Effectiveness of Short-Acting Oral Antihypertensives in Asymptomatic Markedly Elevated Blood Pressure: An Inverse Probability Treatment Weighted Study
DOI:
https://doi.org/10.14740/jocmr6353Keywords:
Hypertension, Antihypertensive agents, Short-acting, Treatment outcome, Arterial pressure, Propensity scoreAbstract
Background: Although guidelines recommend gradual blood pressure (BP) reduction in asymptomatic markedly elevated BP (AMEBP), short-acting oral antihypertensives are often used despite limited evidence - driven by healthcare providers’ concerns or institutional policies - thereby increasing system burden. This study aimed to identify practical regimens enabling safe, timely discharge and continuity of care.
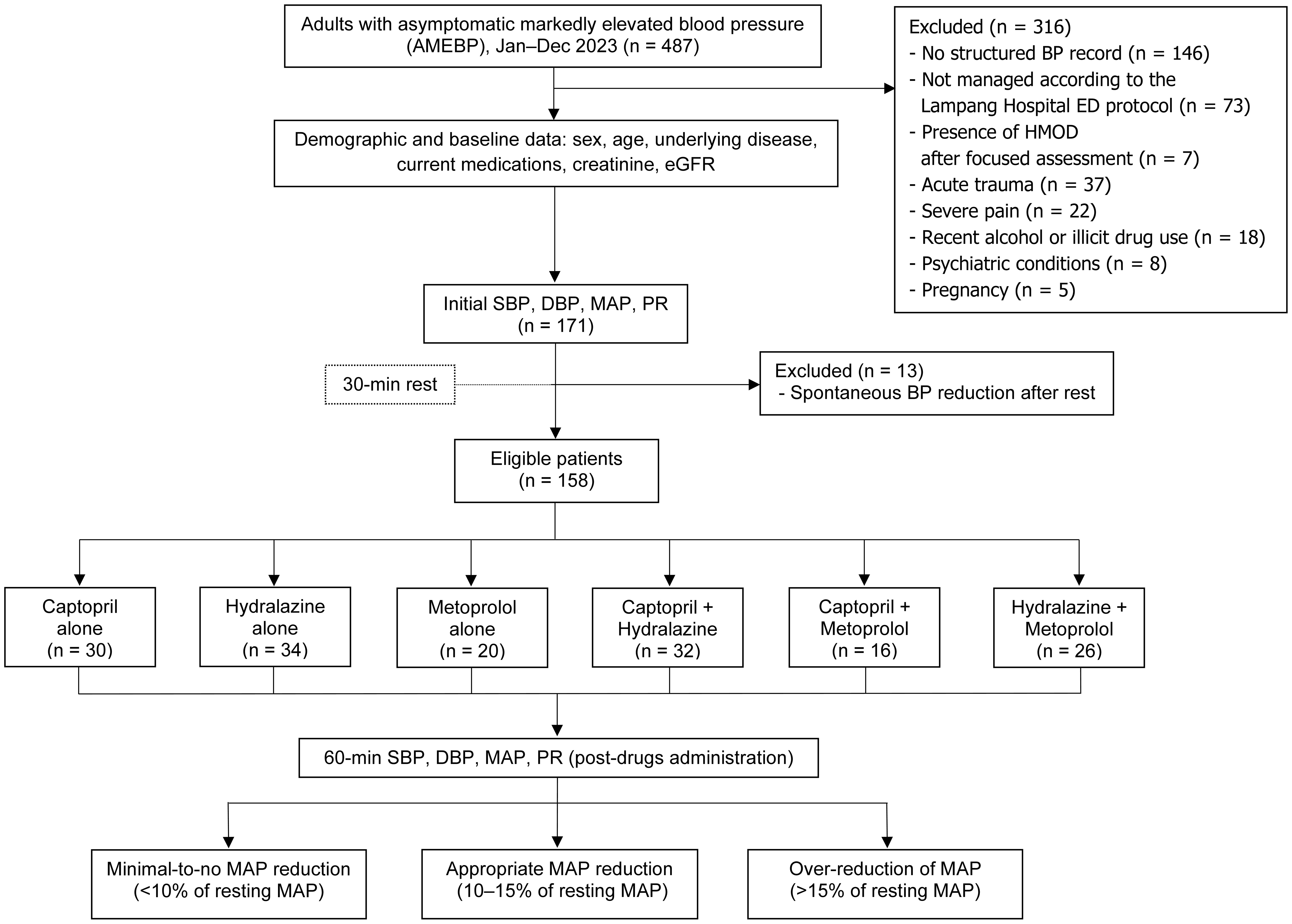
Methods: This retrospective cohort included patients with AMEBP (systolic BP > 180 mm Hg and/or diastolic BP > 110 mm Hg), who presented to the emergency department (ED) of Lampang Hospital between January and December 2023. Oral regimens included captopril, hydralazine, metoprolol (25 mg each), or combinations. The outcome was mean arterial pressure (MAP) reduction within 60 min, classified as no reduction (< 10%), appropriate reduction (10-15%), or over-reduction (> 15%). Inverse probability of treatment weighting (IPTW) adjusted for regimen selection, and multinomial odds ratios (mORs) with 95% confidence intervals (CIs) were reported.
Results: Among 158 patients (mean age 60 years; 67.1% female), baseline MAP was 142.4 ± 16.2 mm Hg. Captopril and hydralazine monotherapy were most likely to achieve appropriate reduction (captopril: mOR: 2.91; 95% CI: 0.96, 8.76; P = 0.058; hydralazine: mOR: 2.76; 95% CI: 0.84, 9.11; P = 0.096). Metoprolol was associated with inappropriate response, while captopril plus hydralazine had highest odds of over-reduction (mOR: 3.04; 95% CI: 1.02, 9.00; P = 0.045).
Conclusions: Although urgent BP reduction is not routinely recommended in the ED, oral captopril appears to be a reasonable first-line option when clinically necessary, while hydralazine may be a suitable alternative. Combination of these two drugs should be used with caution due to the risk of excessive MAP reduction.
Published
Issue
Section
License
Copyright (c) 2025 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.








