Evaluation of the Combined Use of Elastography and Cervicometry With the E-Cervix Index to Predict Second Trimester Preterm Birth Risk
DOI:
https://doi.org/10.14740/jocmr6301Keywords:
Preterm birth, Cervicometry, Cervical elastography, E-Cervix index, Risk prediction, Obstetrics, Cervical assessment, Pregnancy monitoringAbstract
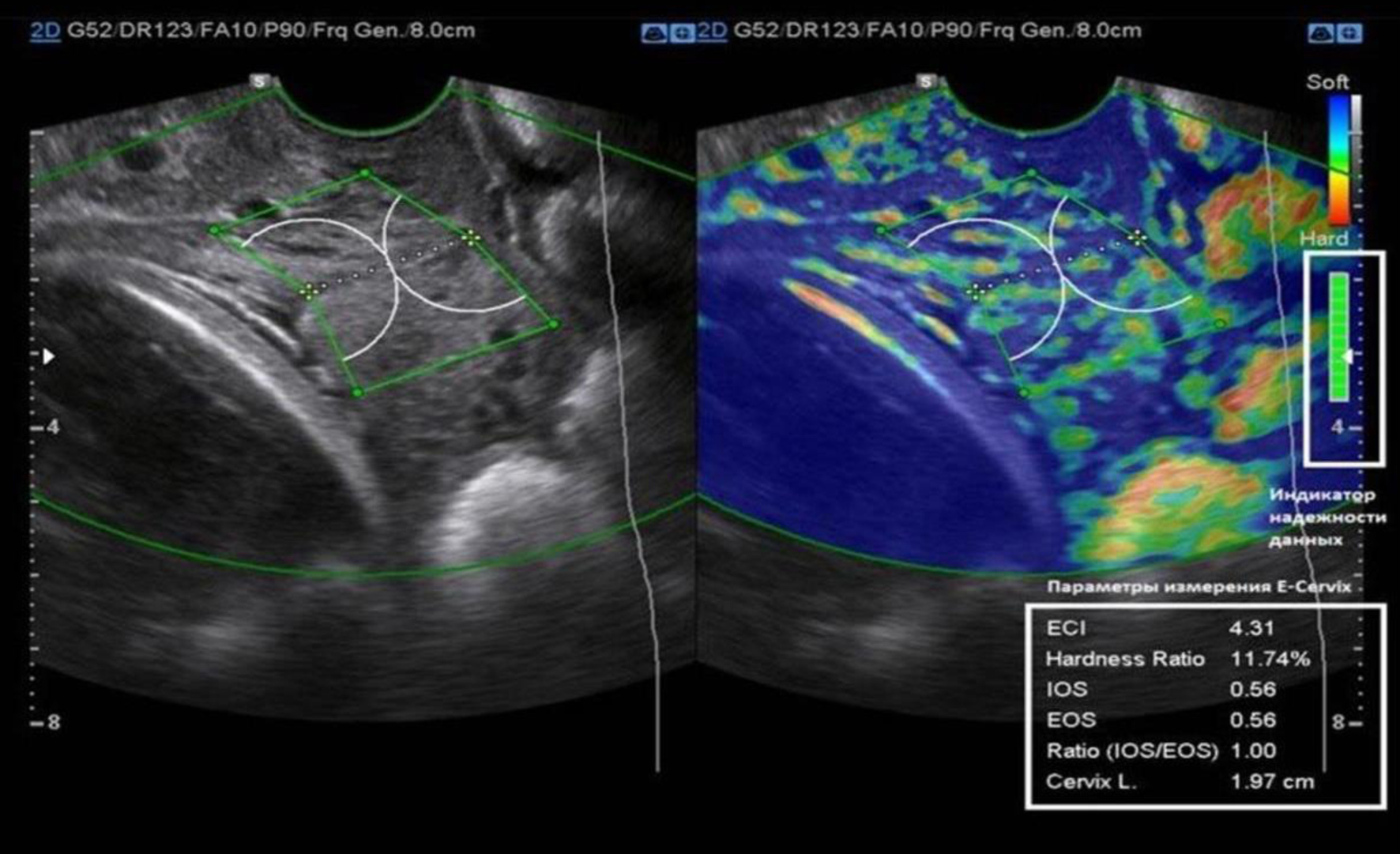
Background: Preterm birth (PB) continues to be a leading cause of neonatal morbidity and mortality, with isthmic-cervical insufficiency (ICI) being among the most serious contributory factors. ICI is often a precursor for PB, and monitoring and diagnosis of this event can largely be achieved through cervicometry and elastography, especially with the use of the E-Cervix index. The aim of this study was to assess the effectiveness of integrating elastography and cervicometry, specifically the E-Cervix index, in predicting PB risk in pregnant women with ICI during the second trimester.
Methods: A prospective cohort study was performed on 250 pregnant women during their second trimester, including 150 women with ICI alongside 100 control women. Cervical elastography was done to assess the stiffness of the cervix coupled with transvaginal ultrasound cervicometry to obtain the length of the cervix. The E-Cervix index was also computed to enhance the discrimination accuracy of lower predictive values. Analysis was done on Statistical Package for the Social Sciences version 27.0 and Statistical Software for Data Analysis version 17.0.
Results: This study investigated the effectiveness of combining cervical elastography and cervicometry, utilizing the E-Cervix index, to assess the risk of PB in pregnant women diagnosed with ICI. The main group (n = 150) had a significantly younger mean age (30.24 ± 5.68 years) compared to the control group (32.17 ± 6.00 years, P = 0.011). Women with ICI showed shorter cervical lengths (2.6 ± 0.5 cm vs. 3.5 ± 0.4 cm, P < 0.001) and higher elasticity contrast index (6.5 ± 1.2 vs. 4.2 ± 0.9, P < 0.001). A significantly higher rate of PB (16% vs. 8%, P = 0.047) was observed in the main group. However, early diagnosis through combined elastography and cervicometry, followed by timely interventions, effectively contributed to a reduction in early PB rates, emphasizing the clinical value of integrated diagnostic approach.
Conclusion: The combined use of elastography and cervicometry, particularly through the E-Cervix index, provides accurate risk assessment for preterm delivery in women with ICI. This approach demonstrates strong diagnostic performance and supports timely clinical decision-making, enhancing early intervention and improving outcomes in high-risk pregnancies.
Published
Issue
Section
License
Copyright (c) 2025 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.








