Predictors of a Paroxysm of Atrial Fibrillation Developing in Patients With Exacerbated Chronic Obstructive Pulmonary Disease
DOI:
https://doi.org/10.14740/jocmr6323Keywords:
Atrial fibrillation, Chronic obstructive pulmonary disease, PredictorsAbstract
Background: Chronic obstructive pulmonary disease (COPD) is a frequent cause of atrial fibrillation (A-fib). A paroxysm of A-fib will protract the patients’ stay at hospital and increase their lethality risk considerably. Despite extensive research done in this field, the predictors of A-fib recurrence in COPD patients have not been definitively studied.
Methods: Our single-institution prospective study involved 569 patients hospitalized for COPD exacerbation. Depending on whether they developed an A-fib paroxysm while in hospital, we divided the patients into two groups: group I (the main one) was composed of 111 COPD patients whose electrocardiogram (ECG) showed an A-fib paroxysm during hospitalization, and group II (the comparison group) comprised 458 COPD patients who had no A-fib paroxysm in their entire hospitalization period. All the patients were given a comprehensive clinical, laboratory, and instrumental examination that included a complete blood count and blood chemistry test, coagulogram, room air oxygen saturation test, external respiration test, standard ECG, echocardiogram, Holter daily ECG monitoring, and a chest computed tomography (CT) scan.
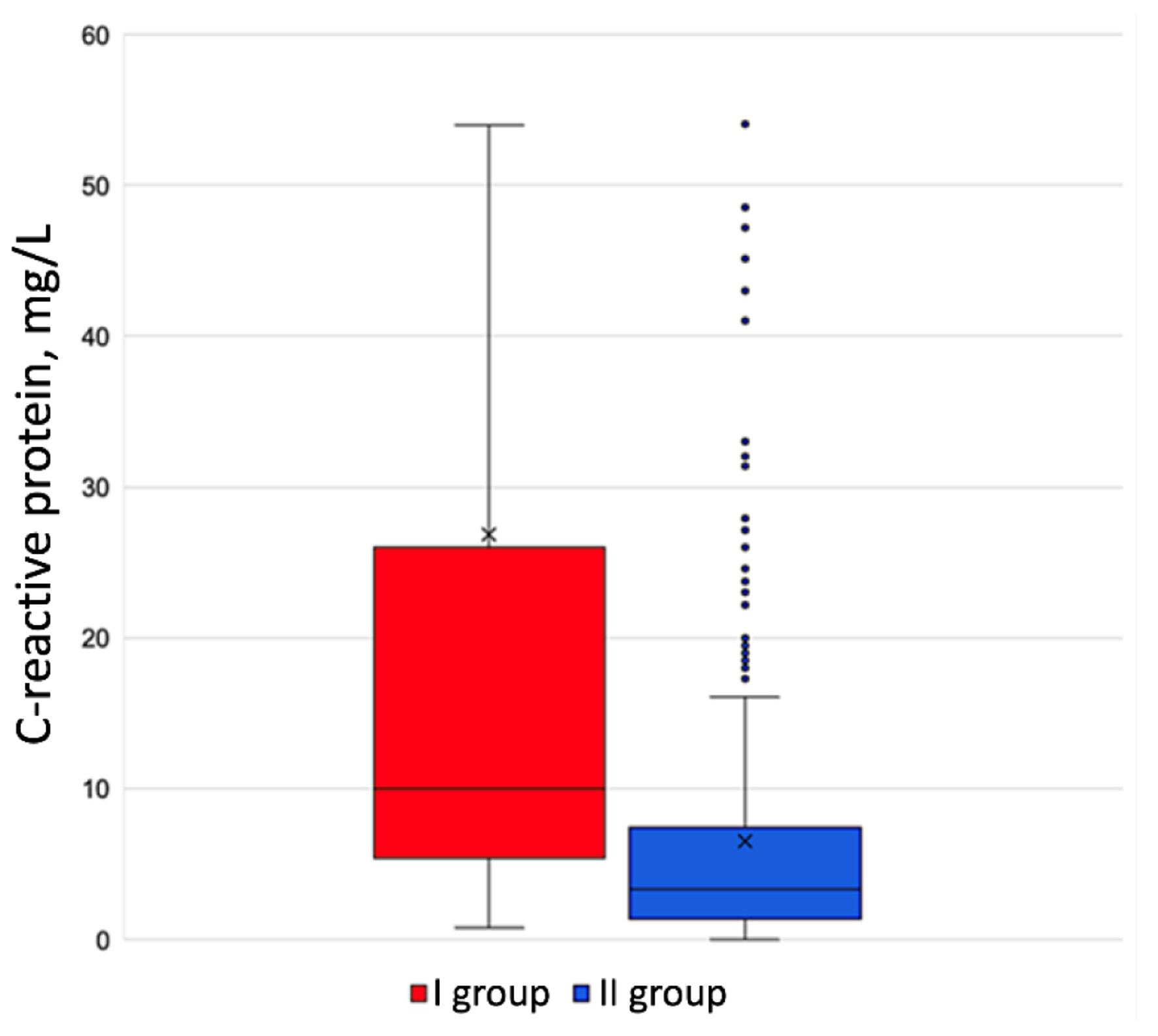
Results: In exacerbated COPD patients, arterial hypertension (AH) would increase their risk of developing an A-fib paroxysm by a factor of 3.74 (confidence interval (CI) 2.78 - 4.19). Arrhythmic patients’ Charlson Comorbidity Index was veritably higher (5 (3 - 6) points) than in the comparison group (3 (2 - 5) points) (P = 0.004). A-fib patients had considerably lower oxygen saturation on room air (SpO2) (91.8% (89-95%)) than non-arrhythmic patients (95.2% (91-97%)). Right atrial area enlargement would increase exacerbated COPD patients’ risk of developing an A-fib paroxysm by a factor of 1.34 (1.16 - 1.56). A-fib patients were found to have a veritably raised level of C-reactive protein to 21.0 mg/L (5.65 - 35.2 mg/L), compared to non-arrhythmic patients with 8.3 mg/L (1.31 - 16.4 mg/L).
Conclusion: The development of an A-fib paroxysm in patients hospitalized for exacerbated COPD is predicted by Charlson Comorbidity Index above 4, right atrial area enlargement, and heightened C-reactive protein.
Published
Issue
Section
License
Copyright (c) 2025 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.








