Organ Damage and Its Associated Factors in Systemic Lupus Erythematosus Patients: A Retrospective Cohort Study
DOI:
https://doi.org/10.14740/jocmr6129Keywords:
SLE, Organ damage, Risk factors, Systemic Damage Index, SLEDAI-2K, Hydroxychloroquine, CorticosteroidsAbstract
Background: Systemic lupus erythematosus (SLE) can affect a plethora of organ systems and cause organ damage due to the disease process and medication toxicity, notably corticosteroids. Patients with SLE often suffer irreversible organ damage. Older age, glucocorticoid use, longer disease duration, and disease activity all represent risk factors for organ damage. This study aims to assess the incidence and predictors of organ damage among Saudi Arabian SLE patients.
Methods: This study is a single-center, retrospective cohort observational study conducted at the adult Rheumatology Outpatient Clinic in King Fahad Medical City, Riyadh, Saudi Arabia. It included all patients aged 16 years and older who met at least four of the American College of Rheumatology Classification criteria for SLE or had a renal biopsy consistent with lupus nephritis and had regular follow-ups at our hospital, with the last visit occurring within 2 years.
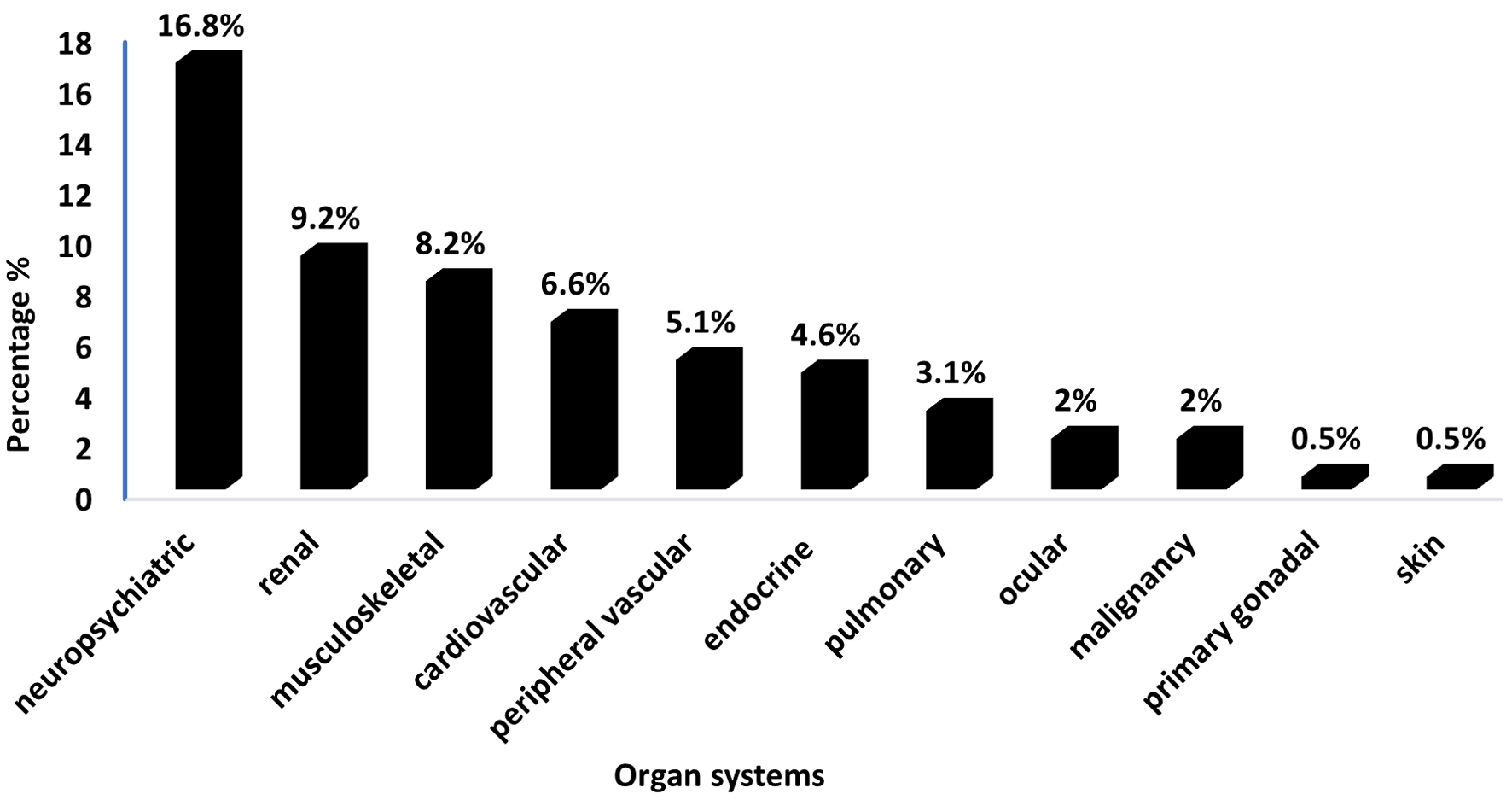
Results: The study included 196 patients with SLE, predominantly female (92.9%) with a mean age of 36.2 years and an average disease duration of 8.88 years. Among the patients, 38.8% had a positive Systemic Damage Index (SDI) score. Hydroxychloroquine was used by 93.4% of the patients, and 46.9% had a Systemic Lupus Erythematosus Disease Activity Index 2000 (SLEDAI-2K) score of 3 or higher. The neuropsychiatric system was most affected, with 16.8% of patients having positive SDI scores in this domain, followed by the renal system at 9.2%. Patients with positive SDI scores were significantly older, had longer disease duration, and had higher prevalence of diabetes mellitus and hypertension.
Conclusion: To address organ damage in SLE patients, integrating adjunctive therapies like antihypertensives and antidiabetic agents into management plans is essential. Future research should adopt prospective cohort designs to evaluate the dynamic interactions between comorbidities and organ damage over time. Additionally, studies should assess the effectiveness of combined treatment strategies and develop targeted approaches for high-risk groups to enhance outcomes and quality of life.
Published
Issue
Section
License
Copyright (c) 2024 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.








