| Journal of Clinical Medicine Research, ISSN 1918-3003 print, 1918-3011 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, J Clin Med Res and Elmer Press Inc |
| Journal website https://jocmr.elmerjournals.com |
Original Article
Volume 17, Number 10, October 2025, pages 565-573
Effectiveness of Short-Acting Oral Antihypertensives in Asymptomatic Markedly Elevated Blood Pressure: An Inverse Probability Treatment Weighted Study
Supark Chotichaipiboona , Thanin Lokeskraweea, e
, Natthaphon Pruksathorna
, Jarupa Yaowalaornga
, Suppachai Lawanaskolb
, Jayanton Patumanondc, Wanwisa Bumrungpagdeed, Suwapim Chanlaord, Chawalit Lakdeed
aDepartment of Emergency Medicine, Lampang Hospital, Lampang, Thailand
bChaiprakarn Hospital, Chiang Mai, Thailand
cClinical Epidemiology and Clinical Statistics Unit, Faculty of Medicine, Naresuan University, Phitsanulok, Thailand
dDepartment of Radiology, Buddhachinaraj Phitsanulok Hospital, Phitsanulok, Thailand
eCorresponding Author: Thanin Lokeskrawee, Department of Emergency Medicine, Lampang Hospital, Lampang, 52000 Thailand
Manuscript submitted August 11, 2025, accepted October 25, 2025, published online October 29, 2025
Short title: Short-Acting Oral Antihypertensives in AMEBP
doi: https://doi.org/10.14740/jocmr6353
| Abstract | ▴Top |
Background: Although guidelines recommend gradual blood pressure (BP) reduction in asymptomatic markedly elevated BP (AMEBP), short-acting oral antihypertensives are often used despite limited evidence - driven by healthcare providers’ concerns or institutional policies - thereby increasing system burden. This study aimed to identify practical regimens enabling safe, timely discharge and continuity of care.
Methods: This retrospective cohort included patients with AMEBP (systolic BP > 180 mm Hg and/or diastolic BP > 110 mm Hg), who presented to the emergency department (ED) of Lampang Hospital between January and December 2023. Oral regimens included captopril, hydralazine, metoprolol (25 mg each), or combinations. The outcome was mean arterial pressure (MAP) reduction within 60 min, classified as no reduction (< 10%), appropriate reduction (10-15%), or over-reduction (> 15%). Inverse probability of treatment weighting (IPTW) adjusted for regimen selection, and multinomial odds ratios (mORs) with 95% confidence intervals (CIs) were reported.
Results: Among 158 patients (mean age 60 years; 67.1% female), baseline MAP was 142.4 ± 16.2 mm Hg. Captopril and hydralazine monotherapy were most likely to achieve appropriate reduction (captopril: mOR: 2.91; 95% CI: 0.96, 8.76; P = 0.058; hydralazine: mOR: 2.76; 95% CI: 0.84, 9.11; P = 0.096). Metoprolol was associated with inappropriate response, while captopril plus hydralazine had highest odds of over-reduction (mOR: 3.04; 95% CI: 1.02, 9.00; P = 0.045).
Conclusions: Although urgent BP reduction is not routinely recommended in the ED, oral captopril appears to be a reasonable first-line option when clinically necessary, while hydralazine may be a suitable alternative. Combination of these two drugs should be used with caution due to the risk of excessive MAP reduction.
Keywords: Hypertension; Antihypertensive agents; Short-acting; Treatment outcome; Arterial pressure; Propensity score
| Introduction | ▴Top |
High blood pressure (BP) poses a significant health burden in upper-middle-income countries, contributing to cardiovascular mortality of up to 143 per 100,000 population, more than double that observed in high-income countries (64 per 100,000) [1]. Notably, rising systolic blood pressure (SBP) is associated with a steeper increase in the hazard of stroke and cardiovascular disease in Asian populations compared with Caucasians [2], underscoring the disproportionate burden of hypertension in this region.
In Thailand, the northern region reports the highest prevalence of hypertension (33%), followed by the southern (28%), central and Bangkok regions (both 23%), and the northeastern region (21%) [3-6]. Extensive evidence has consistently supported a causal relationship between salt intake and BP [7-11]. In the northern region, individuals consume an average of 3,044.1 mg of sodium [4, 5] and 10.8 g of salt [6], exceeding the World Health Organization (WHO) recommended limits of less than 2,000 mg of sodium and 5 g of salt per day, respectively [4, 6]. Moreover, uncontrolled BP is often attributed to multifactorial causes [10]. At Lampang Hospital, approximately 500 cases of asymptomatic markedly elevated blood pressure (AMEBP) - formerly referred to as hypertensive urgency [12-15] - are seen annually in the emergency department (ED), with 75% referred from outpatient departments (OPDs).
Despite recommendations for gradual BP reduction over several days to weeks [12-15], ED-based lowering is frequently undertaken due to institutional policies and provider concerns. However, prior Thai studies have several limitations: 1) Most focused solely on absolute differences in SBP, diastolic BP (DBP), or mean arterial pressure (MAP) [16, 17] without defining an appropriate percentage range of reduction; 2) Some applied overly aggressive strategies, reducing 20-30% of resting MAP [18]; 3) Others initiated antihypertensive therapy in mixed populations, of which hypertensive urgency accounted for only about 9% [19]; 4) Most employed only basic regression with confounder adjustment; and 5) None accounted for the multinomial nature of outcomes - no reduction, appropriate reduction, and over-reduction - leading to statistically inappropriate analyses.
In light of these limitations, there remains a gap between evidence-based recommendations and real-world clinical practice. Additionally, about half of AMEBP patients cannot return to a specialist clinic on the same day; follow-up is often delayed by 1 to 2 weeks, and some patients travel up to 120 km to the hospital. These challenges highlight the need to identify short-acting oral antihypertensive regimens that achieve appropriate BP reduction while maintaining safety in the ED.
| Materials and Methods | ▴Top |
Study design
This observational cohort study was conducted in the ED of Lampang Hospital, a tertiary care center that receives approximately 75,000 ED visits annually, of which around 500 involve cases of AMEBP. Between January and December 2023, patients presenting with AMEBP, either referred from the OPDs or self-presenting to the ED, underwent initial evaluation including vital signs, followed by secondary assessment comprising history taking and a focused physical examination for hypertension-mediated organ damage (HMOD). All patients received a 12-lead electrocardiography (ECG), and in selected cases, estimated glomerular filtration rate (eGFR) was measured or recent outpatient values were reviewed.
Lampang Hospital ED protocol
Asymptomatic patients incidentally found to have an SBP > 180 mm Hg and/or a DBP > 110 mm Hg [12-15] were managed in accordance with a standardized ED protocol. At triage, BP was measured by a triage nurse using an automated oscillometric sphygmomanometer - which automatically calculated the MAP - while the patient was seated after a 5-min rest. The cuff size was selected according to the American Heart Association (AHA) guidelines [20]. If the BP remained > 180/110 mm Hg, the patient was transferred to the ED observation unit (EDOU) - a quiet and separate area intended to facilitate rest - for an additional 15 min of bed rest. The BP remeasured after this period was defined as the “resting BP.”
To ensure safety and avoid over-reduction, we prespecified an ED target of a 10-15% decrease in MAP from the resting BP [15]. Our stepwise rationale was as follows: 1) The recommended early reduction for hypertensive emergency is 20-25% over several hours, which is not appropriate for AMEBP; 2) Our department’s initial consensus considered a 15-20% range; 3) We considered a 20% reduction too close to emergency thresholds, posing a potential risk of over-reduction in AMEBP; 4) We consequently adopted a 10-15% target, consistent with contemporary guidance summarized in the 2024 European Society of Cardiology (ESC) hypertension guideline [15]; and 5) Operationally, after a period of rest, patients whose BP spontaneously fell within the 10-15% target were returned to the OPD without pharmacologic treatment, whereas persistent elevation prompted an AMEBP diagnosis and administration of short-acting oral antihypertensives in the EDOU.
The selection of antihypertensive agents was based on patient age, renal function, and pulse rate. First, patients were stratified by age (< 80 vs. ≥ 80 years) and renal function (eGFR > 60 vs. ≤ 60 mL/min/1.73 m2).
For patients under 80 years of age with an eGFR > 60 mL/min/1.73 m2, pulse rate determined the choice of oral medication: 1) If pulse ≥ 80 beats per minute (bpm), four regimens were considered: captopril 25 mg, hydralazine 25 mg, metoprolol 25 mg, or their combinations; 2) If pulse < 80 bpm, metoprolol was contraindicated, leaving three options: captopril, hydralazine, or their combination.
For patients aged 80 years or older, or with eGFR ≤ 60 mL/min/1.73 m2, captopril was avoided due to safety concerns: 1) If pulse ≥ 80 bpm, available options included hydralazine 25 mg, metoprolol 25 mg, or their combination; 2) If pulse < 80 bpm, only hydralazine 25 mg was used.
It is noted that this protocol was applied flexibly under the structured approach; the final selection of medication also considered resting BPs, patients’ overall conditions, and physicians’ preferences.
Participant and data collection
Participants
Asymptomatic adults aged 18 years or older with SBP > 180 mm Hg and/or DBP > 110 mm Hg were eligible for inclusion. Exclusion criteria comprised missing structured BP records, management not following the Lampang Hospital ED protocol, presence of HMOD after focused assessment, acute trauma, severe pain contributing to transient BP elevation, recent alcohol or illicit drug use, psychiatric conditions, and pregnancy.
Endpoints
BP was recorded at 30 and 60 min after the administration of the antihypertensive regimens. The primary endpoint was the percentage reduction in MAP at 60 min, calculated as: (resting MAP - MAP at 60 min)/resting MAP × 100.
Outcomes were categorized into three groups: minimal-to-no reduction (< 10%), appropriate reduction (10-15%), and over-reduction (> 15%), using the minimal-to-no reduction group as the reference.
Study size estimation
The required sample size was estimated through pairwise comparisons of the proportions of appropriate MAP reduction across six regimens, using data from a pilot study involving 30 patients. The calculated sample sizes varied widely and were impractical for certain regimen pairs, particularly for the comparison between captopril + metoprolol and hydralazine + metoprolol, which required up to 745 vs. 1,211 participants. Therefore, the comparison between captopril alone (58%) and hydralazine alone (25%) was adopted as the reference for sample size estimation. Using a one-sided test with an alpha error of 5%, power of 80%, and a 1:1 allocation ratio, the required sample size was determined to be 33 patients per group. This number was sufficient to accommodate other relevant pairwise comparisons, including captopril alone vs. metoprolol alone, captopril alone vs. captopril + metoprolol, and captopril alone vs. hydralazine + metoprolol.
Statistical analysis
Baseline characteristics were compared across the six antihypertensive regimens. Categorical variables were analyzed using the exact probability test, and continuous variables were assessed using one-way analysis of variance (ANOVA).
Treatment selection varied according to physician discretion and patient-specific indications or contraindications, resulting in unequal group sizes. To mitigate selection bias, inverse probability of treatment weighting (IPTW) incorporating covariates (sex, age, pulse rate, and eGFR) was applied. Stabilized weights were generated to improve comparability among treatment groups by balancing baseline characteristics.
Outcomes were classified into three levels: minimal-to-no reduction (reference), appropriate reduction, and over-reduction. Multinomial logistic regression was used to estimate the effectiveness of all regimens simultaneously within a single analytical model. Results were presented as multinomial odds ratios (mORs) with corresponding 95% confidence intervals (CIs) and P values.
All statistical analyses were performed using Stata, version 18 (StataCorp, College Station, TX, USA).
The study protocol was registered with the Thai Clinical Trials Registry (TCTR) (TCTR20250810001) and approved by the Institutional Review Board of Lampang Hospital (CERT No. 159/67; approved December 27, 2024, valid until December 26, 2025). Informed consent was waived due to the observational design, and all patient data were anonymized before analysis. The study was conducted in accordance with institutional ethical standards and the principles of the Declaration of Helsinki and its subsequent amendments.
| Results | ▴Top |
Between January and December 2023, after exclusion, a total of 158 eligible patients were analyzed. Most were female (67.1%) with a mean age of 60 years. Six antihypertensive regimens were included, with varying sample sizes due to being observational in nature. Patients in the hydralazine monotherapy group were older and had the lowest eGFR. Higher pulse rates were observed in those receiving metoprolol alone and hydralazine plus metoprolol. The captopril plus metoprolol group had the highest values for both initial and resting DBP (Fig. 1, Table 1).
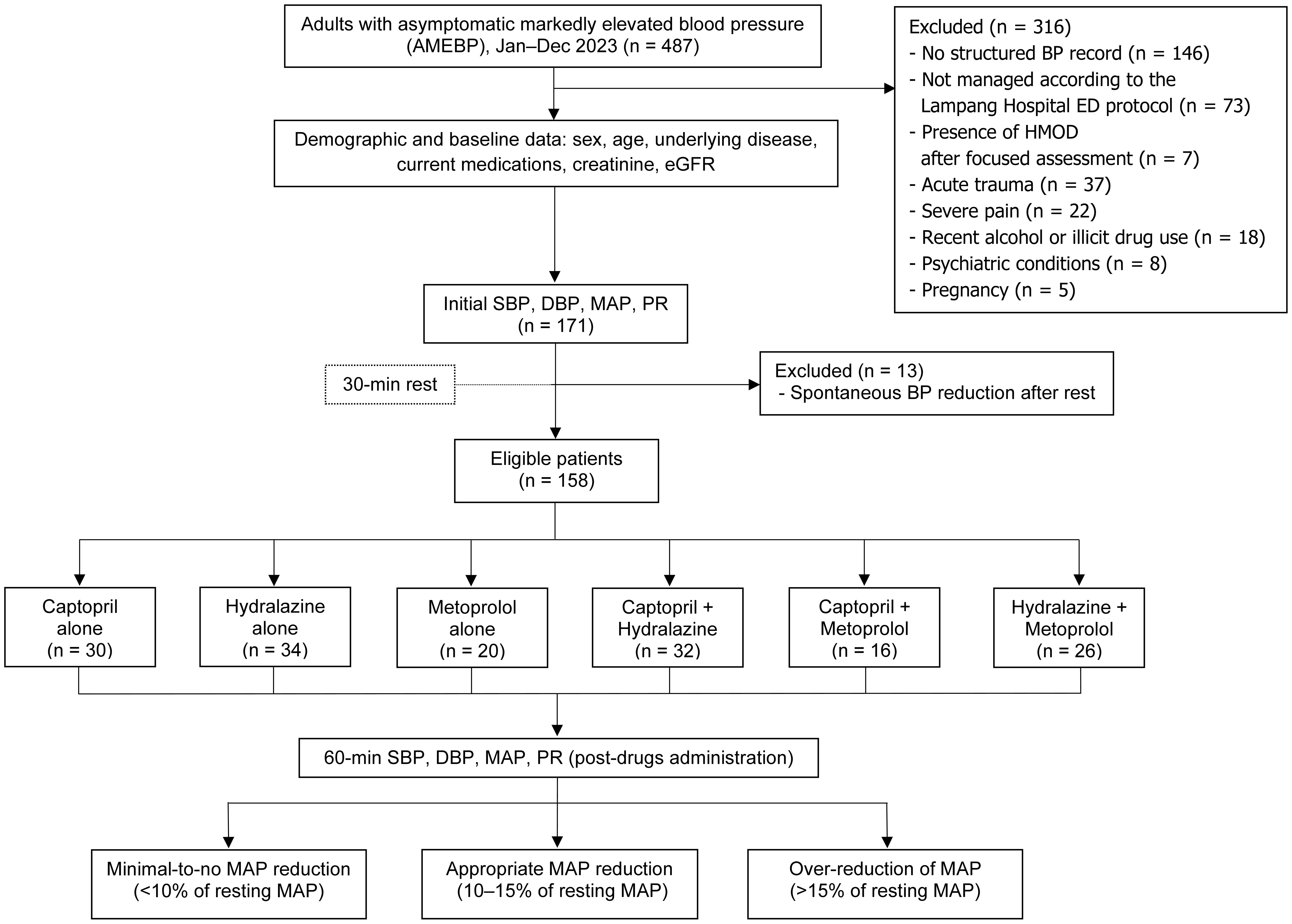 Click for large image | Figure 1. Study flow diagram. BP: blood pressure; ED: emergency department; HMOD: hypertension-mediated organ damage; eGFR: estimated glomerular filtration rate; SBP: systolic blood pressure; DBP: diastolic blood pressure; MAP: mean arterial pressure; PR: pulse rate. |
 Click to view | Table 1. Baseline Characteristics of Patients Across Antihypertensive Regimens |
At 60 min after antihypertensive administration, the captopril plus hydralazine regimen yielded the greatest crude percentage reduction in MAP, with a median of -13.64% (interquartile range (IQR): -20.88 to -10.74). In contrast, metoprolol monotherapy showed minimal change, with a median of -2.79% (IQR: -13.03 to 2.04) (Table 2).
 Click to view | Table 2. Crude Percent Reduction in Mean Arterial Pressure (MAP) Across Antihypertensive Regimens |
After multinomial logistic regression using the minimal-to-no reduction group as the reference and adjusting for confounders (IPTW applied as previously described), captopril monotherapy showed the highest likelihood of achieving appropriate MAP reduction (mOR: 2.91; 95% CI: 0.96, 8.76; P = 0.058), followed by hydralazine monotherapy (mOR: 2.76; 95% CI: 0.84, 9.11; P = 0.096). The combination of captopril and hydralazine yielded the highest odds for MAP over-reduction (mOR: 3.04; 95% CI: 1.02, 9.00; P = 0.045). In contrast, metoprolol monotherapy demonstrated significantly lower odds of achieving appropriate MAP reduction (mOR: 0.09; 95% CI: 0.02, 0.42; P = 0.002) and was also less likely to result in MAP over-reduction (mOR: 0.20; 95% CI: 0.06, 0.68; P = 0.010), indicating an overall negligible effect on MAP (Table 3).
 Click to view | Table 3. Multinomial Odds Ratios for Appropriate and Over-Reduction Across Antihypertensive Regimens (IPTW-Adjusted), Using Minimal-to-No Reduction as Baseline |
No adverse events or complications were observed across any antihypertensive regimens; however, the relatively small sample size limits definitive conclusions regarding safety (Table 4).
 Click to view | Table 4. Post-Treatment Adverse Events by Antihypertensive Regimens |
| Discussion | ▴Top |
A multicenter study in the United States reported that lowering BP in the ED did not improve clinical outcomes [21], consistent with the recently published 2025 AHA/American College of Cardiology (ACC) guideline [22], which redefines AMEBP as “severe hypertension without evidence of acute target organ damage” and reiterates that BP reduction in the ED is not routinely recommended. Given that northern Thailand has the highest prevalence of severe hypertension nationwide [3-6], both our study and prior regional investigations [16, 18] included patients with AMEBP and implemented BP reduction. Although we recognize that urgent BP lowering is generally unnecessary, our practice was nevertheless mandated by institutional directives and providers’ concerns. To ensure patient safety under these conditions, we targeted a modest 10-15% reduction in resting MAP, measured 1 h after antihypertensive administration.
In real-world practice, approximately 75% of AMEBP cases are referred from OPDs, and nearly half cannot be seen by a specialist on the same day; follow-up is often delayed by 1 to 2 weeks. Our study therefore aimed for a modest MAP reduction that would allow patients to safely return to OPD care in a timely manner. Because all participants were asymptomatic, a comprehensive HMOD evaluation was not pursued. Instead, we performed a focused assessment comprising a primary survey, history taking, physical examination, a 12-lead ECG, and eGFR to compare renal function with prior values. A full HMOD workup, as recommended by guidelines [12-15], is time-consuming, costly, and provides limited cost-effectiveness in this context; therefore, extensive investigations were deemed unnecessary in the ED setting.
Captopril, a short-acting angiotensin-converting enzyme (ACE) inhibitor, lowers BP by inhibiting the conversion of angiotensin I to angiotensin II, resulting in vasodilation and decreased aldosterone secretion. It is well absorbed orally, reaching peak plasma concentrations within 1 h [23]. Although captopril can be used cautiously in patients with chronic kidney disease (CKD) [24], the Lampang Hospital ED protocol prioritizes safety; thus, an eGFR < 60 mL/min/1.73 m2 was considered a contraindication in this study. Captopril ranked among the top two agents for achieving appropriate MAP reduction, with borderline statistical significance - an effect suggesting a possible trend that warrants confirmation in larger studies. This result aligns with prior research supporting the use of 25 mg oral captopril for AMEBP management [25, 26].
Hydralazine, a direct arteriolar vasodilator, represents another viable option for BP control. Its effects typically begin within 20 to 30 min after oral administration, and it is safe for use in patients with CKD, including those on maintenance dialysis [27, 28]. In this study, hydralazine demonstrated a comparable trend toward appropriate MAP reduction, although the effect did not reach statistical significance. When captopril is contraindicated, 25 mg oral hydralazine may be considered a suitable alternative.
The combination of captopril and hydralazine was associated with a statistically significant over-reduction in MAP, raising safety concerns regarding potential complications such as hypotension, transient ischemic attack, stroke, and myocardial infarction [29, 30]. This finding underscores the need for caution and highlights the importance of further confirmatory studies to evaluate the safety profile of combination therapy.
Metoprolol monotherapy exhibited significantly reduced likelihood of achieving appropriate MAP reduction and was less likely to cause MAP over-reduction, indicating an overall negligible effect on BP. This may be attributed to the low dose used in this study (25 mg orally), which could not be escalated due to safety concerns, particularly the risk of bradycardia. These findings align with current guidelines, which do not recommend beta-blockers as a first-line option for the outpatient management of severe hypertension. However, metoprolol may still be considered as an adjunct to other antihypertensive agents or in select clinical situations [12-15].
Traditional propensity score methods such as matching or stratification could not be applied in this study because of absolute treatment indications and contraindications defined by the Lampang Hospital ED protocol. Instead, we applied IPTW [31] with confounder adjustment - a propensity score-based approach - to upweight patients who received less likely treatments and downweight those who received more likely ones. We subsequently employed multinomial logistic regression, which is well-suited for the three categorical outcomes: minimal-to-no reduction (baseline), appropriate reduction, and over-reduction. Unlike binary logistic regression, which requires collapsing outcomes and analyzing them in pairs, multinomial logistic regression models all outcome categories simultaneously within a single framework. This approach utilizes the entire dataset to improve statistical efficiency and power by preserving information across all categories, ensuring consistent variance estimation, and minimizing the inflated type I error that can result from multiple pairwise comparisons [32-34].
A key limitation of this study is its relatively small sample size. Although the initial cohort included nearly three times the number of eligible patients, many were excluded due to missing structured BP records or deviation from the institutional protocol. Moreover, being a single-center retrospective study may limit the generalizability of the findings. The analysis focused solely on short-term outcomes, specifically MAP reduction, without subsequent assessment of revisits or readmissions. Potential unmeasured confounders - such as comorbidities, baseline antihypertensive therapy, medication adherence, and lifestyle factors - could not be fully controlled. Future multicenter prospective studies with extended follow-up are needed to confirm these results and evaluate long-term safety profiles.
The study provides practical insight into real-world ED management of AMEBP. Preferably, a coordinated approach involving the OPD, ED, relevant specialists, and hospital leadership should be implemented to reduce unnecessary ED referrals for BP control alone. Official communication, gradual organizational learning, cultural adaptation, and continuous knowledge sharing remain essential for achieving sustainable improvement in hypertension management.
Conclusions
Current guidelines discourage urgent BP reduction in the ED; however, institutional protocols or clinical necessity may occasionally require acute pharmacologic treatment. In such cases, oral captopril 25 mg appears to be a reasonable first-line option, while oral hydralazine 25 mg may serve as a suitable alternative. Caution is warranted when combining these two agents due to the risk of excessive MAP reduction, though confirmatory prospective studies are needed to validate these findings.
Acknowledgments
This study was supported by the Lampang Medical Education Center. The authors would like to thank the Emergency Medicine residents, staff, and registered nurses at the Department of Emergency Medicine, Lampang Hospital.
Financial Disclosure
This study was supported by the Lampang Medical Education Center.
Conflict of Interest
The authors reported no conflicts of interest in the article.
Informed Consent
Informed consent was waived due to the observational nature of the study.
Author Contributions
Conceptualization: Supark Chotichaipiboon, Thanin Lokeskrawee, Suppachai Lawanaskol, Jayanton Patumanond. Data curation: Supark Chotichaipiboon. Formal analysis: Supark Chotichaipiboon, Natthaphon Pruksathorn, Jarupa Yaowalaorng, Suwapim Chanlaor, Wanwisa Bumrungpagdee, Chawalit Lakdee, Thanin Lokeskrawee, Suppachai Lawanaskol, Jayanton Patumanond. Methodology: Thanin Lokeskrawee, Suppachai Lawanaskol, Jayanton Patumanond. Supervision: Thanin Lokeskrawee, Suppachai Lawanaskol, Jayanton Patumanond. Writing-original draft: Supark Chotichaipiboon, Thanin Lokeskrawee, Suppachai Lawanaskol, Jayanton Patumanond.
Data Availability
Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.
| References | ▴Top |
- Schutte AE, Srinivasapura Venkateshmurthy N, Mohan S, Prabhakaran D. Hypertension in low- and middle-income countries. Circ Res. 2021;128(7):808-826.
doi pubmed - Perkovic V, Huxley R, Wu Y, Prabhakaran D, MacMahon S. The burden of blood pressure-related disease: a neglected priority for global health. Hypertension. 2007;50(6):991-997.
doi pubmed - Aekplakorn W, Sangthong R, Kessomboon P, Putwatana P, Inthawong R, Taneepanichskul S, Sritara P, et al. Changes in prevalence, awareness, treatment and control of hypertension in Thai population, 2004-2009: Thai National Health Examination Survey III-IV. J Hypertens. 2012;30(9):1734-1742.
doi pubmed - Satheannoppakao W, Kasemsup R, Inthawong R, Chariyalertsak S, Sangthong R, Taneepanichskul S, Putwatana P, et al. Sodium intake and socio-demographic determinants of the non-compliance with daily sodium intake recommendations: Thai NHES IV. J Med Assoc Thai. 2013;96(Suppl 5):S161-170.
pubmed - Rusmevichientong P, Morales C, Castorena G, Sapbamrer R, Seesen M, Siviroj P. Dietary salt-related determinants of hypertension in rural northern Thailand. Int J Environ Res Public Health. 2021;18(2):377.
doi pubmed - World Health Organization Country Office for Thailand. Hypertension care in Thailand: best practices and challenges, 2019 [Internet]. Nonthaburi: Ministry of Public Health; 2019 [cited Jun 5, 2025]. Available from: https://iris.who.int/handle/10665/330488.
- He FJ, MacGregor GA. Reducing population salt intake worldwide: from evidence to implementation. Prog Cardiovasc Dis. 2010;52(5):363-382.
doi pubmed - Guideline: sodium intake for adults and children. Geneva, 2012.
pubmed - Thawornchaisit P, de Looze F, Reid CM, Seubsman SA, Sleigh A, Thai Cohort Study T. Health-risk factors and the prevalence of hypertension: cross-sectional findings from a national cohort of 87,143 Thai Open University students. Glob J Health Sci. 2013;5(4):126-141.
doi pubmed - Rust P, Ekmekcioglu C. Impact of salt intake on the pathogenesis and treatment of hypertension. Adv Exp Med Biol. 2017;956:61-84.
doi pubmed - Grillo A, Salvi L, Coruzzi P, Salvi P, Parati G. Sodium intake and hypertension. Nutrients. 2019;11(9):1970.
doi pubmed - Whelton PK, Carey RM, Aronow WS, Casey DE, Jr., Collins KJ, Dennison Himmelfarb C, DePalma SM, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Hypertension. 2018;71(6):1269-1324.
doi pubmed - Mancia G, Kreutz R, Brunstrom M, Burnier M, Grassi G, Januszewicz A, Muiesan ML, et al. 2023 ESH Guidelines for the management of arterial hypertension The Task Force for the management of arterial hypertension of the European Society of Hypertension: Endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA). J Hypertens. 2023;41(12):1874-2071.
doi pubmed - Bress AP, Anderson TS, Flack JM, Ghazi L, Hall ME, Laffer CL, Still CH, et al. The Management of Elevated Blood Pressure in the Acute Care Setting: A Scientific Statement From the American Heart Association. Hypertension. 2024;81(8):e94-e106.
doi pubmed - McEvoy JW, McCarthy CP, Bruno RM, Brouwers S, Canavan MD, Ceconi C, Christodorescu RM, et al. 2024 ESC Guidelines for the management of elevated blood pressure and hypertension. Eur Heart J. 2024;45(38):3912-4018.
doi pubmed - Sruamsiri K, Chenthanakij B, Wittayachamnankul B. Management of patients with severe hypertension in emergency department, Maharaj Nakorn Chiang Mai hospital. J Med Assoc Thai. 2014;97(9):917-922.
pubmed - Jirdsermanun R, Durongbhandhu T. A prospective observational study comparing oral captopril, hydralazine, and amlodipine in patients with hypertensive urgency at the emergency room at Bangplee Hospital. J Emerg Med Serv Thai. 2024;4(2):147-156.
- Promyuang P. Comparing the efficacy of antihypertensive drug between captopril (25 mg) and hydralazine (25 mg) in patients with hypertensive urgency in emergency department, Chiangrai Prachanukroh Hospital. Chiangrai Med J. 2022;14(1):17-30.
- Kotruchin P, Mitsungnern T, Ruangsaisong R, Imoun S, Pongchaiyakul C. Hypertensive urgency treatment and outcomes in a northeast Thai population: the results from the hypertension registry program. High Blood Press Cardiovasc Prev. 2018;25(3):309-315.
doi pubmed - American Heart Association. Selecting a cuff size [Internet]. Dallas (TX): AHA; 2025 [cited Oct 15, 2025]. Available from: https://targetbp.org/patient-measured-bp/implementing/smbp-selecting-the-right-cuff-size/.
- Chaudhry F, Small E, Korzeniewski SJ, Benyas D, Ross L, Hill AB, Vahia A, et al. Emergency department blood pressure treatment and outcomes in adults presenting with severe hypertension. West J Emerg Med. 2024;25(5):680-689.
doi pubmed - Writing Committee M, Jones DW, Ferdinand KC, Taler SJ, Johnson HM, Shimbo D, Abdalla M, et al. 2025 AHA/ACC/AANP/AAPA/ABC/ACCP/ACPM/AGS/AMA/ASPC/NMA/PCNA/SGIM guideline for the prevention, detection, evaluation and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Hypertension. 2025;82(10):e212-e316.
doi pubmed - Marte F, Sankar P, Patel P, Cassagnol M. Captopril. In: StatPearls. Treasure Island (FL) ineligible companies. 2025.
pubmed - Kidney Disease: Improving Global Outcomes Diabetes Work G. KDIGO 2020 clinical practice guideline for diabetes management in chronic kidney disease. Kidney Int. 2020;98(4S):S1-S115.
doi pubmed - Obied AHH, Ahmed AAE. Evaluation of the clinical outcome of captopril use for hypertensive urgency in Khartoum State's emergency centres. Afr J Emerg Med. 2021;11(1):202-206.
doi pubmed - Vidt DG. Emergency room management of hypertensive urgencies and emergencies. J Clin Hypertens (Greenwich). 2001;3(3):158-164.
doi pubmed - Herman LL, Bruss ZS, Tivakaran VS. Hydralazine. In: StatPearls. Treasure Island (FL) ineligible companies. 2025.
pubmed - Mavrakanas TA, Soomro QH, Charytan DM. Hydralazine-isosorbide dinitrate use in patients with end-stage kidney disease on dialysis. Kidney Int Rep. 2022;7(6):1332-1340.
doi pubmed - Kessler CS, Joudeh Y. Evaluation and treatment of severe asymptomatic hypertension. Am Fam Physician. 2010;81(4):470-476.
pubmed - Adebayo O, Rogers RL. Hypertensive emergencies in the emergency department. Emerg Med Clin North Am. 2015;33(3):539-551.
doi pubmed - Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. 2015;34(28):3661-3679.
doi pubmed - Becg CB, Gray R. Calculation of polychotomous logistic regression parameters using individualized regressions. Biometrika. 1984;71(1):11-18.
- Hosmer DW, Lemeshow S, Sturdivant RX. Applied logistic regression. 3rd ed. New Jersey: Wiley; 2013.
- Agresti A. Categorical data analysis. Third edition. Hoboken, New Jersey: Wiley-Interscience; 2013.
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Journal of Clinical Medicine Research is published by Elmer Press Inc.