Strategies in Management of Pulmonary Embolism With Acute Ischemic Stroke: A Systematic Review
DOI:
https://doi.org/10.14740/jocmr6153Keywords:
Pulmonary embolism, Ischemic stroke, Case reports, Anticoagulation, Thrombolysis, Mechanical thrombectomy, Catheter-directed thrombolysis, Patent foramen ovaleAbstract
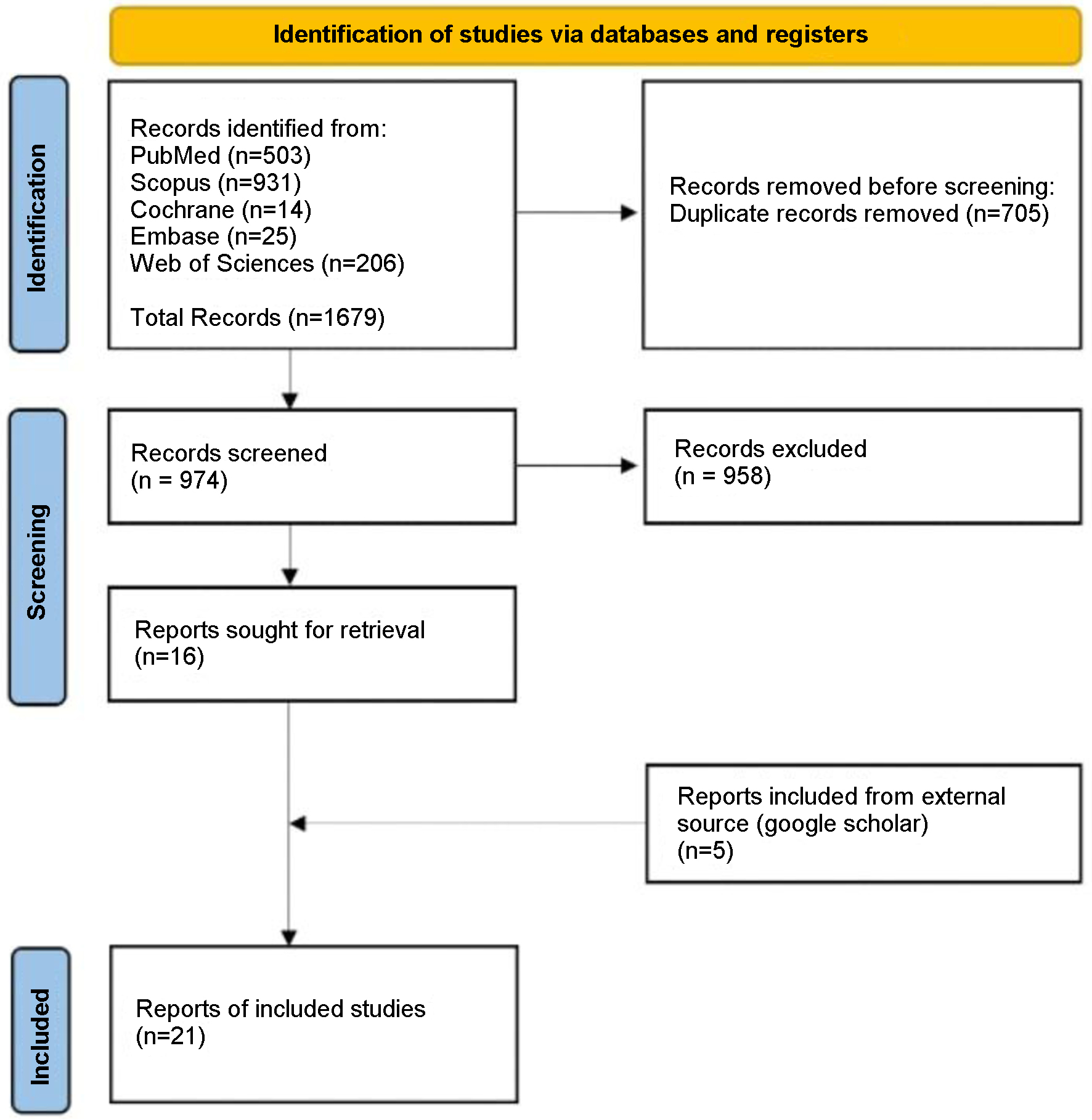
Pulmonary embolism (PE) and acute ischemic stroke (AIS) are serious conditions with high morbidity and mortality. In the USA, PE causes around 100,000 deaths annually, with higher incidence in males. AIS following PE occurs in 1-10% of cases and is a leading cause of death within 2 - 4 weeks post-stroke. Managing concurrent PE and AIS is complex due to the need for anticoagulation, which is contraindicated after thrombolysis for AIS. This review evaluates the impact of various PE treatments - anticoagulation, thrombolysis, and embolectomy - on mortality in patients with both conditions. Following PRISMA 2020 guidelines, a systematic review was conducted across six databases from January 2010 to December 2023. The primary outcome measured was mortality, comparing treated vs. untreated patients for PE. Secondary outcomes included marked symptom improvement, slight improvement or deterioration of symptoms, and the complications. Data were analyzed descriptively, summarizing patient demographics, clinical characteristics, and treatment outcomes. Treatment modalities, such as anticoagulation, thrombolysis, catheter-directed thrombectomy, surgical thrombectomy, and conservative management, were evaluated based on their impact on symptom improvement, survival, and mortality. Initial querying of six databases yielded 1,679 articles, with only 21 remaining after a thorough review. Thrombolysis led to 100% symptom improvement and survival, with 0% mortality. Anticoagulation resulted in symptom improvement and survival in 62.5% of cases, with a 12.5% mortality rate. Catheter-directed and surgical thrombectomy had symptom improvement and survival in 66.7% and 75% of cases, respectively, with no mortality. Conservative management, defined here as management without anticoagulation or thrombolytic therapy, was associated with symptom worsening or no improvement and 50% mortality. This systematic review, based on observational data from case reports, highlights the diverse strategies used by physicians. Proactive and aggressive treatments, especially thrombolysis, show better outcomes and lower mortality rates. However, specific recommendations cannot be made from these results alone, emphasizing the need for well-designed prospective, randomized controlled trials to design structured guidelines for healthcare providers.
Published
Issue
Section
License
Copyright (c) 2025 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.








