Predicting Breast Imaging-Reporting and Data System Classification of Palpable Breast Masses Using Ultrasound to Prioritize Mammography Queues
DOI:
https://doi.org/10.14740/jocmr6409Keywords:
Breast neoplasms, Mammography, Mammary ultrasonography, BI-RADS, Early detection of cancerAbstract
Background: Breast cancer is the leading cause of cancer death in women worldwide. Breast imaging, usually mammography and/or ultrasound, is classified using the Breast Imaging-Reporting and Data System (BI-RADS). At Lampang Hospital, mammography delays of up to 5 months postpone diagnosis in 40% of breast cancer cases. An urgent queue for palpable breast masses was introduced, but nearly half were benign, leading to inefficient prioritization. This study aimed to develop a two-step model based on high-risk ultrasound features and compare it with reference BI-RADS classifications.
Methods: This diagnostic prediction study collected retrospective data from Lampang Hospital between January 2021 and December 2023. Ultrasound images of 390 patients were independently reviewed by radiologists blinded to the reference BI-RADS classification. Stepwise multivariable risk difference regression analysis was applied to identify predictive characteristics from seven predefined ultrasound findings.
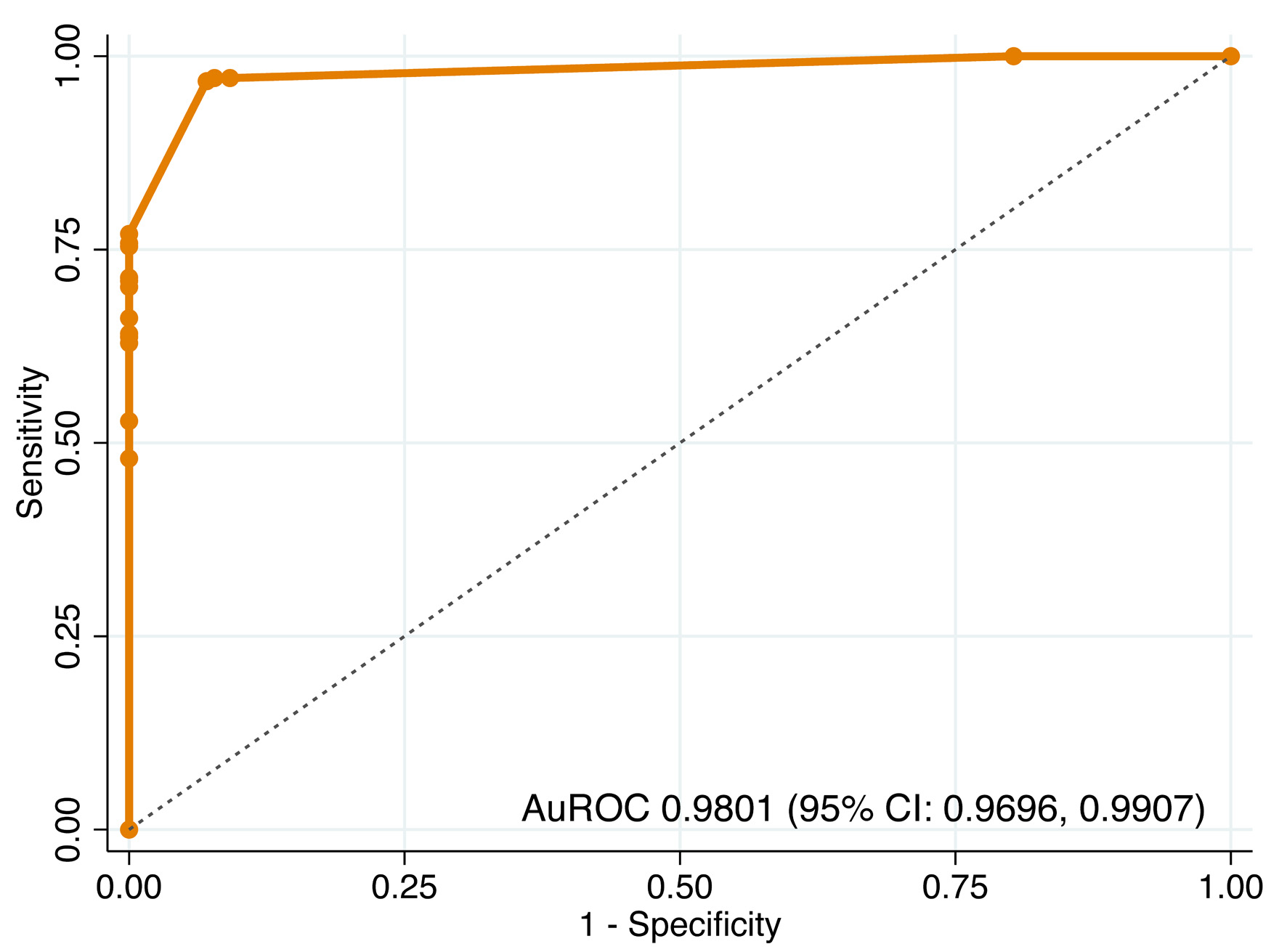
Results: Three predictive characteristics were identified: shape, margin, and echo pattern. The two-step model showed excellent discrimination, with an area under the receiver operating characteristic curve (AuROC) of 0.9801 (95% CI, 0.9696–0.9907) in step 1 and 0.9623 (95% CI, 0.9411–0.9835) in step 2. Internal validation with 200 bootstrap cycles confirmed minimal optimism. Using prevalence-based cut points, the model achieved 88.5% accuracy, with 6.7% underestimation in BI-RADS 4–5 (predicted as 3) and overestimation not exceeding 3% in any category.
Conclusions: A two-step ultrasound-based model using shape, margin, and echo pattern demonstrated excellent discrimination as well as high accuracy, with slightly increased underestimation and minimal overestimation. This re-scheduling strategy optimizes mammography queue prioritization, but external validation is required before clinical implementation.
Published
Issue
Section
License
Copyright (c) 2026 The authors

This work is licensed under a Creative Commons Attribution 4.0 International License.








