Plasma Level of Stromal Cell-Derived Factor-1 Provides Insight Into Statin Response, But Not Into Left Ventricular Dysfunction in New Unstable Angina
DOI:
https://doi.org/10.14740/jocmr6393Keywords:
Statins, Stromal cell-derived factor-1, Unstable anginaAbstract
Background: Stromal cell-derived factor-1 (SDF-1) is a chemokine that regulates atherogenesis, angiogenesis, and multiple physiological processes. Dyslipidemia can contribute to low plasma SDF-1 disturbing its vascular repair functions and elevating cardiovascular risk. Statin therapy is recommended for patients with acute coronary syndrome irrespective of low-density lipoprotein-cholesterol (LDL-C) levels. This study aimed to evaluate the potential associations of plasma SDF-1 levels with LDL-C levels, coronary occlusion-based disease severity, low left ventricular ejection fraction (LVEF) values, and statin therapy in patients with unstable angina (UA).
Methods: Patients with new UA (n = 108) were selected from Coronary Care Unit, King Abdulaziz University Hospital. The exclusion criteria included previous history of myocardial infarction, cardiac valvular problems, myocarditis, liver dysfunction, and recent acute infection. The demographic and clinical features were collected. Disease severity and LVEF values were determined. Plasma SDF-1, LDL-C, and troponin levels were measured.
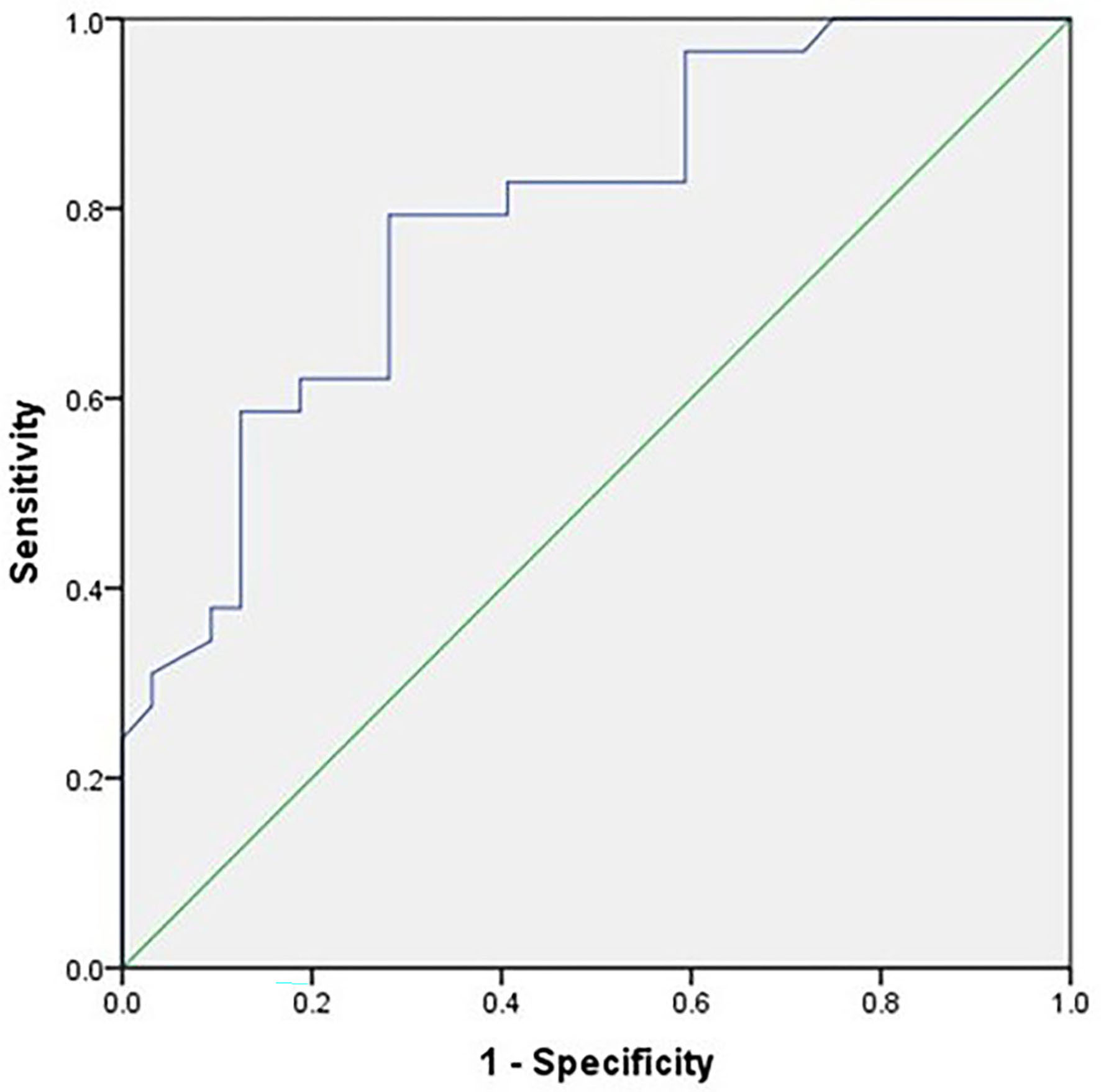
Results: There were poor correlations between plasma SDF-1 level, and sociodemographic features and risk factors except with LDL-C, where it showed a significant correlation. Furthermore, plasma SDF-1 showed non-significant variations with LVEF values and troponin peak levels. In contrast, plasma SDF-1 declined significantly in statin-treated patients, regardless of LDL-C level, compared with those untreated. The receiver operating characteristic (ROC) curve for SDF-1 test showed good accuracy.
Conclusion: In patients with severe UA, plasma SDF-1 level showed significant variations with LDL-C levels and statin therapy suggesting that it can give insight into response to statin therapy regardless of LDL-C level. The ROC analysis showed favorable characteristics suggesting a potential usefulness of plasma SDF-1 assay to discriminate the statin-treated patients from those untreated. This novel approach highlights SDF-1 potential as a biomarker for monitoring statin therapy and predicting risks for adverse events in UA. Furthermore, it could pave the way for longitudinal studies with repeated measurements of plasma SDF-1 to evaluate its role as a prognostic indicator for major adverse cardiovascular events besides the other cardiovascular disease risk factors.
Published
Issue
Section
License
Copyright (c) 2025 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.








