Prognostic Value of SIRS, SOFA, qSOFA, and LqSOFA in Emergency Department Sepsis Patients and Correlation of Cytokine Patterns With In-Hospital Mortality
DOI:
https://doi.org/10.14740/jocmr6340Keywords:
Sepsis, Mortality, Cytokines, SOFA, qSOFAAbstract
Background: Several prognostic scores and molecular patterns have been developed to predict increased in-hospital mortality in septic patients. This prospective study aimed to evaluate the prognostic value of systemic inflammatory response syndrome (SIRS), Sequential Organ Failure Assessment (SOFA), quick SOFA (qSOFA), lactate quick SOFA (LqSOFA) and cytokine production levels in emergency department sepsis patients to predict in-hospital mortality.
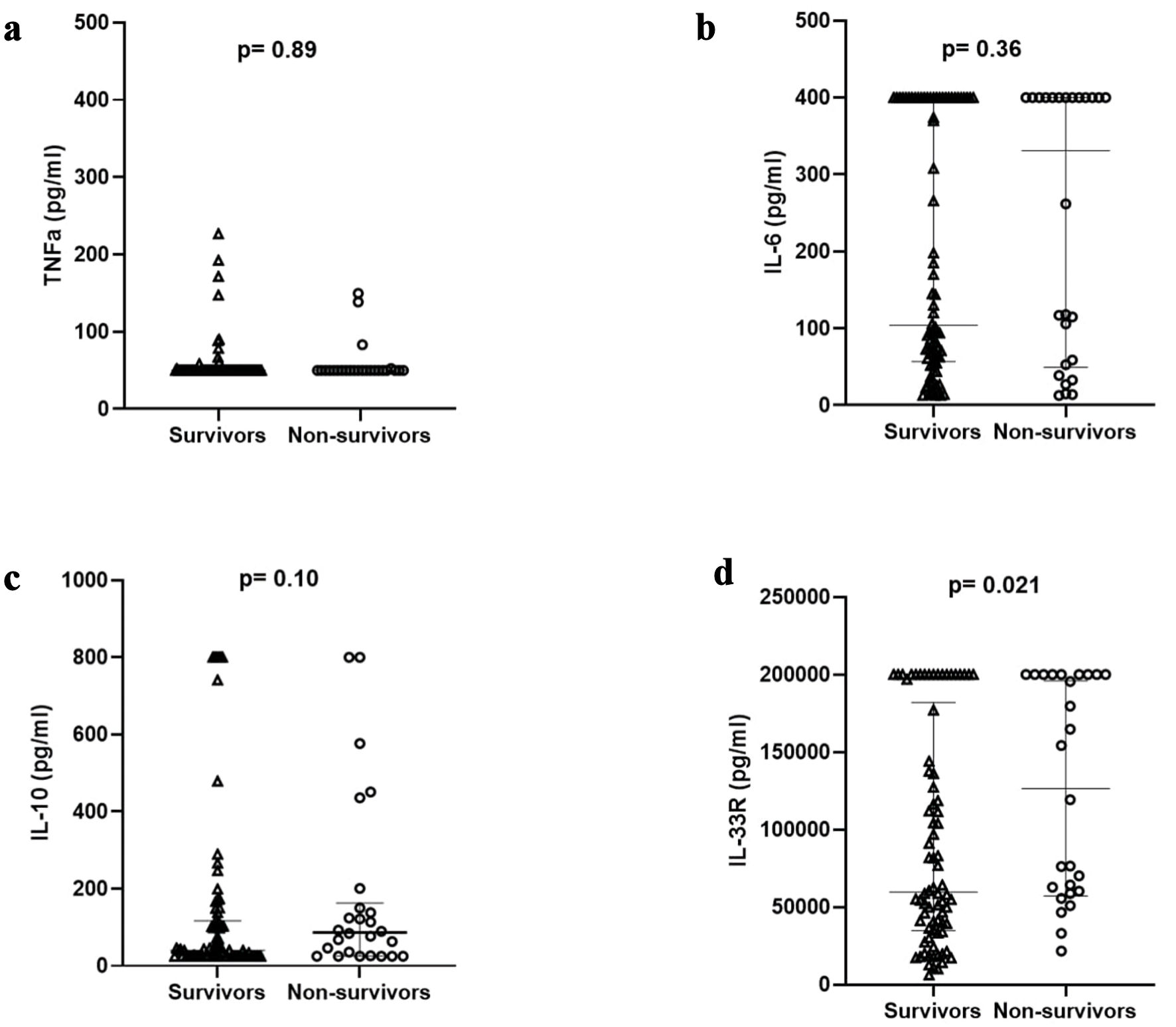
Methods: A total of 106 septic patients were enrolled. Baseline SOFA, SIRS, qSOFA and LqSOFA scores were calculated, and plasma levels of interleukin (IL)-6, IL-10, tumor necrosis factor-α (TNF-α) and interleukin-33 receptor (IL-33R) were measured on admission.
Results: SOFA, qSOFA, LqSOFA scores were significantly lower in sepsis survivors. IL-33R levels were significantly higher in non-survivors (P = 0.021). The best predictive score for sepsis based on the area under the receiver operating characteristic (ROC) curve was qSOFA (0.764, 95% confidence interval (CI) = 0.663 - 0.866), followed by LqSOFA (0.738, 95% CI = 0.63 - 0.845), SOFA (0.713, 95% CI = 0.604 - 0.822) and SIRS (0.603, 95% CI = 0.478 - 0.729). The addition of IL-33R levels (cut-off values > 55,393 pg/mL) to qSOFA and SOFA significantly increased the diagnostic accuracy of both scores with area under the curve (AUC) of 0.78 (95% CI = 0.695 - 0.85) and 0.740 (95% CI = 0.636 - 0.844), respectively. When evaluating early (within 72 h) in-hospital mortality, both IL-10 and IL-33R were significantly higher in non-survivors (124 pg/mL vs. 41 pg/mL in survivors, 195,610 pg/mL vs. 62,767 pg/mL in survivors, respectively). When added to qSOFA and SOFA scores (cut-off levels 74.5 pg/mL and 55,393 pg/mL for IL-10 and IL-33R, respectively), they significantly increased their diagnostic accuracy.
Conclusions: Sepsis prognostic scores were significantly lower in sepsis survivors. IL-10 levels had a significant impact in predicting early (within 72 h) in-hospital mortality and IL-33R levels in predicting both early and total in-hospital mortality, especially when combined with SOFA and qSOFA scores.
Published
Issue
Section
License
Copyright (c) 2025 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.








