Long-Term Mental Health Evaluation After COVID-19: Insights From the CARDIO COVID 20–21 Registry
DOI:
https://doi.org/10.14740/jocmr6390Keywords:
COVID-19, Long COVID, Depression, Anxiety, Stress, Cognitive dysfunctionAbstract
Background: Psychopathological manifestations are key features of long COVID, contributing to a considerable global mental health burden. Neuropsychiatric sequelae such as anxiety, depression, cognitive dysfunction, and perceived stress may persist for months or years after infection. Latin American populations remain underrepresented, despite a high prevalence of long COVID and unique socio-demographic characteristics. Understanding these impacts is essential for targeted screening and interventions.
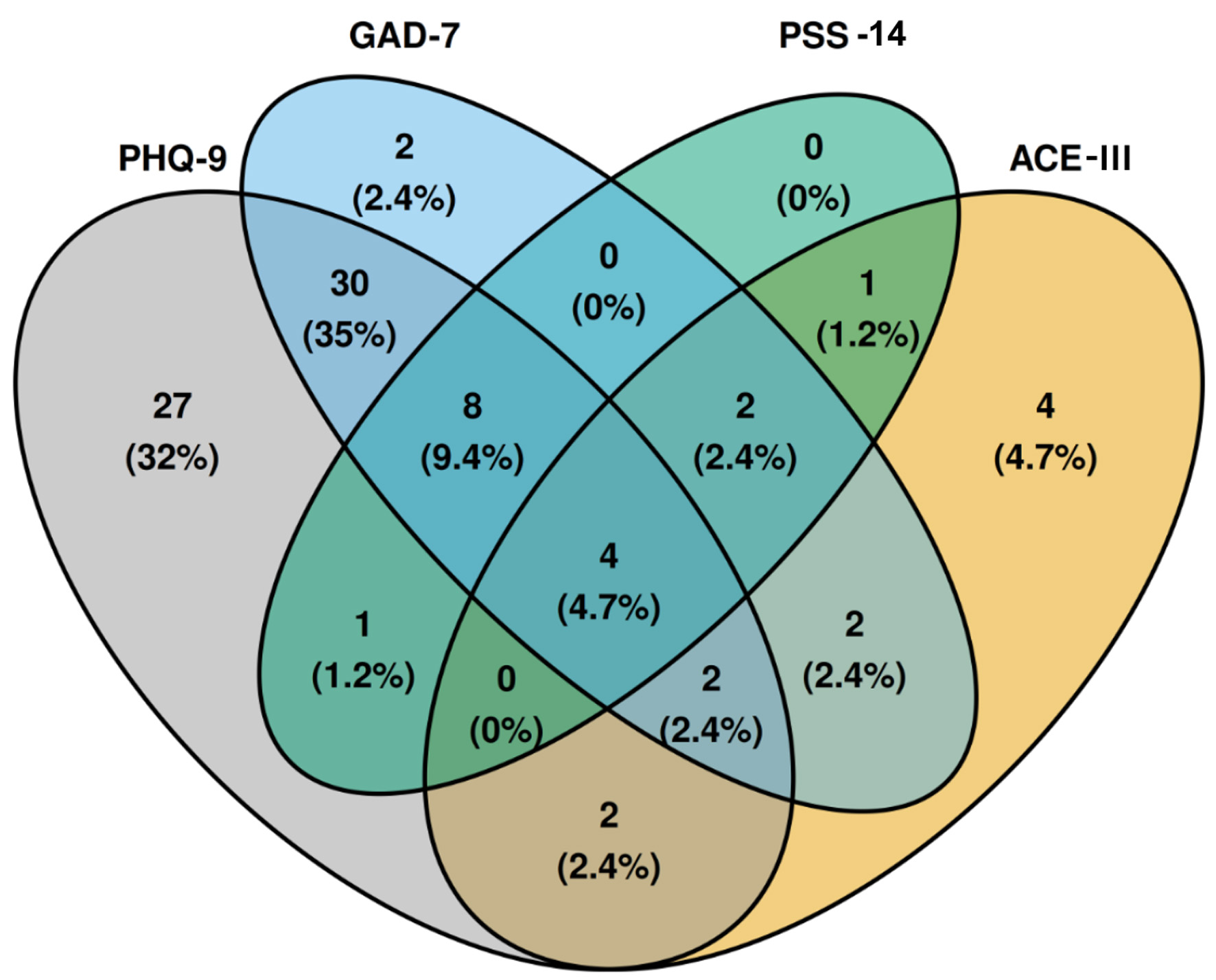
Methods: We conducted a prospective study of patients hospitalized for severe COVID-19. Psychiatric evaluation used the General Anxiety Disorder-7, Patient Health Questionnaire-9, Perceived Stress Scale-14, and Addenbrooke’s Cognitive Examination-III (ACE-III), at an average of 24.5 months post-illness. Bivariate analyses evaluated differences by sex and intensive care unit (ICU) admission. Multivariable linear regression was used to examine associations between cognitive scores and age, sex, education, socioeconomic status, ICU admission, body mass index, smoking exposure, hypertension, and diabetes.
Results: We included 152 patients; the mean age was 56 years, and 58.5% were male. Anxiety symptoms were present in 33%, depression in 49%, and both perceived stress and cognitive dysfunction were each observed in 11% of patients. Women exhibited significantly higher levels of depression (P = 0.02) and stress (P = 0.011), whereas patients admitted to the ICU demonstrated greater cognitive impairment (P < 0.001). In multivariable regression, male sex (P = 0.002), higher education (P < 0.001), and hypertension (P = 0.037) were significantly associated with higher ACE-III scores, while ICU admission was associated with lower scores (P = 0.017).
Conclusion: Our study reveals a high prevalence of mental health symptoms and cognitive dysfunction among patients 2 years after severe COVID-19. Anxiety showed no differences by sex or ICU requirement. Women exhibited higher rates of depression and perceived stress, while ICU admission was associated with poorer cognitive performance. Our findings should encourage systematic screening, diagnosis, and management of long-term neuropsychiatric sequelae in COVID-19 survivors. However, due to the limitations of the single-center design, further longitudinal and multicenter studies are warranted to better elucidate the long-term psychiatric impact of COVID-19.
Published
Issue
Section
License
Copyright (c) 2026 The authors

This work is licensed under a Creative Commons Attribution 4.0 International License.








