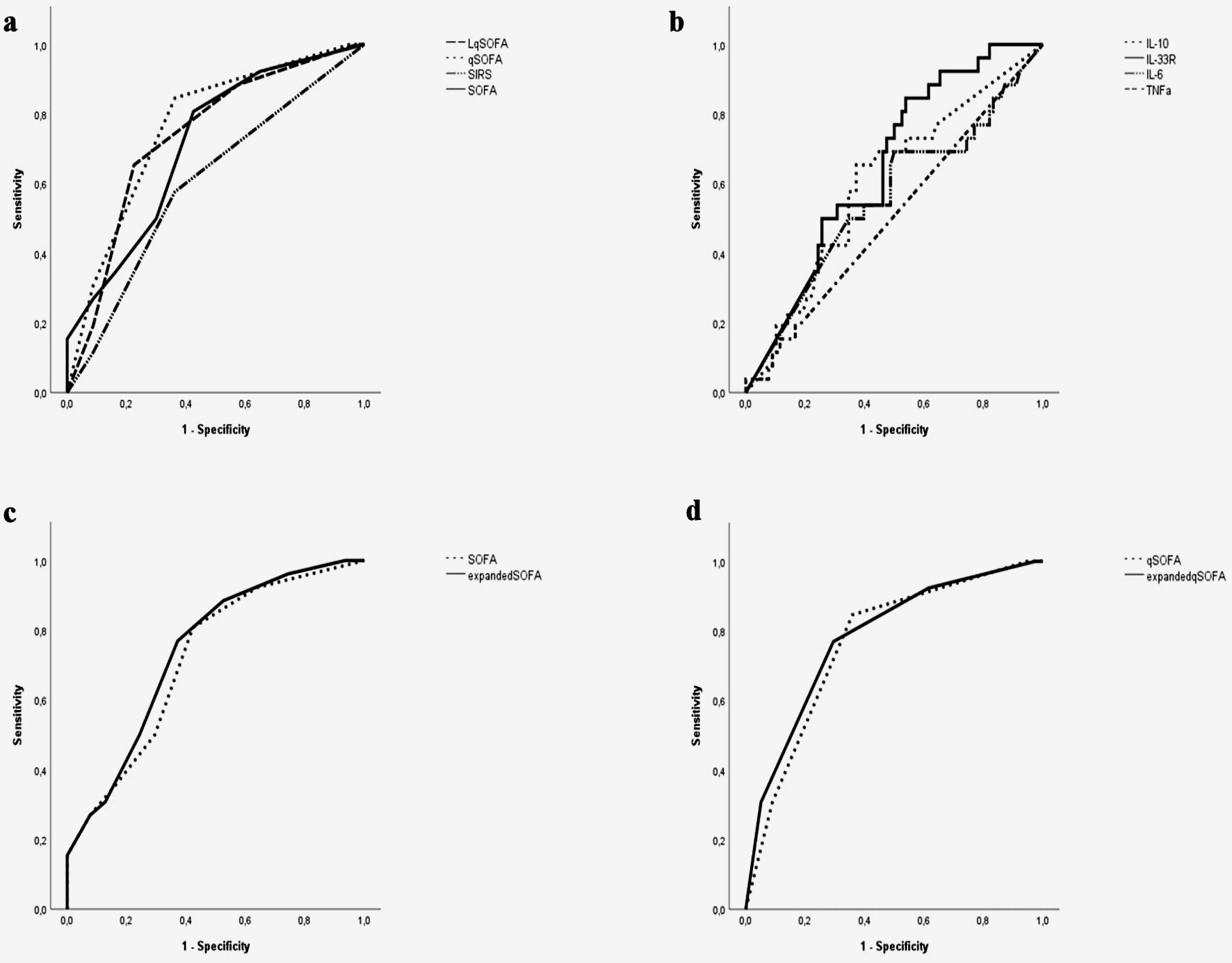 Click for large image | Figure 3. The area under the receiver operating characteristic (ROC) curve of SIRS, SOFA, qSOFA, and LqSOFA (a), IL-6, IL-10, TNF-α, IL-33R (b), expanded SOFA-IL-33R (SOFA combined with cutoff value of IL-33R) and expanded qSOFA-IL-33R (qSOFA combined with cutoff value of IL-33R) scores (c, d), respectively, in predicting in-hospital mortality of sepsis patients. LqSOFA: lactate quick SOFA; qSOFA: quick SOFA; SIRS: systemic inflammatory response syndrome; SOFA: Sequential Organ Failure Assessment; TNF: tumor necrosis factor; IL: interleukin; IL-33R: interleukin-33 receptor. |
 Click for large image | Figure 4. The area under the receiver operating characteristic (ROC) curve of expanded SOFA-IL-33R (SOFA combined with cutoff value of IL-33R) (a), expanded qSOFA-IL-33R (qSOFA combined with cutoff value of IL-33R) (b), expanded SOFA-IL-10 (SOFA combined with cutoff value of IL-10) (c) and expanded qSOFA-IL10 (qSOFA combined with cutoff value of IL-10) (d) in predicting early (within 72 h) in-hospital mortality of sepsis patients. qSOFA: quick SOFA; SOFA: Sequential Organ Failure Assessment; IL-33R: interleukin-33 receptor. |
Interestingly, we conducted a subgroup analysis examining the prognostic significance of different biomarkers and severity scores in patients with lower respiratory tract infections. Of the 46 septic patients suffering from lower respiratory tract infections, 34 were finally discharged from hospital. Of all cytokines studied (IL-6, IL-10, TNF-α, IL-33R), only IL-33R correlated significantly with in-hospital mortality in this group of patients (median levels of 159,540 pg/mL in non-survivors, 100,590.5 pg/mL in survivors, P < 0.01). Survivors had also significantly lower SOFA, qSOFA, LqSOFA scores than non-survivors, while both groups did not differ in SIRS score. Moreover, to assess the values of these prognostic scores and molecular patterns on admission as predictors for in-hospital mortality in this group of patients, we conducted ROC analysis. In accordance with the study population, IL-10 and IL-33R had a significant prognostic value in predicting in-hospital mortality with cutoff levels of 68.5 pg/mL (sensitivity 83%, specificity 67%) and AUC 0.74 (95% CI = 0.58 - 0.89) for IL-10, and cutoff levels of 57,415 pg/mL (sensitivity 83%, specificity 70%) and AUC 0.82 (95% CI = 0.68 - 0.96) for IL-33R. Interestingly, the addition of IL-33R levels (cutoff values > 57,415 pg/mL) to qSOFA, LqSOFA and SOFA scores significantly increased the diagnostic accuracy of all three individual tests, with AUC 0.902 (95% CI = 0.81 - 0.99), 0.95 (95% CI = 0.89 - 1) and 0.905 (95% CI = 0.81 - 1), respectively (Figs. 5-9).
 Click for large image | Figure 5. The area under the receiver operating characteristic (ROC) curve of IL-6, IL-10, TNF-α, IL-33R in predicting in-hospital mortality of sepsis patients with lower respiratory tract infections. TNF: tumor necrosis factor; IL: interleukin; IL-33R: interleukin-33 receptor. |
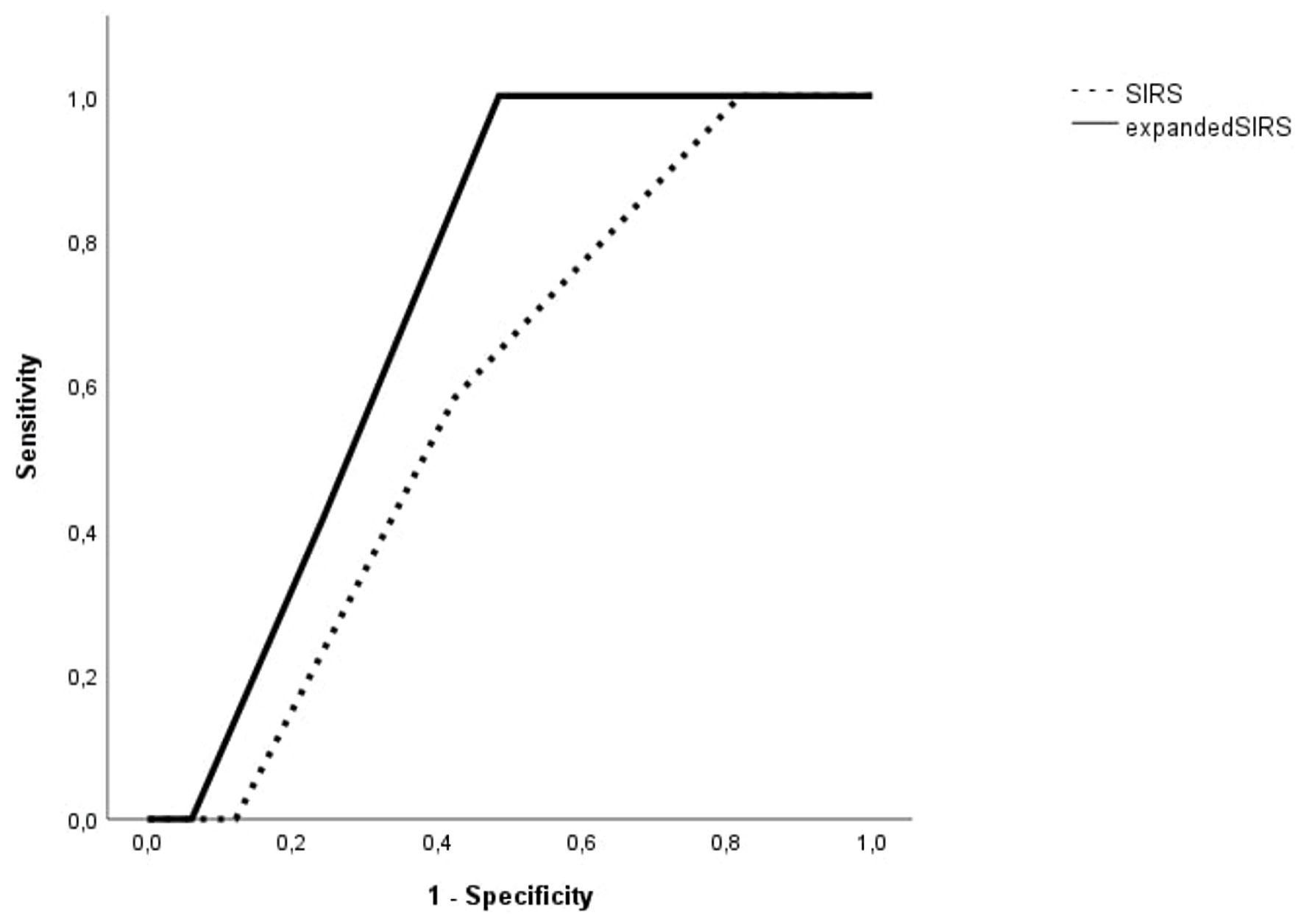 Click for large image | Figure 6. The area under the receiver operating characteristic (ROC) curve of SIRS and expanded SIRS (SIRS combined with cutoff value of IL-33R) in predicting in-hospital mortality of sepsis patients with lower respiratory tract infections. SIRS: systemic inflammatory response syndrome; IL-33R: interleukin-33 receptor. |
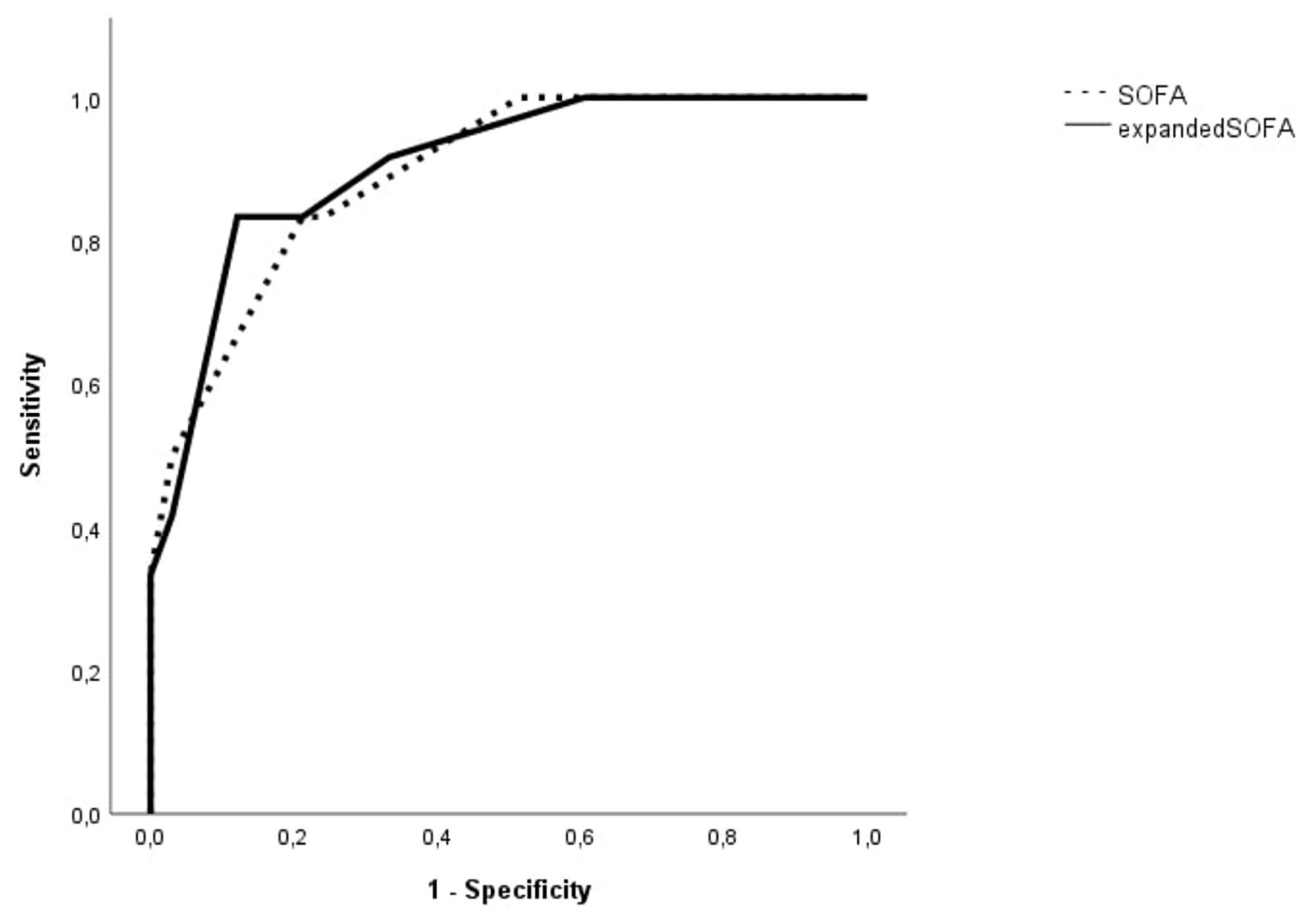 Click for large image | Figure 7. The area under the receiver operating characteristic (ROC) curve of SOFA and expanded SOFA (SOFA combined with cutoff value of IL-33R) in predicting in-hospital mortality of sepsis patients with lower respiratory tract infections. SOFA: Sequential Organ Failure Assessment; IL-33R: interleukin-33 receptor. |
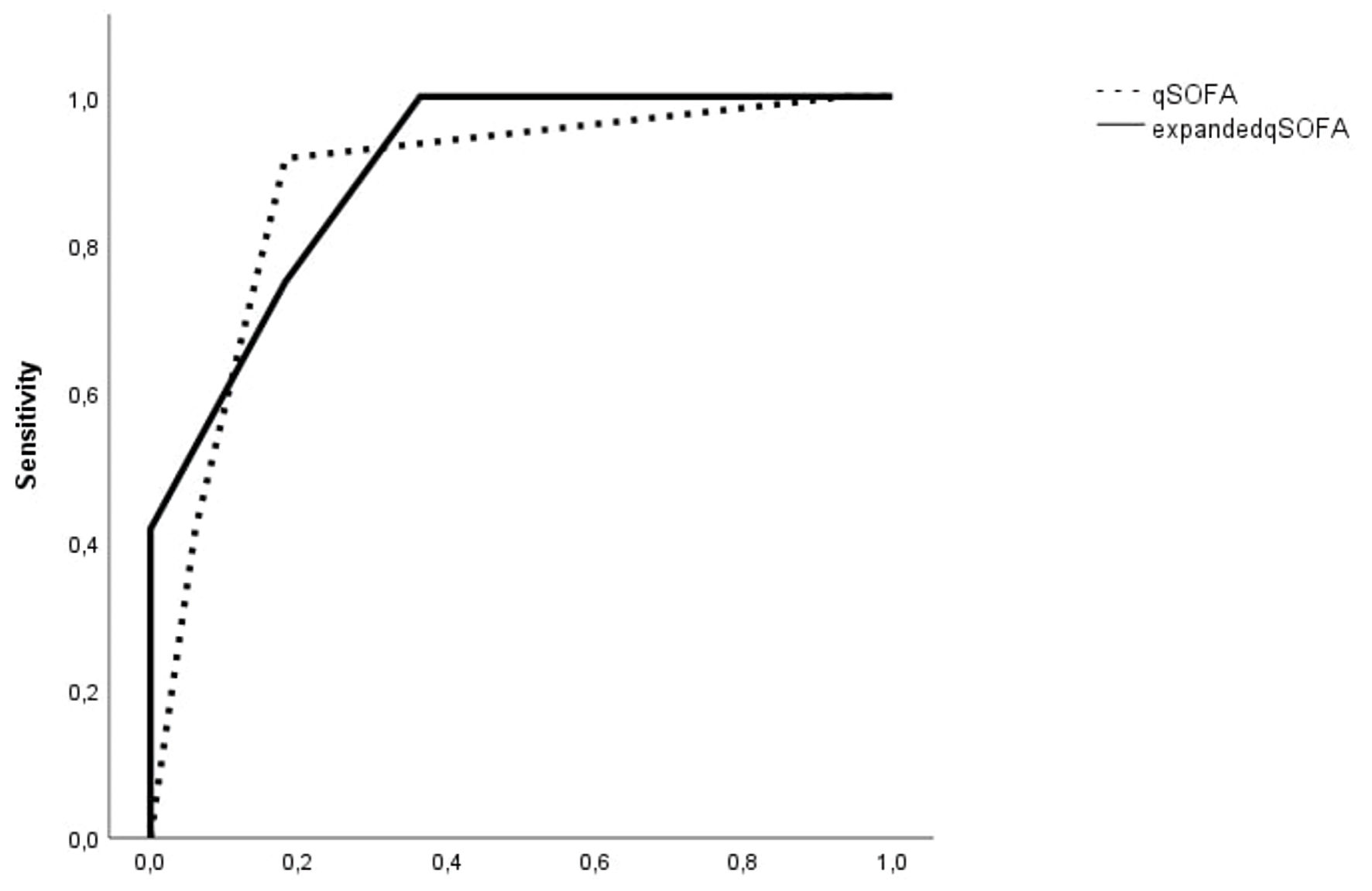 Click for large image | Figure 8. The area under the receiver operating characteristic (ROC) curve of qSOFA and expanded qSOFA (qSOFA combined with cutoff value of IL-33R) in predicting in-hospital mortality of sepsis patients with lower respiratory tract infections. qSOFA: quick SOFA; SOFA: Sequential Organ Failure Assessment; IL-33R: interleukin-33 receptor. |
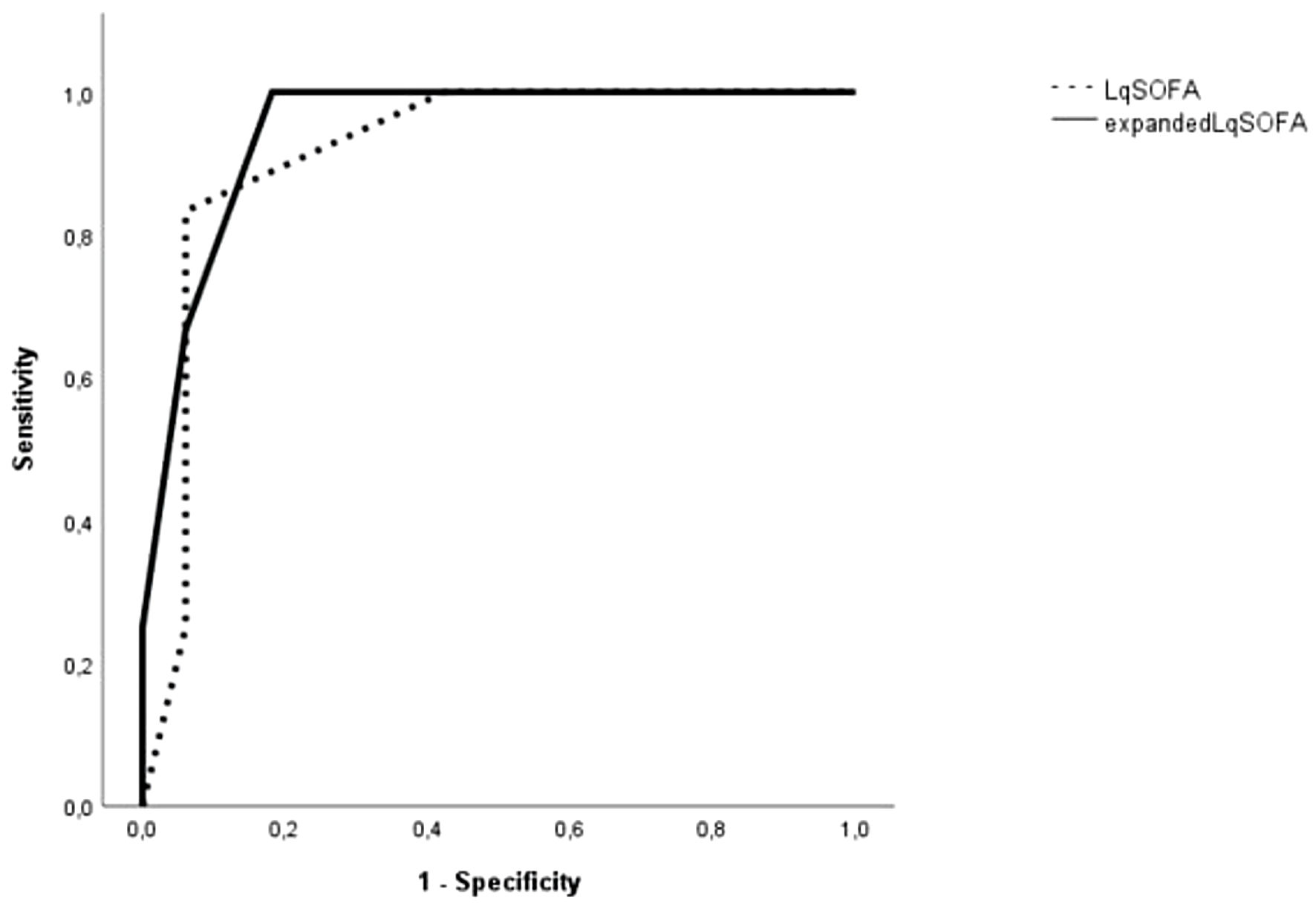 Click for large image | Figure 9. The area under the receiver operating characteristic (ROC) curve of LqSOFA and expanded LqSOFA (LqSOFA combined with cutoff value of IL-33R) in predicting in-hospital mortality of sepsis patients with lower respiratory tract infections. LqSOFA: lactate quick SOFA; SOFA: Sequential Organ Failure Assessment; IL-33R: interleukin-33 receptor. |
| Discussion | ▴Top |
Sepsis remains a major global health issue, contributing to substantial morbidity and mortality, particularly without early detection. Dysregulated immune response is a key factor in sepsis pathophysiology and raises the need for accurate diagnostic tools to guide management.
Severity scores and mortality prediction
We evaluated the performance of several commonly used severity scores in predicting in-hospital mortality in sepsis patients. SOFA, qSOFA and LqSOFA were all significant predictors of in-hospital mortality whereas SIRS failed to predict in-hospital mortality, which aligns with previous studies indicating its limited utility in sepsis risk stratification. The best predictive score was qSOFA, followed by LqSOFA and SOFA using ROC analysis, with qSOFA having greater sensitivity (84.6% for qSOFA > 1 in comparison to 81% for SOFA > 3), although for qSOFA values > 2 sensitivity drops to about 31% underscoring the score’s limited ability to capture all at-risk patients, particularly those in early stages of sepsis or with non-severe manifestations. This is in accordance with a retrospective validation of the Sepsis-3 definitions, which raises concerns about the prognostic value of qSOFA for sepsis patients outside ICU due to its poor sensitivity [11]. The Third International Consensus for Sepsis and Septic Shock added qSOFA as a useful tool for early discrimination of patients with sepsis requiring more intensive care using only clinical criteria, making it an important adjunct for resource low settings [4, 9]. However, many patients, especially young, did not meet the threshold of two points in qSOFA scale and failed to be classified as septic, wasting an important amount of time in sepsis treatment, which led to abandonment of qSOFA in 2021 Sepsis Guidelines as a single diagnostic sepsis score and favored other scores such as SOFA or NEWS [12]. To overcome low sensitivity, there were studies combining lactate point-of-care values with qSOFA to enhance bedside mortality prediction. A prospective cohort study in southeast Asia concluded that combination identified patients at risk for sepsis-related mortality with better accuracy than qSOFA alone and with similar accuracy as SOFA score [10]. That has been also confirmed by a systematic review, which included 11 studies - most of which indicated an increase in the area under the receiver operating characteristic (AUROC) curve for qSOFA with the addition of lactate mainly in the emergency department [13]. In contrast, in our study, combination of binary lactate (> 2 mmol) values with qSOFA did not lead to better predicting ability than qSOFA alone, although it was an adequate predictor of mortality with higher values in non-survivors.
Cytokines and the immune response
The aim of this study was also to investigate the immune-mediated response of sepsis patients who presented to the emergency department by measuring several cytokine levels and their predicting ability of in-hospital mortality. Inflammatory response is guided primarily by cytokines such as IL-1b, IL-6, IL-8, TNF-α, and interferon (IFN)-γ, which are produced by monocytes, macrophages, endothelial cells, epithelial cells and provoke immune cell activation through intracellular signalling. Meanwhile, there are some other cytokines, such as IL-33 with its soluble receptor IL-33R (sST) that exert both pro- and anti-inflammatory responses.
Sepsis pathogenesis involves identification of pathogen-associated molecular patterns (PAMPs) by pattern recognition receptors, which drive complex reactions such as cellular modifications, microcirculation and coagulation cascade dysregulation and disrupted host immune reactions with concomitant pro- and anti-inflammatory responses [14]. As Karakike et al showed, excessive host pro-inflammatory responses can lead to abrupt inflammation syndromes such as macrophage activation syndrome (MAS) with greater mortality [15]. Meanwhile, excessive immunoparalysis through alterations in both innate and adapted immune system leads also to endotoxin tolerance and higher sepsis mortality [16-18].
Over the past years, there have been a lot of studies on molecular patterns of sepsis, with earlier research focusing on the pro-inflammatory aspect, whereas more recent ones on the disequilibrium between pro- and anti-inflammatory patterns, as indicated in the latest sepsis guidelines [12, 19]. Most of these studies used pro-inflammatory cytokines such as IL-1, IL-6 or TNF-α, anti-inflammatory cytokines such as IL-10 or pro- to anti-inflammatory ratios such as IL-10 to TNF-α ratio to assess patient’s immune reaction [20-22]. Furthermore, there have been studies examining potential targets for immune intervention interfering with the molecular cascade in sepsis such as IL-6 blockade in coronavirus disease 2019 (COVID-19) patients with hyperinflammatory syndrome or anakinra in sepsis patients with macrophage activation-like syndrome [23, 24]. In our study, none of the IL-6, IL-10, TNF-α or IL-6/IL-10 ratio was significant mortality predictor in sepsis patients, which contrasts with other studies. This is mainly explained by our small sample size (n = 106) and small number of non-survivors (26 patients). Except from these molecular markers, some studies examined the role of IL-33/suppression of tumorigenicity-2 (ST2) axis. IL-33, a member of IL-1 family, is produced by both structural and immune cells and acts through its ligation with ST2 receptor or with the receptor for advanced glycation end products (RAGE), depending on which IL-33 form circulates in plasma, reduced or oxidized. ΙL-33 interaction with its receptors exerts diverse roles depending on microenvironment and type of cells expressed, both producing pro-inflammatory response and contributing to immunosuppression [5, 6, 25-27]. In contrast, soluble IL-33R (sST2) acts as a decoy receptor for IL-33 and functions as an inhibitor of the IL-33/ST2 pathway. IL-33 levels rise in many inflammatory conditions, such as asthma, chronic obstructive pulmonary disease (COPD), autoimmune diseases, acute lung injury such as in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, with many preclinical studies suggesting a beneficial effect of IL-33/ST2 blockade in asthma or acute lung injury patients [28-31]. To date, there are many clinical studies under development testing the efficiency of tozorakimab, an anti-IL-33 antibody that inhibits IL-33 signalling via ST2 and RAGE/EGFR pathways, in reducing inflammation and epithelial dysfunction in patients with acute respiratory failure (phase 3 - NCT05624450) and in COPD patients (phase 3 - NCT05166889 and NCT05158387) [27].
Moreover, there is a lot of evidence highlighting the role of IL-33R (sST2) as a useful predictor of sepsis severity and mortality, although some studies such as that conducted by Parenica et al, failed to indicate similar predicting ability [32-34]. In our study, we examined serum IL-33R concentrations alone or in combination with sepsis severity scores on admission as in-hospital mortality predictors. We found that IL-33R levels on admission were significantly higher in non-survivors than in sepsis survivors (median 136,800 pg/mL vs. 59,693 pg/mL) and had a moderate to strong positive correlation with sepsis predicting scores such as SOFA, qSOFA and LqSOFA. Furthermore, although IL-33R levels were moderate predictors of in-hospital mortality (AUC of 0.65), when used adjunctively to sepsis severity scores, it augmented the diagnostic accuracy of both qSOFA and SOFA, with AUC of 0.78 (95% CI = 0.679 - 0.88) and 0.74 (95% CI = 0.636 - 0.844), respectively. That would have clinical implications as a new score including qSOFA and bedside IL-33R semi quantitative measurement (cutoff > 55,393 pg/mL) could identify earlier sepsis patients before deteriorating, augmenting qSOFA sensitivity at cutoff values > 1 (0.92 vs. 0.85). Due to the need to identify patients at risk of early deterioration, we evaluated the possible role of those biomarkers in predicting early (within 72 h) in-hospital mortality. Except for IL-33R levels, IL-10 levels were significantly higher in non-survivors, which is interesting because IL-10 is an anti-inflammatory biomarker, pointing towards an early immunosuppressive phenotype in those patients. Similarly, both IL-10 and IL-33R (with cutoff levels of 74.5 pg/mL and 55,393 pg/mL, respectively) could be combined to qSOFA and SOFA to further augment the diagnostic accuracy of those scores to predict early (within 72 h) in-hospital mortality. However, when performing a subgroup analysis for patients with qSOFA scores of 0 or 1 trying to augment qSOFA predictive mortality in low-risk patients, we found that IL-33R levels were similar, although this could be explained by the small subgroup size (54 patients).
Subgroup analysis and respiratory infections
Furthermore, we conducted a subgroup analysis for patients with lower respiratory infections. Hincapie et al evaluated the role of several prognostic scores in patients with respiratory infections, such as NEWS, Modified Early Warning Score (MEWS) and qSOFA in predicting in-hospital mortality. NEWS and MEWS were the best prognostic scores with AUC of 0.75 and 0.73, respectively [35]. Similarly, Fan et al compared Acute Physiology Score III (APSIII) and Logical Organ Dysfunction System (LODS) to SOFA score in sepsis patients with acute respiratory failure concluding that the former (APSIII and LODS) had better predicting ability for in-hospital mortality [36]. In our study, IL-33R had significantly better prognostic ability in patients with lower respiratory infections than in study population, and it had a significant impact when combined to usual scores such as qSOFA, LqSOFA and SOFA scores. Notably, qSOFA and LqSOFA were better predicting scores than SOFA in this subgroup of patients. This could be explained by the addition of respiratory rate as a factor in qSOFA and LqSOFA scores, which is usually elevated in such patients. What is more, the SOFA score contains indicators reflecting laboratory parameters such as bilirubin or platelet count, which are not often affected, as well as measures of hemodynamic instability, which is also not commonly observed in this subgroup of patients.
Study limitations
Our study has a few limitations. First, the small sample size and number of non-survivors did not allow us to have stronger results when comparing various cytokine levels. Furthermore, it was a single-center study with our study group comprising mainly from patients suffering from respiratory infections, which limits the generalizability of our findings to broader populations or other types of infections. Further large prospective studies are needed before incorporating novel biomarkers such as IL-33R into clinical practice either as mortality predictors or as immune targets for therapeutic reasons.
Conclusions
SOFA, qSOFA, and LqSOFA were all strong predictors of in-hospital mortality in patients suffering from sepsis with higher scores correlating better with higher IL-6, IL-10 and IL-33R levels. Furthermore, both IL-10 and IL-33R levels were adequate predictors of early (both) and in-hospital mortality (the latter) when used alone or as an adjunct to qSOFA or SOFA. Quick bedside assessment of IL33R could aid in earlier discrimination of septic patients particularly when combined to qSOFA.
Acknowledgments
The publication fees of this manuscript have been financed by the Research Council of the University of Patras.
Financial Disclosure
This work was funded by the Hellenic Institute for the study of sepsis.
Conflict of Interest
The authors declared no potential conflict of interest with respect to the research, authorship and/or publication of this article.
Informed Consent
All subjects provided written informed consent.
Author Contributions
Christos Davoulos: conceptualization, methodology, software, validation, formal analysis, investigation, writing - original draft, visualization, project administration, data curation. Evangelos J. Giamarellos-Bourboulis: conceptualization, methodology, resources, writing - review and editing, supervision, visualization, project administration, funding acquisition. Panagiotis Koufargyris: methodology, validation, resources, writing - review and editing. Charalambos Gogos: conceptualization, writing - review and editing, supervision. Dimitrios Velissaris: conceptualization, methodology, software, validation, formal analysis, writing - original draft, writing - review and editing, visualization, supervision, project administration, data curation.
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
APSIII: Acute Physiology Score III; AUC: area under the curve; CNS: central nervous system; COPD: chronic obstructive pulmonary disease; ELISA: enzyme-linked immunosorbent assay; ER: emergency room; ICU: intensive care unit; IFN: interferon; IL: interleukin; IL-33R: interleukin-33 receptor; LODS: Logical Organ Dysfunction System; LqSOFA: lactate quick SOFA; MAS: macrophage activation syndrome; MEWS: Modified Early Warning Score; NEWS: National Early Warning Score; PAMPs: pathogen-associated molecular patterns; qSOFA: quick SOFA; RAGE: receptor for advanced glycation end products; ROC: receiver operating characteristic; SIRS: systemic inflammatory response syndrome; SOFA: Sequential Organ Failure Assessment; SPSS: Statistical Package of the Social Sciences; ST2: suppression of tumorigenicity-2; TNF: tumor necrosis factor
| References | ▴Top |
- Rudd KE, Johnson SC, Agesa KM, Shackelford KA, Tsoi D, Kievlan DR, Colombara DV, et al. Global, regional, and national sepsis incidence and mortality, 1990-2017: analysis for the Global Burden of Disease Study. Lancet. 2020;395(10219):200-211.
doi pubmed - Fleischmann-Struzek C, Mellhammar L, Rose N, Cassini A, Rudd KE, Schlattmann P, Allegranzi B, et al. Incidence and mortality of hospital- and ICU-treated sepsis: results from an updated and expanded systematic review and meta-analysis. Intensive Care Med. 2020;46(8):1552-1562.
doi pubmed - Cortes-Puch I, Hartog CS. Opening the debate on the new sepsis definition change is not necessarily progress: revision of the sepsis definition should be based on new scientific insights. Am J Respir Crit Care Med. 2016;194(1):16-18.
doi pubmed - Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801-810.
doi pubmed - Xu H, Turnquist HR, Hoffman R, Billiar TR. Role of the IL-33-ST2 axis in sepsis. Mil Med Res. 2017;4:3.
doi pubmed - Babic ZM, Zunic FZ, Pantic JM, Radosavljevic GD, Jovanovic IP, Arsenijevic NN, Lukic ML. IL-33 receptor (ST2) deficiency downregulates myeloid precursors, inflammatory NK and dendritic cells in early phase of sepsis. J Biomed Sci. 2018;25(1):56.
doi pubmed - Royal College of Physicians of London. National Early Warning Score (NEWS): standardising the assessment of acute-illness severity in the NHS. Royal College of Physicians, 2012.
- Goulden R, Hoyle MC, Monis J, Railton D, Riley V, Martin P, Martina R, et al. qSOFA, SIRS and NEWS for predicting inhospital mortality and ICU admission in emergency admissions treated as sepsis. Emerg Med J. 2018;35(6):345-349.
doi pubmed - Usman OA, Usman AA, Ward MA. Comparison of SIRS, qSOFA, and NEWS for the early identification of sepsis in the Emergency Department. Am J Emerg Med. 2019;37(8):1490-1497.
doi pubmed - Sarkar R. A combined qSOFA-lactate model for sepsis-related mortality prediction: a small step towards an elusive answer? Lancet Glob Health. 2022;10(9):e1214-e1215.
doi pubmed - Giamarellos-Bourboulis EJ, Tsaganos T, Tsangaris I, Lada M, Routsi C, Sinapidis D, Koupetori M, et al. Validation of the new Sepsis-3 definitions: proposal for improvement in early risk identification. Clin Microbiol Infect. 2017;23(2):104-109.
doi pubmed - Evans L, Rhodes A, Alhazzani W, Antonelli M, Coopersmith CM, French C, Machado FR, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021;47(11):1181-1247.
doi pubmed - Gill A, Ackermann K, Hughes C, Lam V, Li L. Does lactate enhance the prognostic accuracy of the quick Sequential Organ Failure Assessment for adult patients with sepsis? A systematic review. BMJ Open. 2022;12(10):e060455.
doi pubmed - Guarino M, Perna B, Cesaro AE, Maritati M, Spampinato MD, Contini C, De Giorgio R. 2023 update on sepsis and septic shock in adult patients: management in the emergency department. J Clin Med. 2023;12(9).
doi pubmed - Karakike E, Giamarellos-Bourboulis EJ. Macrophage activation-like syndrome: a distinct entity leading to early death in sepsis. Front Immunol. 2019;10:55.
doi pubmed - Boomer JS, To K, Chang KC, Takasu O, Osborne DF, Walton AH, Bricker TL, et al. Immunosuppression in patients who die of sepsis and multiple organ failure. JAMA. 2011;306(23):2594-2605.
doi pubmed - Bomans K, Schenz J, Sztwiertnia I, Schaack D, Weigand MA, Uhle F. Sepsis induces a long-lasting state of trained immunity in bone marrow monocytes. Front Immunol. 2018;9:2685.
doi pubmed - Yao RQ, Ren C, Zheng LY, Xia ZF, Yao YM. Advances in immune monitoring approaches for sepsis-induced immunosuppression. Front Immunol. 2022;13:891024.
doi pubmed - Gogos CA, Drosou E, Bassaris HP, Skoutelis A. Pro- versus anti-inflammatory cytokine profile in patients with severe sepsis: a marker for prognosis and future therapeutic options. J Infect Dis. 2000;181(1):176-180.
doi pubmed - Ye Q, Du LZ, Shao WX, Shang SQ. Utility of cytokines to predict neonatal sepsis. Pediatr Res. 2017;81(4):616-621.
doi pubmed - McElvaney OJ, Hobbs BD, Qiao D, McElvaney OF, Moll M, McEvoy NL, Clarke J, et al. Corrigendum to 'A linear prognostic score based on the ratio of interleukin-6 to interleukin-10 predicts outcomes in COVID-19'. EBioMedicine. 2020;62:103116.
doi pubmed - Song J, Park DW, Moon S, Cho HJ, Park JH, Seok H, Choi WS. Diagnostic and prognostic value of interleukin-6, pentraxin 3, and procalcitonin levels among sepsis and septic shock patients: a prospective controlled study according to the Sepsis-3 definitions. BMC Infect Dis. 2019;19(1):968.
doi pubmed - Bhimraj A, Morgan RL, Shumaker AH, Baden LR, Cheng VC, Edwards KM, Gallagher JC, et al. Infectious diseases society of america guidelines on the treatment and management of patients with COVID-19 (September 2022). Clin Infect Dis. 2024;78(7):e250-e349.
doi pubmed - Leventogiannis K, Kyriazopoulou E, Antonakos N, Kotsaki A, Tsangaris I, Markopoulou D, Grondman I, et al. Toward personalized immunotherapy in sepsis: The PROVIDE randomized clinical trial. Cell Rep Med. 2022;3(11):100817.
doi pubmed - Nascimento DC, Melo PH, Pineros AR, Ferreira RG, Colon DF, Donate PB, Castanheira FV, et al. IL-33 contributes to sepsis-induced long-term immunosuppression by expanding the regulatory T cell population. Nat Commun. 2017;8:14919.
doi pubmed - Strickson S, et al. Oxidised IL-33 signals via RAGE/EGFR to drive a COPD-associated phenotype. In 03.02 - Airway cell biology and immunopathology, European Respiratory Society. 2022. p. 2482.
doi - England E, Rees DG, Scott IC, Carmen S, Chan DTY, Chaillan Huntington CE, Houslay KF, et al. Tozorakimab (MEDI3506): an anti-IL-33 antibody that inhibits IL-33 signalling via ST2 and RAGE/EGFR to reduce inflammation and epithelial dysfunction. Sci Rep. 2023;13(1):9825.
doi pubmed - Martinez-Gonzalez I, Roca O, Masclans JR, Moreno R, Salcedo MT, Baekelandt V, Cruz MJ, et al. Human mesenchymal stem cells overexpressing the IL-33 antagonist soluble IL-1 receptor-like-1 attenuate endotoxin-induced acute lung injury. Am J Respir Cell Mol Biol. 2013;49(4):552-562.
doi pubmed - Yin H, Li X, Yuan B, Zhang B, Hu S, Gu H, Jin X, et al. Heme oxygenase-1 ameliorates LPS-induced acute lung injury correlated with downregulation of interleukin-33. Int Immunopharmacol. 2011;11(12):2112-2117.
doi pubmed - Zhao J, Wei J, Mialki RK, Mallampalli DF, Chen BB, Coon T, Zou C, et al. F-box protein FBXL19-mediated ubiquitination and degradation of the receptor for IL-33 limits pulmonary inflammation. Nat Immunol. 2012;13(7):651-658.
doi pubmed - Wang H, Hosakote YM, Boor PJ, Yang J, Zhang Y, Yu X, Gonzales C, et al. The alarmin IL-33 exacerbates pulmonary inflammation and immune dysfunction in SARS-CoV-2 infection. iScience. 2024;27(6):110117.
doi pubmed - Parenica J, Malaska J, Jarkovsky J, Lipkova J, Dastych M, Helanova K, Litzman J, et al. Soluble ST2 levels in patients with cardiogenic and septic shock are not predictors of mortality. Exp Clin Cardiol. 2012;17(4):205-209.
pubmed - Hur M, Kim H, Kim HJ, Yang HS, Magrini L, Marino R, Cardelli P, et al. Soluble ST2 has a prognostic role in patients with suspected sepsis. Ann Lab Med. 2015;35(6):570-577.
doi pubmed - Hoogerwerf JJ, Tanck MW, van Zoelen MA, Wittebole X, Laterre PF, van der Poll T. Soluble ST2 plasma concentrations predict mortality in severe sepsis. Intensive Care Med. 2010;36(4):630-637.
doi pubmed - Hincapie C, van Wijk R, Postma D, Bouma H, ter Maaten J. Evaluating and comparing prognostic scores in patients with respiratory tract infections at the emergency department. In A23. Investigating heterogeneity in sepsis and pneumonia: trials, cohorts, and patient-oriented research, American Thoracic Society, 2024. p. A1113.
doi - Fan S, Ma J. The value of five scoring systems in predicting the prognosis of patients with sepsis-associated acute respiratory failure. Sci Rep. 2024;14(1):4760.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.