The Risk of Tuberculosis in Chronic Obstructive Pulmonary Disease Across Different Comorbidities
DOI:
https://doi.org/10.14740/jocmr6345Keywords:
Chronic obstructive pulmonary disease, Comorbidity, Pneumoconiosis, TuberculosisAbstract
Background: Chronic obstructive pulmonary disease (COPD) is a progressive respiratory disorder with significant global morbidity and mortality. COPD is increasingly recognized as a systemic inflammatory condition that predisposes patients to multiple comorbidities, including tuberculosis (TB). There are limited data on how comorbidities in COPD influence the development of TB.
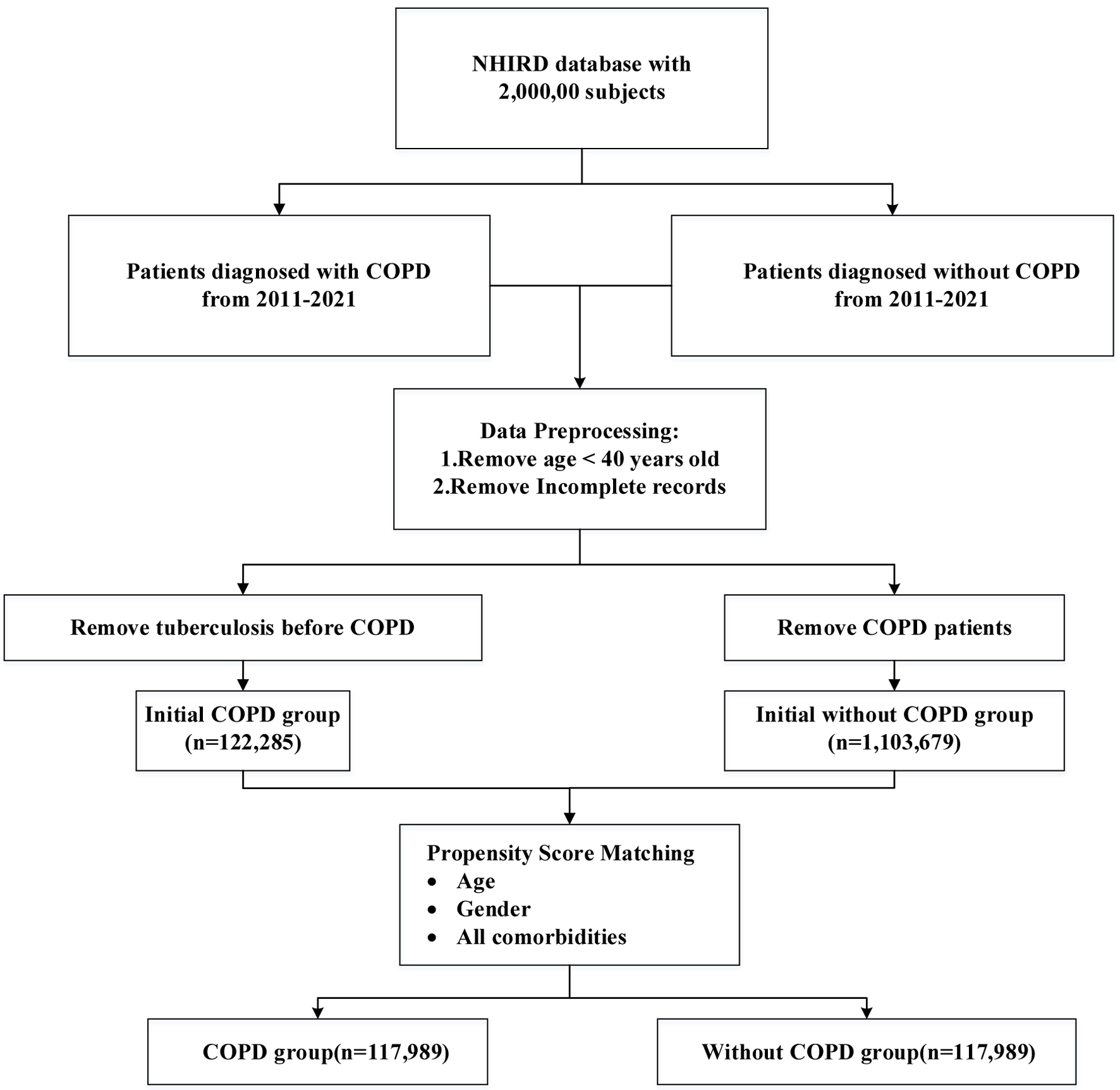
Methods: We conducted a nationwide, retrospective cohort study using data from Taiwan’s National Health Insurance Research Database (NHIRD) between 2011 and 2021. Patients aged ≥ 40 years with a diagnosis of COPD, confirmed by ≥ 3 outpatient visits or ≥ 1 hospitalization, were included. Individuals with prior TB were excluded. Non-COPD controls were matched 1:1 using propensity score matching for demographics and comorbidities. The primary outcome was incident TB (ICD-9-CM 010-018). Cox proportional hazards models were used to estimate adjusted hazard ratios (aHRs) for TB, accounting for a variety of comorbidities.
Results: A total of 117,989 COPD patients and an equal number of matched controls were analyzed. During follow-up, TB incidence was significantly higher in the COPD group (3.20 vs. 1.45 per 10,000 person-years). COPD was associated with a 74% increased risk of TB (aHR 1.74; 95% confidence interval (CI): 1.42 - 2.14; P < 0.001). Stratified analysis demonstrated that TB risk rose progressively with age and was markedly amplified by comorbidities. Notably, pneumoconiosis conferred a nearly sevenfold higher TB risk among COPD patients (aHR 6.94; 95% CI: 2.72 - 17.71; P < 0.001), followed by lung cancer (aHR 1.81; 95% CI: 1.07 - 3.05; P < 0.027) and rheumatoid arthritis (aHR 2.05; 95% CI: 1.01 - 4.12; P < 0.046).
Conclusion: After adjustment for available covariates, COPD was associated with an increased risk of TB; however, residual confounding due to factors such as corticosteroid use, immunosuppressive therapy, and smoking cannot be excluded.
Published
Issue
Section
License
Copyright (c) 2025 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.








